Translate this page into:
Acitretin in dermatology
Correspondence Address:
Rashmi Sarkar
Department of Dermatology, Maulana Azad Medical College, New Delhi - 110 092
India
| How to cite this article: Sarkar R, Chugh S, Garg VK. Acitretin in dermatology. Indian J Dermatol Venereol Leprol 2013;79:759-771 |
Abstract
Acitretin, a synthetic retinoid has gradually replaced etretinate in today's dermatologic practice because of its more favorable pharmacokinetics. Acitretin over the past 20 years has proven useful in a number of difficult-to-treat hyperkeratotic and inflammatory dermatoses and nonmelanoma skin cancers. It is effective both as monotherapy and in combination with other drugs for hyperkeratotic disorders. It is considered to be an established second line treatment for psoriasis and exerts its effect mainly due to its antikeratinizing, antiinflammatory, and antiproliferative effect. Its antineoplastic properties make it a useful agent for cancer prophylaxis. Evidence-based efficacy, side-effect profile, and approach to the use of acitretin would be discussed in this review. In addition to its approved uses, the various off label uses will also be highlighted in this section. Since its use is limited by its teratogenic potential and other adverse effects, including mucocutaneous effects and hepatotoxicity, this review would summarize the contraindications and precautions to be exercised before prescribing acitretin.Introduction
The skin absorbs, stores, and metabolizes vitamin A. Retinoids influence cellular division and differentiation of stratified structures of the epidermis. Many of the physiological responses of the skin, such as dermal aging, immune defense, and wound healing are significantly affected by retinoids. Interest in the effects of retinol, retinyl palmitate, and other retinoids on skin is a subject for continued investigation. Synthetic retinoids are classified into three generations including nonaromatic, monoaromatic, and polyaromatic compounds.
- First generation retinoids: Which include retinol, retinal, tretinoin (retinoic acid, Retin-A), isotretinoin, and alitretinoin.
- Second generation retinoids: Which include etretinate and acitretin.
- Third generation retinoids: Which include tazarotene, bexarotene, and adapalene.
Pharmacokinetics
Acitretin is rapidly and extensively distributed throughout the body bound to plasma proteins without tissue accumulation. It is metabolized mainly in the liver into 13-cisisoacitretin, which is excreted both in urine and feces. [1],[2],[3] Its bioavailablity is increased by intake with fatty food. [4] As studied in human hepatocyte cultures, alcohol indirectly increases the conversion of acitretin to etretinate by acting as a catalyst for hepatic enzymes, a process known as reverse esterification. [1],[5] The mechanism of the metabolic process for conversion of acitretin to etretinate has not been fully defined and whether substances other than ethanol are associated with transesterification is not clear. In a study by Gronhoj et al., on 86 patients on acitretin, a trend linking higher risk of etretinate formation with higher dose of alcohol consumption was found (all 16 patients with average >200 g/week alcohol intake having detectable etretinate). As etretinate is more lipid-soluble and has longer T1/2, it is especially important for pregnant females to avoid alcohol intake during pregnancy and for 2 months after discontinuation of acitretin therapy.
Mechanism of Action
Acitretin acts at cytosolic proteins and intranuclear receptors, which are part of the steroid-thyroid hormone super family. The metabolites of acitretin bind to retinoic acid receptors (RARs), which lead to alteration of gene transcription through response elements, leading to antiproliferative and antiinflammatory effects. In psoriasis and other disorders of keratinization, acitretin normalizes epidermal cell proliferation, differentiation, and cornification. [2],[3],[6],[7]
- Acitretin stimulates differentiation and normalizes accelerated epidermopoiesis of pathological epidermis
- It decreases release of leucotrienes and dihydroeicosatetraenoic acid products and inhibits neutrophil chemotaxis into the epidermis. It also interferes with the esterification and incorporation of arachidonic acid into nonphosphorus lipids in human keratinocytes and causes inhibition of ornithine decarboxylase thus decreasing the synthesis of polyamines. It also inhibits keratinocyte production of vascular endothelial growth factor.
- It inhibits cell growth and proliferation and decreases AMP-dependent protein kinases in fibroblasts.
- Antineoplastic effects: By normalizing abnormal epidermopoesis acitretin exerts its anticarcinogenic effects. It also inhibits tumor cell angiogenesis and modulates cellular apoptosis. Retinoids influence growth factors, can indirectly down-regulate proto-oncogenes and may act to increase intracellular levels of ceramides. These changes may lead to decrease in cell growth and possibly inhibit malignant progression
- Wound healing: Retinoids lead to increased mucopolysaccharides, collagen, and fibronectin synthesis and decrease in collagenase production interfere with wound healing
- Antiacne and sebum effects: Caused by inhibition of sebocyte proliferation although the potency of acitretin (27.5%) is much lower than isotretinoin (48.2%).
Psoriasis
The effect is dose dependant. A total of seven studies, (level of evidence of 3), showed partial remission (PASI 75) in 25-75% of the patients, in doses of 30-40 mg daily. [7],[8],[9],[10],[11] In a study by Gupta et al. with 24 patients, daily treatment with acitretin 10 or 25 mg did not lead to any improvement in skin lesions, whereas daily doses of 50 and 75 mg resulted in an improvement of at least 75% in 25% of the patients with psoriasis. [12] Acitretin is licensed for use in severe extensive psoriasis, which is resistant to other forms of therapy, including topical, light and systemic and palmoplantar pustular psoriasis. [13] An initial worsening of psoriasis symptoms is sometimes seen at the beginning of the treatment period.
- Generalized pustular psoriasis: In a study on 385 patients of generalized pustular psoriasis retinoid therapy was effective in 84% of patients, methotrexate in 76%, and cyclosporine in 71%, making retinoids the choice of drug in generalized pustular psoriasis [14]
- Palmoplantar pustulosis: In two randomized controlled trials (RCTs) Expand comparing acitretin with placebo in palmoplantar pustulosis, acitretin was significantly more effective than placebo, acting within 4 weeks to produce a 5-fold reduction in pustules. [15] In the study by Lassus and Geiger, comparing acitretin and etretinate there was a 10-fold reduction in pustules after 12 weeks of therapy, however, the difference in the efficacy of two drugs was not significant. [14]
- Erythrodermic psoriasis: As monotherapy, acitretin has been shown to be effective in treating erythrodermic psoriasis.
- Severe plaque type psoriasis: The efficacy of acitretin in chronic plaque psoriasis as a monotherapy is below methotrexate and cyclosporine. However, when used in combination with other topical and systemic therapies (topical corticosteroids, topical vitamin D preparations, psoralen with UVA (PUVA, ultraviolet B (UVB) therapy) it is as potent as classical therapies.
- Nail psoriasis: In an open study of 396 patients with nail psoriasis who received acitretin in doses of 0.2-0.3 mg/kg daily for 6 months, the mean improvement in Nail Psoriasis Severity Index was 41% and 25% of patients cleared completely or almost cleared. [16]
- Psoriasis associated with human immunodeficiency virus (HIV) infection: Acitretin is the only drug in antipsoriatic armarium that does not appear to have immunosuppressive properties and hence can be used even in HIV and immunosuppressed patients.
A recent systematic review of efficacy of oral retinoids as single agent or combined therapy in plaque-type psoriasis (PV), nail psoriasis and localized and generalized pustular psoriasis: Initial and optimal dosage; was compiled by Sbidian et al. [17] Out of the 44 RCTs studied in most of the studies, starting daily dosages were between 10 and 25 mg and stepwise escalation was associated with higher clinical efficacy and lower incidence of adverse events in comparison with higher doses and regimens rapidly reaching optimal dose. Retinoids as single agent therapy appeared to show limited efficacy in PV, whereas good clinical efficacy was reported in pustular forms, which may, however, spontaneously remit. Retinoids in combination with phototherapy were highly effective.
In the comparative studies with etretinate there was a trend for acitretin to be slightly less effective and to present a higher incidence of similar side-effects. In an 8-week trial in 175 patients acitretin at 10, 25, and 50 mg daily produced a 50% improvement in psoriasis in 50%, 40.5%, and 54%, respectively, compared with 61% with etretinate. [18] Side-effects, like efficacy, were dose related as found by Pearce et al., where common adverse events (deranged liver enzymes and lipid profile) were two to three times more frequent in patients receiving 50 mg daily compared with patients receiving 25 mg daily. [19]
Optimal dosing
In a randomized double-blind study by Dogra et al., 61 patients of severe plaque psoriasis were divided into three groups to receive acitretin in doses of 25, 35, and 50 mg per day for 12 weeks. After 12 weeks the percentage reduction in the PASI score was 54%, 76%, and 54% and PASI 75 was achieved in 47%, 69%, and 53% patients in 25, 35, and 50 acitretin mg/day groups, respectively. The majority of adverse events were mucocutaneous, mild-to-moderate severity, and dose dependent. Thus 35 mg dosing appeared to be most efficacious and safe for psoriasis patients. [20]
There is evidence to support that low doses of acitretin has reduced adverse events but still maintains efficacy. Retrospective analysis of data from two large randomized trials, which had an 8-week, double-blinded (DB), placebo-controlled phase followed by a 16-week open-label (OL) phase was done by Haushalter et al. [21] During the DB phase, patients received placebo, 10, 25, 50, or 75 mg of acitretin daily. During the OL phase, patients received either high-dose treatment of approximately 50 mg/day or low-dose of 25 mg/day. At the end of the OL phase (24 weeks), treatment success rates were similar among all groups (29-33%) with highest rates in the group receiving low-dose treatment for both DB and OL phases (47% success). Decrease in bovine serum albumin (BSA) was also highest in this group (73% vs. 28-54%). Thus, individualization of acitretin dosing is crucial to minimize side effects and improving adherence and efficacy. This analysis supports the utility of low-dose acitretin for psoriasis over extended treatment periods.
Combination Therapy
Acitretin and PUVA: The major advantage of this combination is reduced risk of malignancy by phototherapy especially squamous cell carcinoma. Four RCTs compared acitretin and PUVA (rePUVA) with placebo and PUVA, and showed acitretin-PUVA combination to be more effective than PUVA alone, reducing the number of PUVA treatments, exposure to UVA and the clinical scores. [11],[13] In a randomized, double-blind comparative study of 48 patients with severe, widespread psoriasis treated either with photochemotherapy (PUVA) alone or combination with acitretin, marked or complete clearing of psoriasis occurred in 80% of the patients (20 of 25) without acitretin and in 96% of the patients (22 of 23) with adjunctive acitretin administration. The mean cumulative UVA dose given to patients in the acitretin-PUVA group was 42% less than that required for patients in the placebo-PUVA group.
Acitretin and ultraviolet B
Studies comparing acitretin in combination with UVB versus UVB alone found better outcomes and sparing of UVB with acitretin-UVB in combination than with UVB alone. [13] Clearance occurred in 89% treated with acitretin-UVB (ReUVB) versus (62.5%) patients given UVB alone. The improvement score was significantly higher for the ReUVB side than the acitretin side. Patients treated with ReUVB showed a statistically higher therapeutic score (95-100% clearance) than those receiving UVB alone. In a recent RCT acitretin and UVB cleared 55.6% of patients compared with 63.3% treated with acitretin and PUVA. [22]
Acitretin and calcipotriol ointment
RCTs combining acitretin with calcipotriol ointment showed additive benefits of the combination with 67% patients showing clearance as compared with 41% with acitretin alone. In another study comparing the combination with acitretin montherapy, the number of patients with complete clearance increased from 15% to 40% after 12 weeks [23] (P < 0.05). After 52 weeks, 60% and 40% in the combination and acitretin monotherapy group, respectively, achieved complete clearance. The duration of treatment and total dose of retinoids required to achieve clearance were slightly lower in the combination group, however, this was not statistically significant.
Other combinations
A RCT showed similar efficacy from the combination regimen of acitretin 0.4 mg/kg daily and etanercept 25 mg once weekly to that observed with etanercept 25 mg twice weekly thus proving etanercept-sparing effect of acitretin. [24]
The combination of methotrexate and acitretin has been used in patients with severe psoriasis, where all other treatments have failed. Although this combination can be very effective, sporadic severe hepatotoxic responses have been reported. [25]
The efficacy of concomitant use of acitretin with ciclosporin is not convincing as this combination can lead to ciclosporin toxicity as both drugs are inactivated by the same cytochrome P-450 system. [26]
In a randomized double-blind placebo controlled trial by Mittal et al., on 41 patients with psoriasis, 19 patients received combination of acitretin and pioglitazone while 22 received placebo with acitretin. After 12 weeks of therapy percentage reduction in PASI score was 64.2% in the acitretin plus pioglitazone group and 51.7% in the acitretin plus placebo group with minimal adverse events in both the groups. Thus, pioglitazone may have potential antipsoriatic effect and provide a convenient, efficacious, and relatively safe option to combine with acitretin.
Other Uses
Darier′s disease
The results of multiple trials studying efficacy of acitretin and comparing with etretinate in Darier′s disease have shown marked improvement or remission in most of the cases even at low doses [27] (10-25 mg) and no significant difference in either of the two drugs. [28]
Pityriasis rubra pilaris
Isotretinoin is a first line therapy for pityriasis rubra pilaris, however, not so successful results have been reported for acitretin. There are individual case reports of success of acitretin therapy with UVB and UVA1 therapy in Pityriasis rubra pilaris (PRP) patients. [29]
Lichen planus
In a RCT in severe lichen planus, Laurberg et al., showed marked improvement in 64% of patients on acitretin 30 mg daily vs. 13% on placebo. [30] In a meta-analysis by Cribier et al., which included six studies with 86 patients with oral LP treated with etretinate, significant improvement occurred with etretinate over placebo. [31] Thus acitretin is favored as first-line therapy in cutaneous lichen planus. Acitretin may also be preferred in the hyperkeratotic variant of lichen planus for its modulating effect on keratinization. Jaime et al., reported a case of exuberant hypertrophic lichen planus involving palms and soles responding to acitretin with excellent response after 9 months of therapy. [32]
Lupus erythematosus
In an RCT of 58 patients comparing acitretin 50 mg daily with hydroxychloroquine 400 mg daily for 8 weeks, improvement was found in 46% and 50%, respectively, but drop outs were more frequent in the acitretin group because of side-effects. [33] In another open trial, 15 out of 20 subjects achieved total clearance or marked reduction in all lesions. Acitretin was found to be superior to previous therapy with antimalarials and/or systemic corticosteroids in most of the patients with subacute cutaneous lupus erythematosus who showed complete clearing of their lesions within 2-4 weeks. [34] Even in verrucous lesions of lupus it may have an edge over other agents as it modulates hyperkeratosis.
Lichen sclerosus
In a randomized controlled trial on 46 subjects, 14 of 22 patients on acitretin responded as compared to 6 of 24 in the placebo group. However, there was a high dropout rate in this study. [35]
Icthyosis and keratodermas
Acitretin has been found to be useful in severe forms of the ichthyoses based on numerous clinical trials both in pediatric [36] and adult population. [37] These include lamellar ichthyosis, X linked icthyosis, bullous, and nonbullous ichthyosiform erythroderma and Sjogren-Larsson syndrome. In these trials most patients have showed marked improvement or remission while on therapy. [38] Among the palmoplantar keratodermas, Vohwinkel syndrome, keratitis-ichthyosis-deafness (KID) syndrome, hereditary punctate palmoplantar keratoderma, type I hereditary punctate keratoderma, epidermolytic hyperkeratosis, and Papillon-Lefevre syndrome have all been reported as successfully treated with acitretin in small series. [39],[40],[41] However, treatment of epidermolytic palmoplantar keratoderma may result in large erosions and worsening may occur in Netherton syndrome. [37] Acitretin has been reported to cause 51% reduction in hyperkeratotic hand eczema in one RCT of 29 patients. [42]
Other conditions
These are some of the off label indications of acitretin [Table - 1].
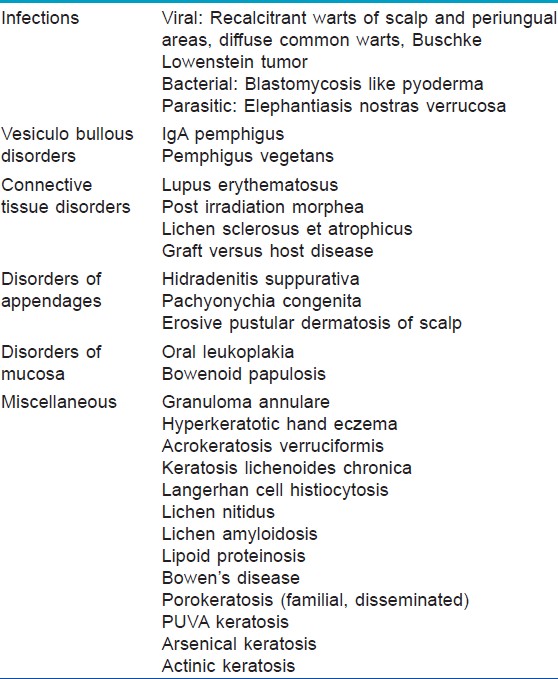
Infections
Acitretin has also been found useful in the management of recalcitrant warts in numerous case reports, [43] especially involving difficult to treat sites, for example, scalp and periungual areas. [44] An open study of etretinate in children with severe warts showed clearance in 16 of 20 patients, however, in 4 patients there was relapse on stopping therapy. [45] Acitretin has been used as an adjunct to imiquimod therapy and excision in giant condyloma acuminata. [46]
In another case report acitretin improved clinical lesions of blastomycosis like pyoderma resistant to all conventional therapies within 3 months of starting treatment and there was nonrecurrence until 9 months of stopping therapy. [47]
Acitretin has been reported to cause improvement with almost complete clearing in cutaneous lesions of a 64-year-old case of elephantiaisis nostras verrucosa (nonfilarial in origin) with coexisting erythrodermic psoriasis.
Acitretin may also be proposed as a management option for morphoea, post irradiation, as suggested in a case report of a 43-year-old patient of morphoea treated with low dose acitretin and UV therapy. [48] There was subjective improvement in pain as well as objective improvement in degree of induration. It may also be useful in immunobullous disorders, for example, subcorneal pustular dermatosis (SCPD) type of IgA pemphigus. In a case report of a patient with SCPD type of IgA pemphigus resistant to all modalities acitretin along with dapsone was found to cause clinical improvement. [49] A recent case report of a 57-year-old patient of Langerhans cell histiocytosis treated with one year of acitretin showed complete clearance of cutaneous lesions even at one year of follow-up. Presumably the action is attributed to the immunomodulator properties of acitretin on Langerhan cells. [50]
In a questionnaire-based retrospective cross-sectional survey by Gruber et al. conducted on 30 patients of Pachyonychia congenita the efficacy and side effects of oral retinoids (10-50 mg/day for 1-240 months) were assessed. [51] Overall, 30 patients were treated of which 12 patients received acitretin and 14 received isotretinoin. The therapy was effective in 58% and satisfaction score of 3.5 was achieved in acitretin group versus 36% and 2.1 for the isotretinoin group. There was significant improvement in hyperkeratosis in 50% of patients (P < 0.001). Overall, 14% patients had amelioration of their pachyonychia; while majority (79%) did not experience any nail change. All patients experienced adverse effects, and 83% discontinued medication. Risk/benefit analysis favored lower retinoid doses (≤25 mg/day) over a longer time period (>5 months), compared with higher doses (>25 mg/day) for a shorter time (≤5 months). Thus oral retinoids especially acitretin in lower doses may be considered a therapeutic modality in the management of pachyonychia congenita.
In a retrospective study of 12 patients with severe, recalcitrant Hidradenitis suppurativa, treated with acitretin for 9-12 months all patients achieved remission and significant improvement in pain, number of nodules and abscesses and long lasting improvement was noticed in 9 patients. [52] Thus acitretin may be used for its antiinflammatory properties in hidradenitis suppurativa. It also targets the process of hyperkeratosis of the infundibular follicular epithelium and eliminates the follicular mass of the keratinocyte-keratin complex. [52]
Acitretin has been reported to cause improvement in individual case reports in patients of porokeratosis with graft versus host disease, generalized linear porokeratosis, erosive pustular dermatosis of scalp, and lichen amyloidosis. [53],[54],[55]
Prophylactic use (chemoprevention) or treatment of precancerous and malignant conditions
There are case reports of acitretin used for prevention of cutaneous malignancies in solar-damaged skin and in genetic syndromes predisposing to skin cancer, for example, epidermodysplasia verruciformis, [56] graft versus host disease, [57] xeroderma pigmentosa, [58] keratoacanthoma, [59] basal cell naevus syndrome (etretinate). In epidermodysplasia verruciformis acitretin has been used as an adjunct in combination with interferon alfa-2a but as monotherapy was ineffective. [56] Acitretin has been reported as drug of choice in the management of keratoacanthomas and squamous cell carcinomas, giant basal cell carcinomas (as adjuvant therapy to surgical removal) in individual case reports. [59],[60],[61]
In a retrospective trial of 32 patients of cutaneous T cell lymphoma (CTCL) treated with acitretin of which 6 patients received montherapy the overall response rate was 59% with mean duration of response being 28 months. Adverse effects were mild with discontinuation of therapy by five patients. Acitretin is well tolerated and potentially effective for early-stage CTCL. Thus response to acitretin, either as adjuvant therapy monotherapy, is comparable with the response to oral agents currently approved for CTCL. [62]
Chemoprevention with systemic retinoids has shown promising prospects in decreasing the incidence of new primary nonmelanoma skin cancers (NMSCs) in immunocompromised posttransplantation recipients. A review of three RCTs by Chen et al., showed significant decrease in the incidence of squamous cell carcinoma (up to 42%), basal cell carcinoma and premalignant lesions (actinic keratosis) in acitrein (not dose dependant) group compared with placebo over a follow up of 6-12 months. [63] However, a randomized controlled trial to assess the efficacy of acitretin as a chemopreventive agent in nontransplantation patients at high-risk for NMSC showed that there although there was a trend that favored the use of acitretin (P = 0.047) to prevent the incidence of NMSC and decrease the number of lesions, this was not a statistically significant benefit, possibly due to low statistical power. [64] Side-effects at higher doses lead to significant drop-outs. Overall, these were small studies with a modest reduction in cancer over a short period of observation, and further studies are required.
Contraindications
The contraindications of acitretin have been enumerated in [Table - 2].
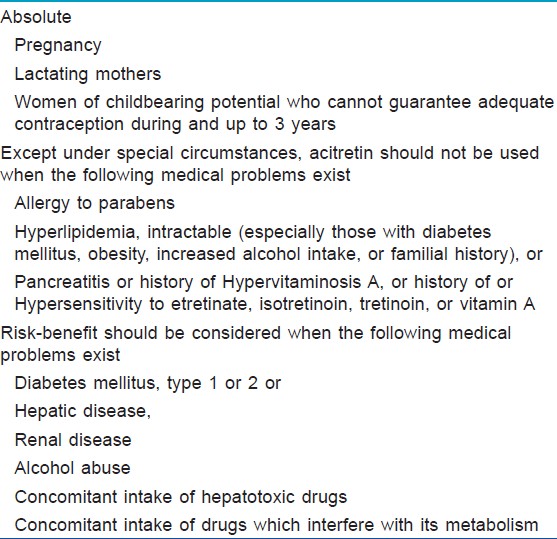
Absolute
The most important contraindication is female patients who are pregnant (CATEGORY X) or want to become pregnant in near future.
Relative
- Neonates: Contraindicated in neonates unless the condition is life threatening (harlequin fetus)
- Children: Should be monitored for bony side effects
- Elderly: Higher risk of adverse events because of preexisting systemic or metabolic derangements
- Patients with systemic diseases (hepatic/renal) or lipid derangements.
Dosage
Response to acitretin is dose dependent, with higher doses yielding greater and rapid improvement. However, adverse effects are also dose dependent, preventing use of higher doses of acitretin. The initial daily dose is 25 or 30 mg for 2-4 weeks, thereafter gradual dose escalation has been shown to be the most effective approach allowing gradual onset of ′tolerance′ to side-effects. [65] Response is gradual peaking at 3-6 months with optimal dose in most patients being 25-50 mg/day up to a maximum of 75-100 mg. As relapse may occur within 2-6 months after discontinuing acitretin, so maintenance therapy is required in most patients based on clinical efficacy and tolerability, recommended dose being 20-50 mg daily which may be reduced to as low as 10-25 mg daily or 25 mg alternate day. It is available in 10 and 25 mg capsules and should ideally be taken with a fatty meal to enhance absorption.
Due to the uncertain effects of long-term acitretin therapy on growth and skeletal development, acitretin should only be used in pediatric patients with the most severe forms of keratinization disorders for which there are no effective alternative therapies.
In individual case reports in neonates and children acitretin given for congenital icthyosis and harlequin icthyosis was found to be safe and effective. It is given at a starting dose of 1 mg/kg body weight and thereafter daily doses can be titrated according to the clinical severity. In children on long-term therapy growth charting and annual screening radiography is advisable. It is advisable to freeze the capsule, cut it into a fraction depending on the dosage when giving to children. This can then be dispensed in children in a liquid like other solid tablets, which are crushed. The excessive part should be discarded as it is sensitive to light.
Newer topical preparation
Acitretin Nanostructured Lipid Carriers are prepared by solvent diffusion technique using 3 (2) full factorial design and NLCs incorporated in 1% w/w Carbopol 934 P gel base. They are lyophilized and crystallinity of NLC characterized by Differential Scanning Calorimtery (DSC) and powder X-Ray Diffraction (XRD). In vitro skin deposition studies in Human Cadaver Skin and double-blind clinical studies in psoriatic patients were evaluated by Agrawal et al. to assess acitretin loaded Nanostructured Lipid Carriers (ActNLCs) and clinically evaluate the role of this gel in the topical treatment of psoriasis. [66] The optimized ActNLCs were spherical in shape, with average particle size of 223 (±8.92) nm, zeta potential of -26.4 (±0.86) mV and EE of 63.0 (±1.54). Significantly higher deposition of Acitretin was found in human cadaver skin from ActNLC gel (81.38 ± 1.23%) versus Acitretin plain gel (47.28 ± 1.02%). Clinical studies demonstrated significant improvement in therapeutic response and reduction in local side effects with ActNLCs loaded gel thus offering a ray of hope for the future management of psoriasis using topical formulation of acitretin.
Monitoring
Liver enzymes, fasting serum cholesterol and triglycerides and blood sugar (in diabetics) every 2-4 weeks for the first 2 months of therapy and then every 3 months. [13] If liver function tests are abnormal weekly checkups should be done and acitretin dose adjusted accordingly. Acitretin should be discontinued if transaminases are elevated to three times their upper normal limit, and patients with bilirubin >50 μmol/L (3 mg/dL) or alanine aminotransferase >200 IU/L should be referred to gastroenterology. If the levels are between 2 and 3 times the normal range, acitretin should be discontinued till they become normal and then restarted at lower doses. [13] If they are elevated only two times then the levels usually resolve even on therapy. However, frequent monitoring is required. Similarly, patients with triglycerides >5 mmol/L (442.48 mg/dL) should be referred to a lipidologist and hypertriglyceridaemia more than 10 mmol/L (884.96 mg/dL) warrants discontinuation of acitretin. [13]
Side effects
All side effects that have been reported for acitretin in the literature are dose-dependent and reversible, except for hyperostosis [Table - 3].
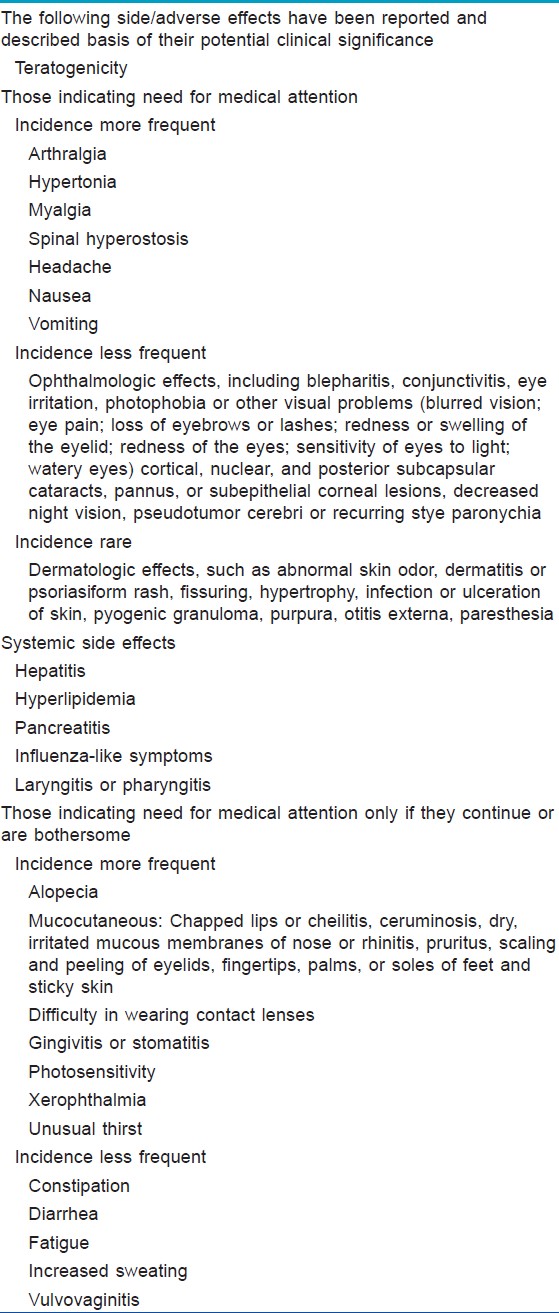
Teratogenicity
There have been a lot of case reports of fetal malformations associated with acitretin use during pregnancy leading to retinoid embryopathy. [67] Retinoid embryopathy can result in craniofacial dysmorphias such as high palate and anophthalmia, abnormalities of appendages including syndactyly and absence of terminal phalanges, malformations of the hip, meningoencephalocele, and multiple synostosis. [68] Acitretin is teratogenic regardless of the duration of treatment or dosage used especially in the first trimester. Two forms of effective contraceptives should be used, beginning one month prior to starting Acitretin, throughout the duration of treatment and for 2 years in Europe and 3 years in US after stopping. Effective forms of contraception include both primary and secondary forms of contraception. Primary forms of contraception include: Tubal ligation, partner′s vasectomy, intrauterine devices, birth control pills, and injectable/implantable/insertable/topical hormonal birth control products. Secondary forms of contraception include latex condoms (with or without spermicide), diaphragms, and cervical caps (which must be used with a spermicide). Acitretin interferes with the action of microdosed progestin (′minipill′) oral contraceptives. So it is not advisable to use this type of birth control while taking acitretin. In women of childbearing age, pregnancy must be excluded by two negative pregnancy tests with a sensitivity of at least 25 mIU/mL with second test to be done during the first 5 days of the menstrual period immediately preceding the beginning of acitretin therapy. For patients with amenorrhea, the second test should be done at least 11 days after the last act of unprotected sexual intercourse and acitretin should be started only on the second or third day of the next menstrual cycle. Regular tests (ideally every month) should be done to rule out pregnancy. The patients of childbearing age should be advised to abstain from alcohol during and 2 months after the cessation of therapy as alcohol intake increases the metabolism of acitretin to etretinate. However, risks from semen of men taking acitrein have not been reported. Blood transfusion is, however, contraindicated for all patients on acitretin therapy.
Mucocutaneous
Mucosal involvement may lead to epistaxis and rhinitis, and ocular disturbances including photophobia, xerophthalmia, and conjunctivitis. Cheilitis, dry mouth, stomatitis, gingivitis, and taste disturbances have been reported. [8],[12],[13],[65],[67],[69] Thinning, redness, and scaling may occur, particularly on the palms and soles. Increased hair loss (up to 75% patients), nail fragility, paronychia and periungual pyogenic granuloma may occur. Rarely, patients may experience photosensitivity reactions and ′retinoid dermatitis′, which resembles unstable psoriasis can also develop in up to 25% of patients receiving high-dose oral acitretin. [8] In a retrospective analysis of 176 patients receiving acitretin, cheilitis occurred in approximately 60-75% patients, skin peeling in 25-50%, rhinitis in 20-30%, dry skin in 15-25%, and hair loss in 10-25%. Other effects such as sticky skin, rigors, itchiness, and dry mouth were less common, occurring in fewer than 25% of patients, even in those receiving the highest doses. [65] These mucocutaneous side effects can be treated symptomatically and do not require discontinuation of therapy. Although most of the studies suggest these side effects to be dose related, [8] there are studies that refute it. [7],[17]
Hepatotoxicity
Use of acitretin may cause transient and reversible elevation in serum liver enzymes in up to 15% of patients. [69],[70] However, severe hepatotoxic reactions (severe cholestatic hepatitis/cirrhosis) and overt hepatitis are rare (0.26%). [71] Frequent monitoring of liver function is recommended in alcoholics, diabetics, obese individuals, and patients with concurrent use of other hepatotoxic agents.
Hyperlipidemia
Retinoid therapy may cause changes in the serum lipid profile especially increase in triglycerdes and cholesterol and decease in high density lipoprotein (HDL). The greatest increase is seen in triglycerides, which occurs in 20-40% of patients while hypercholesterolaemia, is seen in 10-30% of patients due to increases in both the VLDL and/or low density lipoprotein (LDL) fractions and decrease in the HDL fraction (40% patients) leading to increased risk of developing cardiovascular disease. [12],[69] One case of fatal fulminant pancreatitis due to hypertriglceridemia has been reported. [71] These effects are reversible and can be managed by dietary modifications, fish oil rich diet, oral hypolipidemic drugs or decreasing acitretin dose. In a retrospective analysis on side effect profile of 525 patients receiving acitretin therapy in doses 10-75 mg/day, increased triglyceride levels occurred in 66% and total cholesterol increased in 33% of patients.
Pancreatitis
Increase in serum triglycerides levels leading to pancreatitis is uncommonly reported (single case). [71] However, patients with diabetes mellitus, obesity, increased alcohol intake, or a family history of hypertriglyceridemia have increased predisposition to this complication.
Pseudotumor cerebri or benign intracranial hypertension has been reported rarely with acitretin especially in patients with concurrent tetracycline or minocycline administration leading to headache, visual changes, nausea, or vomiting and papilledema. [69] Such patients should discontinue acitretin immediately and shall be referred for neurological evaluation.
Hyperostosis
Long-term (2-4 years) treatment with acitretin has been associated with radiographic evidence of extraspinal tendon and ligament calcification, the most common sites being ankles, pelvis, and knees. [72] Diffuse idiopathic skeletal hyperostosis (DISH)-like involvement, characterized by degenerative spondylosis, vertebral arthritis, and syndesmophytes of the vertebral spine, has also been reported but these changes have found no correlation with dose or duration of treatment. Occasional reports of bone changes including premature epiphyseal closure, skeletal hyperostosis, and extraosseous calcification have been reported in pediatric age group. However, recent studies do not focus on any growth or bony abnormalities in patients on long-term retinoids. [73] Thus routine annual radiography is not warranted in adults unless symptomatic. Pretreatment X-rays for bone age including X-rays of the knees or ankles are generally advised in children. Bone scans (scintigraphs) and/or X-rays should be considered at yearly intervals when monitoring children on long-term therapy. Atypical musculoskeletal pain or limitation of movement should be evaluated by appropriate radiological examination. Recent British Association of Dermatology (BAD) guidelines, however, do not recommend routine radiography for monitoring in children unless warranted as it may cause unnecessary radiation exposure. However, growth charting should be done for children on acitretin to detect premature closure at early stage. Other rheumatological manifestations that may occur during therapy with acitretin include arthralgias, arthritis, myalgias, osteopenia and a few cases of vasculitis, Wegener granulomatosis, and erythema nodosum. [13]
Other side effects
Vulvovaginitis, increased insulin sensitivity, and delayed wound healing have also been reported. [13] Acitretin although leads to excessive granulation tissue formation, does not significantly affect wound healing. In a study of 44 complex wounds in transplant recipients by Tan et al., there were no significant effects on wound infection, dehiscence, hypertrophic scarring, or hypergranulation. There is therefore no need to stop acitretin for routine surgery such as orthopedic procedures.
Drug Interactions
Tetracycline and minocycline: Increased photosensitivity, pseudotumor cerebri (although the single case report of pseudotumor reported with acitretin was not associated with tetracycline intake)
Alcohol
Increased conversion to etretinate, hepatotoxicity.
Vitamin A supplements
Hypervitaminosis. Intake should not exceed the recommended dietary allowance (2400-3000 IU daily).
Antidiabetic agents
Alterations in blood glucose may occur. In a study of seven healthy male volunteers, acitretin treatment potentiated the blood glucose lowering effect of glibenclamide in three of the seven subjects. Repeating the study with six healthy male volunteers in the absence of glibenclamide did not detect an effect of acitretin on glucose tolerance. Careful supervision of diabetic patients under treatment with acitretin is therefore recommended.
Corticosteroids
Hyperlipidemia, pseudotumor cerebri.
Methotrexate and other hepatotoxic drugs
Increased methotrexate level, hepatotoxicity.
Following oral absorption, acitretin undergoes extensive metabolism and interconversion by simple isomerization to its 13-cis form (cis-acitretin) in the liver by cytochrome enzymes. The concomitant administration of methotrexate or other hepatotoxic drugs that are also metabolized in liver by these enzymes thus alters the pharmacodynamics with increased blood levels of methotrexate and further hepatotoxicity.
Progesterone pills ("minipill") preparations
Acitretin decreases the antiovulatory effect of the progestin only pill (mini-pill) but has no effect on the combined preparations.
Excessive exposure to sunlight or phototoxic drugs: Increased photosensitivity.
Thus, Acitretin monotherapy is recommended in the treatment of: [13]
- Severe psoriasis, or psoriasis with severe effects on quality of life, meriting systemic therapy, which is resistant to topical therapy, phototherapy or is unsuitable for these treatments (A, 1+)
- In combination with PUVA therapy or narrowband phototherapy (A, 1+)
- In combination with calcipotriol ointment (A, 1+)
- Palmoplantar pustular psoriasis (A, 1+)
- Hyperkeratotic hand eczema (A, 1+)
- Severe Darier disease (A, 1+)
- Severe congenital ichthyosis (D, 3)
- Keratoderma (D, 3).
- Lichen planus (A, 1+)
- Lichen sclerosus (A, 1+)
- Discoid lupus erythematosus (A, 1+)
- Prevention of cutaneous malignancies in organ transplant patients (A, 1+).
Acitretin has been found to be effective in psoriasis, keratinization disorders, inflammatory dermatosis, and as an antineoplastic agent. Despite being associated with a wide range of side effects, the benefits of its use scores over the side effects. However, teratogenicity is a serious concern and adequate monitoring is required especially in higher risk groups.
| 1. |
Nguyen EH, Wolverton S. Systemic retinoids. In: Wolverton SE, editors. Comprehensive dermatologic drug therapy. 2 nd ed. Philadelphia: WB Saunders Co.; 2007. p. 275-300.
[Google Scholar]
|
| 2. |
Wiegand UW, Chou RC. Pharmacokinetics of acitretin and etretinate. J Am Acad Dermatol 1998;39:S25-33.
[Google Scholar]
|
| 3. |
Pilkigton T, Brogden RN. Acitretin: A review of its pharmacology and therapeutic use. Drugs 1992;43:597-627.
[Google Scholar]
|
| 4. |
McNamara PJ, Jewell RC, Jensen BK, Brindley CJ. Food increases the bioavailability of acitretin. J Clin Pharmacol 1988;28:1051-5.
[Google Scholar]
|
| 5. |
Larsen FG, Steinkjer B, Jakobsen P, Hjorter A, Brockhoff PB, Nielsen Kudsuk F. Acitretin is converted to etretinate only during concomitant alcohol intake. Br J Dermatol 2000;143:1164-9.
[Google Scholar]
|
| 6. |
Tong PS, Horowitz NN, Wheeler LA. Trans retinoic acid enhances the growth response of epidermal keratinocytes to epidermal growth factor and transforming growth factor beta. J Invest Dermatol 1990;94:126-31.
[Google Scholar]
|
| 7. |
Goldfarb MT, Ellis CN, Gupta AK, Tincoff T, Hamilton TA, Voorhees JJ. Acitretin improves psoriasis in a dose-dependent fashion. J Am Acad Dermatol 1988;18:655-62.
[Google Scholar]
|
| 8. |
Kragballe K, Jansen CT, Geiger JM, Bjerke JR, Falk ES, Gip L, et al. A double-blind comparison of acitretin and etretinate in the treatment of severe psoriasis. Results of a Nordic multicentre study. Acta Derm Venereol 1989;69:35-40.
[Google Scholar]
|
| 9. |
Caca-Biljanovska NG, V'Lckova-Laskoska MT. Management of guttate and generalized psoriasis vulgaris: Prospective randomized study. Croat Med J 2002;43:707-12.
[Google Scholar]
|
| 10. |
Lauharanta J, Geiger JM. A double-blind comparison of acitretin and etretinate in combination with bath PUVA in the treatment of extensive psoriasis. Br J Dermatol 1989;121:107-12.
[Google Scholar]
|
| 11. |
Saurat JH, Geiger JM, Amblard P, Beani JC, Boulanger A, Claudy A, et al. Randomized double-blind multicenter study comparing acitretin-PUVA, etretinate-PUVA and placebo-PUVA in the treatment of severe psoriasis. Dermatologica 1988;177:218-24.
[Google Scholar]
|
| 12. |
Gupta AK, Goldfarb MT, Ellis CN, Voorhees JJ. Side-effect profile of acitretin therapy in psoriasis. J Am Acad Dermatol 1989;20:1088-93.
[Google Scholar]
|
| 13. |
Ormerod AD, Campalani E, Goodfield MJ. British Association of Dermatologists guidelines on the efficacy and use of acitretin in Dermatology. Br J Dermatol 2010;162:952-63.
[Google Scholar]
|
| 14. |
Lassus A, Geiger JM. Acitretin and etretinate in the treatment of palmoplantar pustulosis: A double blind comparative trial. Br J Dermatol 1988;119:755-9.
[Google Scholar]
|
| 15. |
Schroder K, Zaun H, Holzmann H, Altmeyer P, el-Gammal S. Pustulosis palmo-plantaris. Clinical and histological changes during etretin (acitretin) therapy. Acta Derm Venereol (Stockh) 1989;146 Suppl: S111-6.
[Google Scholar]
|
| 16. |
Tosti A, Ricotti C, Romanelli P, Cameli N, Piraccini BM. Evaluation of the efficacy of acitretin therapy for nail psoriasis. Arch Dermatol 2009;145:269-71.
[Google Scholar]
|
| 17. |
Sbidian E, Maza A, Montaudie H, Gallini A, Aractingi S, Aubin F, et al. Efficacy and safety of oral retinoids in different psoriasis subtypes: A systematic literature review. J Eur Acad Dermatol Venereol 2011;25 Suppl 2:S28-33.
[Google Scholar]
|
| 18. |
Gollnick H, Bauer R, Brindley C, Orfanos CE, Plewig G, Wokalek H, et al. Acitretin versus etretinate in psoriasis - clinical and pharmacokinetic results of a German multicenter study. J Am Acad Dermatol 1988;19:458-68.
[Google Scholar]
|
| 19. |
Pearce DJ, Klinger S, Ziel KK, Murad EJ, Rowell R, Feldman SR. Low-dose acitretin is associated with fewer adverse events than high-dose acitretin in the treatment of psoriasis. Arch Dermatol 2006;142:1000-4.
[Google Scholar]
|
| 20. |
Dogra S, Jain A, Kanwar AJ. Efficacy and safety of acitretin in adult patients with severe plaque type psoriasis: A randomized, double blind, parallel group, dose ranging study in three fixed doses of 25, 35 and 50 mg. J Eur Acad Dermatol Venereol 2012 [In press].
[Google Scholar]
|
| 21. |
Haushalter K, Murdad EJ, Dabade TS, Rowell R, Pearce DJ, Feldman SR. Efficacy of low-dose acitretin in the treatment of psoriasis. J Dermatolog Treat 2012;23:400-3.
[Google Scholar]
|
| 22. |
Ozdemir M, Engin B, Baysal I, Mevlitoglu L. A randomized comparison of acitretin-narrow-band TL-01 phototherapy and acitretin-psoralen plus ultraviolet A for psoriasis. Acta Derm Venereol (Stockh) 2008;88:589-93.
[Google Scholar]
|
| 23. |
Rim JH, Park JY, Choe YB, Youn JI. The efficacy of calcipotriol plus acitretin combination therapy for psoriasis: Comparison with acitretin monotherapy. Am J Clin Dermatol 2003;4:507-10.
[Google Scholar]
|
| 24. |
Gisondi P, Del Giglio M, Cotena C, Girolomoni G. Combining etanercept and acitretin in the therapy of chronic plaque psoriasis: A 24-week, randomized, controlled, investigator-blinded pilot trial. Br J Dermatol 2008;158:1345-9.
[Google Scholar]
|
| 25. |
Beck HI, Foged EK. Toxic hepatitis due to combination therapy with methotrexate and etretinate in psoriasis. Dermatologica 1983;167:94-6.
[Google Scholar]
|
| 26. |
Kuijpers AL, van Dooren-Geebe RJ, van de Kerkhof PC. Failure of combination therapy with acitretin and cyclosporin A in 3 patients with erythrodermic psoriasis. Dermatology 1997;194:88-90.
[Google Scholar]
|
| 27. |
Van Dooren-Greebe RJ, van de Kerkhof PC, Happle R. Acitretin monotherapy in Darier's disease. Br J Dermatol 1989;121:375-9.
[Google Scholar]
|
| 28. |
Christophersen J, Geiger JM, Danneskiold-Samsoe P, Kragballe K, Larsen FG, Laurberg G, et al. A double-blind comparison of acitretin and etretinate in the treatment of Darier's disease. Acta Derm Venereol (Stockh) 1992;72:150-2.
[Google Scholar]
|
| 29. |
Kirby B, Watson R. Pityriasis rubra pilaris treated with acitretin and narrow-band ultraviolet B (Re-TL-01). Br J Dermatol 2000;142:376-7.
[Google Scholar]
|
| 30. |
Laurberg G, Geiger JM, Hjorth N, Holm P, Hou-Jensen K, Jacobsen KU, et al. Treatment of lichen planus with acitretin. A double-blind, placebo-controlled study in 65 patients. J Am Acad Dermatol 1991;24:434-7.
[Google Scholar]
|
| 31. |
Cribier B, Frances C, Chosidow O. Treatment of lichen planus: An evidence-based medicine analysis of efficacy. Arch Dermatol 1998;134:1521-30.
[Google Scholar]
|
| 32. |
Jaime TJ, Guaraldi Bde M, Melo DF, Jeunon T, Lerer C. Disseminated hypertrophic lichen planus: Relevant response to acitretin. An Bras Deramatol 2011;86:96-9.
[Google Scholar]
|
| 33. |
Ruzicka T, Sommerburg C, Goerz G, Kind P, Mensing H. Treatment of cutaneous lupus erythematosus with acitretin and hydroxychloroquine. Br J Dermatol 1992;127:513-8.
[Google Scholar]
|
| 34. |
Ruzicka T, Meurer M, Bieber T. Efficiency of acitretin in the treatment of cutaneous lupus erythematosus. Arch Dermatol 1988;124:897-902.
[Google Scholar]
|
| 35. |
Bousema MT, Romppanen U, Geiger JM, Baudin M, Vähä-Eskeli K, Vartiainen J, et al. Acitretin in the treatment of severe lichen sclerosus et atrophicus of the vulva: A double-blind, placebo-controlled study. J Am Acad Dermatol 1994;30:225-31.
[Google Scholar]
|
| 36. |
Lacour M, Mehta-Nikhar B, Atherton DJ, Harper JI. An appraisal of acitretin therapy in children with inherited disorders of keratinization. Br J Dermatol 1996;134:1023-9.
[Google Scholar]
|
| 37. |
Happle R, van de Kerkhof PC, Traupe H. Retinoids in disorders of keratinization: Their use in adults. Dermatologica 1987;175 Suppl 1:S107-24.
[Google Scholar]
|
| 38. |
Katugampola RP, Finlay AY. Oral retinoid therapy for disorders of keratinization: Single-centre retrospective 25 years' experience on 23 patients. Br J Dermatol 2006;154:267-76.
[Google Scholar]
|
| 39. |
Bondeson ML, Nystrom AM, Gunnarsson U, Vahlquist A. Connexin 26 (GJB2) mutations in two Swedish patients with atypical Vohwinkel (mutilating keratoderma plus deafness) and KID syndrome both extensively treated with acitretin. Acta Derm Venereol (Stockh) 2006;86:503-8.
[Google Scholar]
|
| 40. |
Erkek E, Erdogan S, Tuncez F, Kurtipek GS, Bagci Y, Ozoguz P, et al. Type I hereditary punctate keratoderma associated with widespread lentigo simplex and successfully treated with low-dose oral acitretin. Arch Dermatol 2006;142:1076-7.
[Google Scholar]
|
| 41. |
Lundgren T, Crossner CG, Twetman S, Ullbro C. Systemic retinoid medication and periodontal health in patients with Papillon-Lefevre syndrome. J Clin Periodontol 1996;23:176-9.
[Google Scholar]
|
| 42. |
Thestrup-Pedersen K, Andersen KE, Menne'T, Veien NK. Treatment of hyperkeratotic dermatitis of the palms (eczema keratoticum) with oral acitretin. A single-blind placebo-controlled study. Acta Derm Venereol (Stockh) 2001;81:353-5.
[Google Scholar]
|
| 43. |
Choi YL, Lee KJ, Kim WS, Lee DY, Lee JH, Lee ES, et al. Treatment of extensive and recalcitrant viral warts with acitretin. Int J Dermatol 2006;45:480-2.
[Google Scholar]
|
| 44. |
El-khavat RH, Haque JS. Use of acitretin in the treatment of resistant viral warts. J Dermatolog Treat 2011;22:194-6.
[Google Scholar]
|
| 45. |
Gelmetti C, Cerri D, Schiuma AA, Menni S. Treatment of extensive warts with etretinate: A clinical trial in 20 children. Pediatr Dermatol 1987;4:254-8.
[Google Scholar]
|
| 46. |
Erkek E, Basar H, Bozdogan O, Emeksiz MC. Giant condyloma acuminate of Buschke-Lo¨wenstein: Successful treatment with a combination of surgical excision, oral acitretin and topical imiquimod. Clin Exp Dermatol 2009;34:366-8.
[Google Scholar]
|
| 47. |
Lee YS, Jung SW, Sim HS, Seo JK, Lee SK. Blastomycosis-like Pyoderma with Good Response to Acitretin. Ann Dermatol 2011;23:365-8.
[Google Scholar]
|
| 48. |
Newland K, Marshman G. Success treatment of post-irradiation morphoea with acitretin and narrowband UVB. Australas J Dermatol 2012;53:136-8.
[Google Scholar]
|
| 49. |
Monshi B, Richter L, Hashimoto T, Groi BE, Haensch N, Rappersberger K. IgA pemphigus of the subcorneal pustular dermatosis type. Successful therapy with a combination of dapsone and acitretin. Hautarzt 2012;63:482-6.
[Google Scholar]
|
| 50. |
Cardoso JC, Cravo M, Cardoso R, Brites MM, Reis JP, Tellechea O, et al. Langerhans cell histiocytosis in an adult: Good response of cutaneous lesions to acitretin. Clin Exp Dermatol 2010;35:627-30.
[Google Scholar]
|
| 51. |
Gruber R, Edlinger M, Kaspar RL, Hansen CD, Leachman S, Milstone LM, et al. An appraisal of oral retinoids in the treatment of pachyonychia congenita. J Am Acad Dermatol 2012;66:e193-9.
[Google Scholar]
|
| 52. |
Boer J, Nazary M. Long-term results of acitretin therapy for hidradenitis suppurativa. Is acne inversa also a misnomer? Br J Dermatol 2011;164:170-5.
[Google Scholar]
|
| 53. |
Garg T, Ramchander, Varghese B, Barara M, Nangia A. Generalized linear porokeratosis: A rare entity with excellent response to acitretin. Dermatol Online J 2011;15:17:3.
[Google Scholar]
|
| 54. |
Darwich E, Munoz Santos C, Mascaro JM Jr. Erosive pustular dermatosis of the scalp responding to acitretin. Arch Dermatol 2011;147:252-3.
[Google Scholar]
|
| 55. |
Carlesimo M, Narcisis A, Orsini D, Mari E, Di Russo P, Arcese A, et al. A case of lichen amyloidosus treated with acitretin. Clin Ter 2011;162:e59-61.
[Google Scholar]
|
| 56. |
Anadolu R, Oskay T, Erdem C, Boyvat A, Terzi E, Gürgey E, et al. Treatment of epidermodysplasia verruciformis with a combination of acitretin and interferon alfa-2a. J Am Acad Dermatol 2001;45:296-9.
[Google Scholar]
|
| 57. |
Borroni RG, Poddighe D, Zecca M, Brazelli V. Efficacy of acitretin for porokeratosis in a child with chronic cutaneous graft versus host disease. Paediatr Dermatol 2013;30:148-50.
[Google Scholar]
|
| 58. |
Berth-Jones J, Cole J, Lehmann AR, Arlett CF, Graham Brown RA. Xeroderma pigmentosum variant: 5 years of tumour suppression by etretinate. J R Soc Med 1993;86:355-6.
[Google Scholar]
|
| 59. |
Robertson SJ, Bashir SJ, Pichert G, Robson A, Whittaker S. Severe exacerbation of multiple self-healing squamous epithelioma (Ferguson-Smith disease) with radiotherapy, which was successfully treated with acitretin. Clin Exp Dermatol 2010;35:e100-2.
[Google Scholar]
|
| 60. |
Sanmartin V, Aquavo R, Baradad M, Casanova JM. Oral acitretin and topical imiquimod as neoadjuvant treatment for giant basal cell carcinoma]. Actas Dermosifiliogr 2012;103:149-52.
[Google Scholar]
|
| 61. |
Foxton G, Delaney T. Eruptive keratoacanthoma and squamous cell carcinoma complicating imiquimod therapy: Response to oral acitretin. Australas J Dermatol 2011;52:66-9.
[Google Scholar]
|
| 62. |
Cheeley J, Sahn RE, Delong LK, Parker SR. Acitretin for the treatment of cutaneous T-cell lymphoma. J Am Acad Dermatol 2013;68:247-54.
[Google Scholar]
|
| 63. |
Chen K, Craig JC, Shumack S. Oral retinoids for the prevention of skin cancers in solid organ transplant recipients: A systematic review of randomized controlled trials. Br J Dermatol 2005;152:518-23.
[Google Scholar]
|
| 64. |
Kadakia KC, Barton Dl, Loprinzi CL, Sloan JA, Otley CC, Diekmann BB, et al. Randomized controlled trial of acitretin versus placebo in patients at high-risk for basal cell or squamous cell carcinoma of the skin (North Central Cancer Treatment Group Study 969251). Cancer 2012;118:2128-37.
[Google Scholar]
|
| 65. |
Nikam BP, Amladi S, Wadhwa SL. Acitretin. Indian J Dermatol Venereol Leprol 2006;72:167-72.
[Google Scholar]
|
| 66. |
Agrawal Y, Petkar KC, Sawant KK. Development, evaluation and clinical studies of Acitretin loaded nanostructured lipid carriers for topical treatment of psoriasis. Int J Pharm 2010;401:93-102.
[Google Scholar]
|
| 67. |
Saurat JH. Side effects of systemic retinoids and their clinical management. J Am Acad Dermatol 1992;27:S23-8.
[Google Scholar]
|
| 68. |
De Die-Smulders CE, Sturkenboom MC, Veraart J, van Katwijk C, Sastrowijoto P, van der Linden E. Severe limb defects and craniofacial anomalies in a fetus conceived during acitretin therapy. Teratology 1995;52:215-9.
[Google Scholar]
|
| 69. |
Katz HI, Waalen J, Leach EE. Acitretin in psoriasis: An overview of adverse effects. J Am Acad Dermatol 1999;41:S7-12.
[Google Scholar]
|
| 70. |
Roenigk HH Jr, Callen JP, Guzzo CA, Katz HI, Lowe N, Madison K, et al. Effects of acitretin on the liver. J Am Acad Dermatol 1999;41:584-8.
[Google Scholar]
|
| 71. |
Vahlquist C, Selinus I, Vessby B. Serum-lipid changes during acitretin (etretin) treatment of psoriasis and palmoplantar pustulosis. Acta Derm Venereol (Stockh) 1988;68:300-5.
[Google Scholar]
|
| 72. |
McGuire J, Lawson JP. Skeletal changes associated with chronic Isotretinoin and etretinate administration. Dermatologica 1987;175:S169-81.
[Google Scholar]
|
| 73. |
Van Dooren-Greebe RJ, Lemmens JA, De Boo T, Hangx NM, Kuijpers AL, van de Kerkhof PC. Prolonged treatment with oral retinoids in adults: No influence on the frequency and severity of spinal abnormalities. Br J Dermatol 1996;134:71-6.
[Google Scholar]
|
Fulltext Views
26,601
PDF downloads
4,473





