Translate this page into:
Hereditary papulotranslucent acrokeratoderma: A simultaneous presentation in daughter and mother
2 Department of Dermatology, Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, China
Correspondence Address:
Hong Jia
Dermatology Hospital of Institute of Dermatology, Chinese Academy of Medical Sciences, Nanjing, Jiangsu Province - 210 042
China
| How to cite this article: Sun Y, Jia H. Hereditary papulotranslucent acrokeratoderma: A simultaneous presentation in daughter and mother. Indian J Dermatol Venereol Leprol 2013;79:555 |
Sir,
Hereditary papulotranslucent acrokeratoderma (HPA) was first described by Onwukwe et al., in 1973. [1] This disease usually occurs in females during puberty and is characterized by yellowish-white and translucent papules or plaques present on palms and occasionally soles. The disease is inherited through an autosomal-dominant pattern. We report two rare cases among mainland Chinese population, particularly within a family.
A 19-year-old female student and her 45-year-old mother were evaluated for keratotic papules on their both hands. The daughter had symmetrical small pinhead-sized flat papules symmetrically on the thenar area of her palms that began to emerge 13 years ago. These papules gradually developed into plaques. No history of systemic disease was reported on the girl and her mother exhibited same syndrome for more than 20 years. Dermatological examination showed that approximately 2 mm milky-white flat papules were diffusely distributed bilaterally on the wrists and palm margins, parts of which were confluent into plaques, but with none on the feet. These solid papules had a smooth surface, without tenderness. White keratotic plaques appeared on the back of the proximal interphalangeal joint and around the nails [Figure - 1]. The papules turned white after hands were soaked in water, but the number of lesions did not change. Normal color was recovered after approximately half an hour. Pathological examination showed typical epidermal hyperkeratosis with acanthosis and hypergranulosis, as well as slight inflammatory infiltration of superficial dermis without any indication of sweat duct expansion or telangiectasis [Figure - 2]. The mother had dense light-yellowish and translucent papules bilaterally on the wrists and thenar muscle [Figure - 3], without subjective symptoms. Patients in both cases were diagnosed with HPA, which was being treated with topical retinoic ointment twice a day for 3 months, combined with oral administration of acitretin 20 mg once a day for 1 month, followed by acitretin 10 mg once a day for 2 months. After 3 months, significant efficacy was observed and the lesions were flattened.
 |
| Figure 1: Milky-white keratotic plaques on palm margins and around nails |
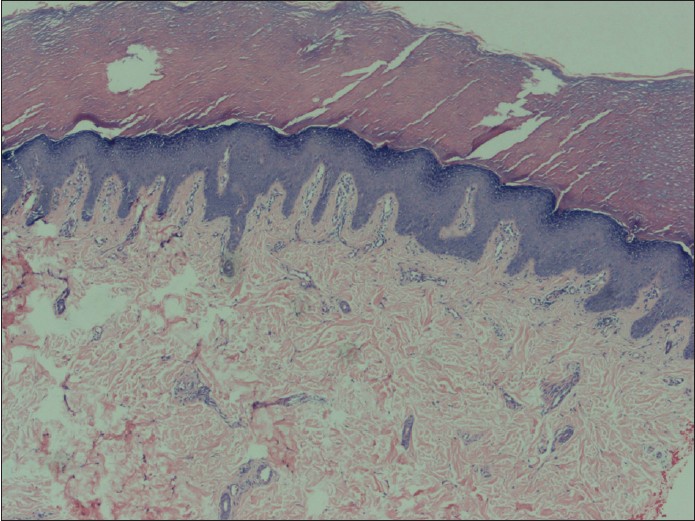 |
| Figure 2: Epidermal hyperkeratosis with acanthosis and hypergranulosis with slight inflammatory infiltration of superficial dermis (H and E, ×40) |
 |
| Figure 3: Typical yellowish-white, translucent, approximately 3 mm papules on the palm margins of both mother and daughter |
Lesions of HPA are usually distributed symmetrically on the back of the joints of both hands, migrating to parts of the palms and the back of the hands, as well as areas under pressure or trauma. Other areas of the body exhibited no such lesion and the hair and nails are healthy. [2] Papules were reported to stop increasing eventually, but existing lesions would not disappear. [3] The pathological section of HPA is characterized neither by cuticle hyperkeratosis without parakeratosis nor inflammatory infiltration of superficial dermis and telangiectasis. Patients with this disease usually present a family history. Heymann [4] reported an HPA patient whose brother and niece had the same lesions.
The pathogenesis of HPA remains unknown. The lesions are considered a subtype of hereditary palmoplantar keratodermas and are similar to aquagenic acrokeratoderma (AAK). AAK is considered a variant of HPA in some papers, whereas others define AAK and HPA as different types of acrokeratoderma. [3] HPA is often associated with atopic diathesis, sparse hair, and persistent translucent yellow-white papules. This disease should be distinguished from other kinds of keratinization, such as punctate palmoplantar keratoderma, epidermodysplasia verruciformis, cutaneous amyloidosis, knuckle pads, jelly-like miliary rash, and so on. There are also researchers who call such keratinization on margin of hands and feet, collectively, as marginal papular acrokeratoderma, which are divided into inherited and acquired, in which HPA is classified as the former. [5]
HPA treatment is mainly topical and often involves exfoliation agents such as ammonium lactate cream 12%. [3] Topical salicylic acid 5% and retinoic acid ointment, as well as oral administration of vitamin A and vitamin E can also be employed, although efficacy is yet to be confirmed. The treatment for the two given cases include topical retinoic acid ointment 0.05% combined with oral administration of acitretin for 3 months. Significant efficacy was observed after 3 months of treatment. However, patients require further follow- up.
| 1. |
Onwukwe MF, Mihm MC Jr, Toda K. Hereditary papulotranslucent acrokeratoderma: A new variant of familial punctate keratoderma? Arch Dermatol 1973;108:108-10.
[Google Scholar]
|
| 2. |
Zhao YK, Luo YD. Aquagenic keratoderma. Chin J Dermatol 2009;42:514-5.
[Google Scholar]
|
| 3. |
Sracic JK, Krishnan RS, Nunez-Gussman JK, Orengo IF, Hsu S. Hereditary papulotranslucent acrokeratoderma: a case report and literature review. Dermatol Online J 2005;11:17.
[Google Scholar]
|
| 4. |
Heymann WR. Hereditary papulotranslucent acrokeratoderma.Cutis1998;61:29-30.
[Google Scholar]
|
| 5. |
Rongioletti F, Betti R, Crosti C, Rebora A. Marginal papular acrokeratodermas: A unified nosography for focal acral hyperkeratosis, acrokeratoelastoidosis and related disorders. Dermatology1994;188:28-31.
[Google Scholar]
|
Fulltext Views
3,213
PDF downloads
1,851





