Translate this page into:
Unusual presentation of lichen scrofulosorum
Correspondence Address:
Ameet Dandale
Department of Dermatology, LTM Medical College, Sion, Mumbai
India
| How to cite this article: Dandale A, Gupta N, Dhurat R, Ghate S. Unusual presentation of lichen scrofulosorum. Indian J Dermatol Venereol Leprol 2013;79:436-438 |
Sir,
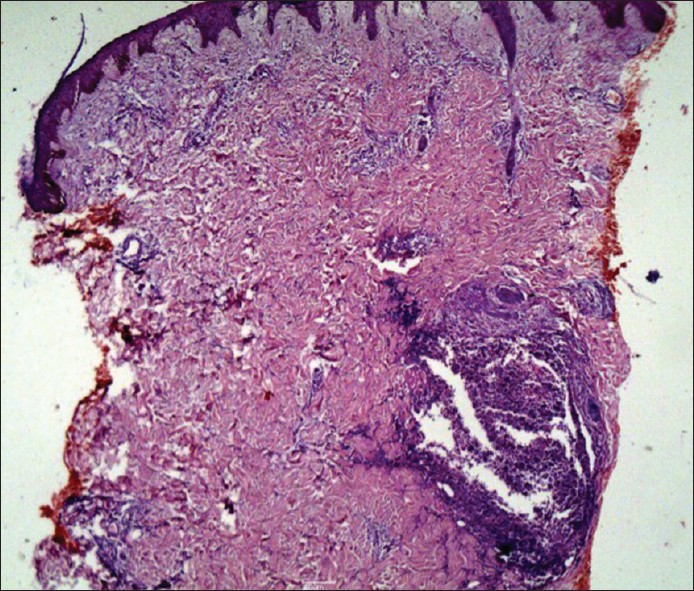
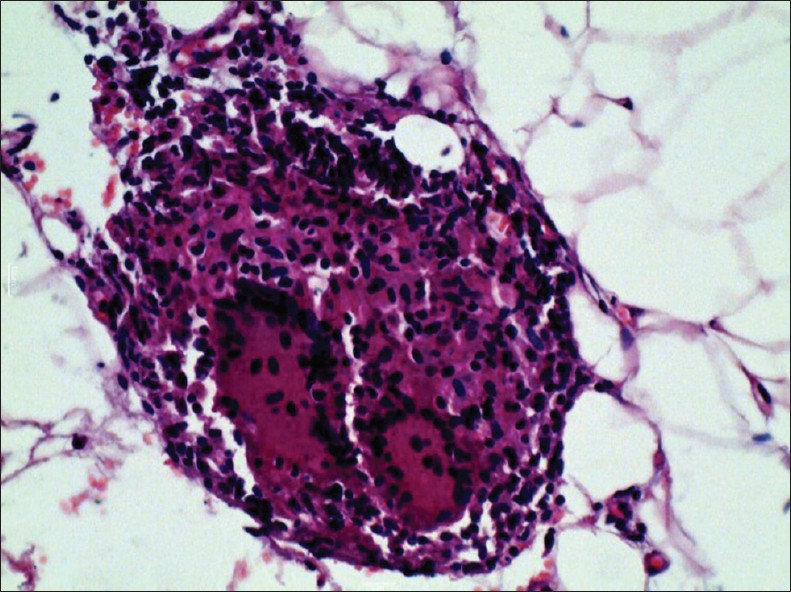
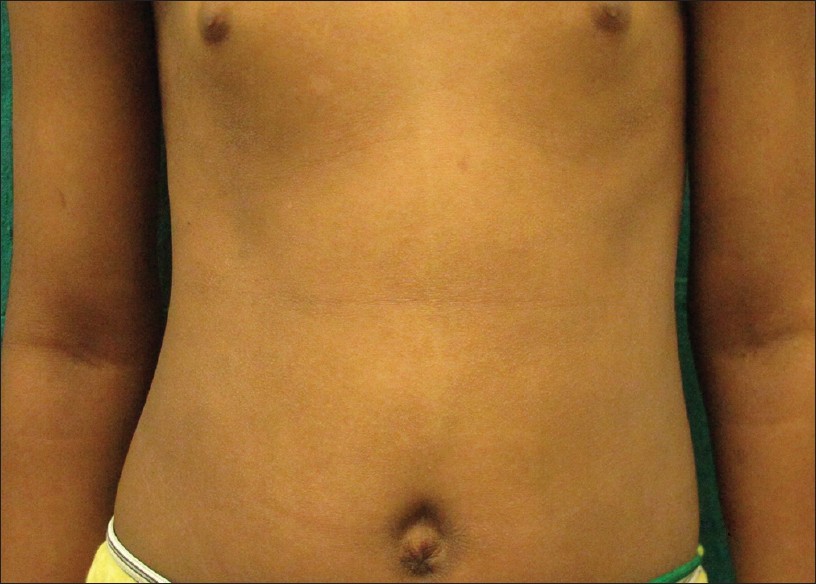
An 8-year-old girl presented with complaints of mildly itchy red-colored tiny lesions over the trunk since 3 months. The patient denied any history of fever, cold and cough, scaling over scalp and extensor aspects, or any history of palmoplantar keratoderma. Cutaneous examination revealed multiple erythematous papules of 1-2 mm in size arranged in an annular pattern forming 3-5 cm plaques associated with mild scaling. The lesions were distributed over the trunk, arms, thighs, and pre-auricular region [Figure - 1]. She was treated with oral anti-histamines and topical emollients. Bacille calmette-guιrin (BCG) vaccination scar was visible on the left deltoid area. Differential diagnosis of follicular psoriasis, pityriasis rubra pilaris, pityriasis rosea, and atopic dermatitis were made. Her hemoglobin level was 10 g%, Erythrocyte sedimentation rate was 50 mm and Mantoux test was 20 mm with blistering. Chest X-ray and ultrasonography of abdomen revealed no abnormality. Human immunodeficiency virus antibodies test and venereal disease research laboratory test were non-reactive. Skin biopsy was done which revealed normal epidermis and infiltrate in upper dermis and around hair follicles forming granulomas with lymphohistiocytic infiltrate and giant cells [Figure - 2] and [Figure - 3]. A diagnosis of lichen scrofulosorum (LS) was made. High-resolution computerized tomography (CT) scan of chest showed lymphadenopathy adjacent to aortic arch, aortopulmonary (AP) window left hilar, subcarinal, and left bronchopulmonary regions along with patchy consolidation in left inferior lingual lobe. CT scan of abdomen showed a calcified splenic granuloma with mild hepatosplenomegaly. Skin tissue was sent for tuberculosis (TB) polymerase chain reaction (PCR) was positive for 123 base pairs (in II amplification round), consistent with positive Mycobacterium tuberculosis infection. The patient was started on isoniazid, 225 mg; rifampicin, 225 mg; pyrazinamide, 750 mg; and ethambutol, 600 mg. Excellent response was noted in 6 weeks in the form of complete subsidence of the lesions with post-inflammatory hyperpigmentation and scaling [Figure - 4].
 |
| Figure 1: Multiple erythematous 2 mm-sized papules arranged in an annular pattern forming 3-5 cm plaques associated with mild scaling over the trunk |
 |
| Figure 2: H and E staining of a skin biopsy showing granulomatous infiltrate around hair follicle (× 100) |
 |
| Figure 3: H and E staining of a skin biopsy showing granulomas with lymphohistiocytic infiltrate and giant cells (×400) |
 |
| Figure 4: After treatment photographs of the patient |
Tuberculides are explained to be a hypersensitivity reaction to M. tuberculosis or its products in a patient with significant immunity. [1] LS is a lichenoid eruption of minute papules ascribed to hematogenous spread of mycobacteria in an individual with strong anti-tuberculous cell-mediated immunity. It is usually associated with strongly positive tuberculin reaction. [1] It has also been observed after BCG vaccination and in association with Mycobacterium avium-intracellulare infections.
LS is found to the second most common form of cutaneous TB, according to recent reports, possibly because of increased incidence of all types of tuberculous infection. Seven percent of cutaneous TB patients were found to have LS in a prospective study in India in 2005. More than 80% cases affected are younger than 16 years of age. [1]
The lesions usually present over trunk as symptomless clusters of firm, typically perifollicular, pink or yellow brown papules of 0.5-3 mm topped by a scale. Lesions persist for months and then spontaneously involute without scarring. Micropustular and noduloulcerative variants have been described. [2] Lesions may coalesce to form annular or discoid plaques. [2] Our case presented with extensive, inflammatory, and scaly plaques resembling psoriasis. Though there is a report of psoriasiform LS dating back to 1911, [2] very few cases of this entity have been reported. [3]
Differential diagnosis includes follicular lichen planus, lichen nitidus, secondary syphilis, lichen spinulosus, keratosis pilaris, sarcoidosis, drug eruptions, and dermatophytid reactions. Histological examination demonstrates superficial non-caseating granulomas around hair follicles and sweat ducts. Mycobacteria are not seen and not be cultured from biopsy material. Specific anti-tuberculous therapy produces complete clearance within 4-8 weeks without scarring. [1]
Main association of LS has been found to be with tuberculous lymph nodes followed by foci in bone. LS can also be associated with other types of cutaneous TB such as scrofuloderma, lupus vulgaris, and erythema induratum. [1] Our patient had no systemic complaints and presented only with skin lesions with mild itching. However, search for internal focus of TB revealed involvement of multiple lymph nodes, lung, liver, and spleen. We also detected M. tuberculosis by PCR in biopsy specimen of LS in our patient. Although in the experience of Tan, et al., polymerase chain reaction (PCR) has not been found to be a useful complement for clinical and histological diagnoses of "paucibacillary" forms of cutaneous TB. [4] Padmavathy et al. reported a case of PCR positivity in LS. [5] This report and our case supports the concept of tuberculids as immunological reactions to degenerate dead bacilli or antigenic fragments thereof that have been deposited in skin and the subcutis. [6] To conclude, such extensive inflammatory form of LS, which is exceedingly rare, should prompt clinicians to search for underlying disseminated internal tuberculous involvement.
| 1. |
Yates VM. Mycobacterial Infections. In: Burns T, Breathnach S, Cox N, Griffith C, editors. Rook's Textbook of Dermatology. 8 th ed. Massachusettes: Wiley-Blackwell; 2010. p. 31.21-22.
th ed. Massachusettes: Wiley-Blackwell; 2010. p. 31.21-22.'>[Google Scholar]
|
| 2. |
Weber FP. Lichen scrofulosorum imitating psoriasis. Proc R Soc Med 1911;4:93.
[Google Scholar]
|
| 3. |
Kumar U, Sethuraman G, Verma P, Das P, Sharma VK. Psoriasiform type of lichen scrofulosorum: Clue to disseminated tuberculosis. Pediatr Dermatol 2011;28:532-4.
[Google Scholar]
|
| 4. |
Tan SH, Tan BH, Goh CL, Tan KC, Tan MF, Ng WC, et al. Detection of Mycobacterium tuberculosis DNA using polymerase chain reaction in cutaneous tuberculosis and tuberculids. Int J Dermatol 1999;38:122-7.
[Google Scholar]
|
| 5. |
Padmavathy L, Rao L, Veliath A. Utility of polymerase chain reaction as a diagnostic tool in cutaneous tuberculosis. Indian J Dermatol Venereol Leprol 2003;69:214-6.
[Google Scholar]
|
| 6. |
Lucas S. Bacterial diseases. In: Lever WF, Schaumberg Lever G, editors. Histopathology of the Skin. 10 th ed. Philadelphia: JB Lippincott; 2009. p. 554.
[Google Scholar]
|
Fulltext Views
5,239
PDF downloads
2,683





