Translate this page into:
A case of classic Kaposi sarcoma in a 11-year-old male
2 Ministry of Health, Ankara Training and Research Hospital, Dermatovenereology, Ankara, Turkey
3 Hacettepe University, Faculty of Medicine, Pathology, Ankara, Turkey
4 Dermatopathologische Gemeinschaftspraxis, Friedrichshafen, Germany
Correspondence Address:
Goknur Kalkan
Cumhuriyet street No:78, Samsun
Turkey
| How to cite this article: Kalkan G, Akbay G, Gungor E, Eken A, Ozkaya O, Kutzner H, Eksioglu M. A case of classic Kaposi sarcoma in a 11-year-old male. Indian J Dermatol Venereol Leprol 2011;77:730 |
Sir,
Kaposi sarcoma (KS) is a highly vascular tumor arising from the human herpesvirus 8 (HHV-8) infected lymphatic endothelium. Worldwide, occasional cases of classic KS have been reported in children. [1],[2] Herein, we report an Human immunodeficiency virus (HIV)-seronegative 11-year-old boy with a 3-year history of lesions, who was diagnosed as classic KS clinically and histopathologically.
A 11-year-old boy was admitted to our clinic with maculopapular and nodular lesions on the dorsum of the hands and feet. On dermatological examination he had pinkish-purple colored, well-demarcated, painless maculopapular lesions, measuring 0.5 - 2 cm on the soles of feet and dorsum of the feet and hands and had a hemorrhagic crusted nodular lesion between the third and fourth toes [Figure - 1] and [Figure - 2]. Clinical examination revealed mild pallor with enlarged axillary and inguinal lymph nodes. Complete blood count, urinalysis, blood chemistry, erythrocyte sedimentation rate, immunoglobulin and complement levels were all within normal limits. Flow cytometric examination of the peripheral blood demonstrated normal values for CD3, CD4, CD8, CD4 /CD8 ratio, CD5, CD20 and CD56 lymphocytic markers. Immunoglobulin (Ig) G antibodies for Cytomegalovirus (CMV) and for the Epstein-Barr nuclear antigen 1 (EBNA-1) and VCA p 19 antigen and were positive. Antibodies against HIV, hepatitis B and C were all negative. No abnormality was detected in chest X-ray or electrocardiographic features. The biopsy specimen from the lesion on the feet revealed vascular neoplasm in a nodular formation beneath the thinned epidermis and increased spindle cells with vascular clefts and structures with a predominance of large endothelial cells [Figure - 3] and [Figure - 4]. HHV-8 was detected in the tissues by polymerase chain reaction (PCR) assay. Immunohistochemical staining was positive for HHV-8 latent nuclear antigen. Neck and abdominal ultrasonography and thoracoabdominal computed tomography showed bilateral multiple lymphadenopathy, and the largest measured lymph nodes were 15 × 9 mm in the cervical area, 25 × 8 mm in the left inguinal area and 9 × 4 mm in the right axillary region. We referred our patient to a children hospital for treatment. He was treated with interferon alpha for six months and lesions started to resolve. Treatment with interferon alfa, at a dose of 3.3 million IU, three times weekly, was initiated; however, since two months later new lesions developed, the dose was increased to 4 million IU. He is still following up and his treatment is going on.
 |
| Figure 1: Well-demarcated, painless maculopapular lesions on the feet |
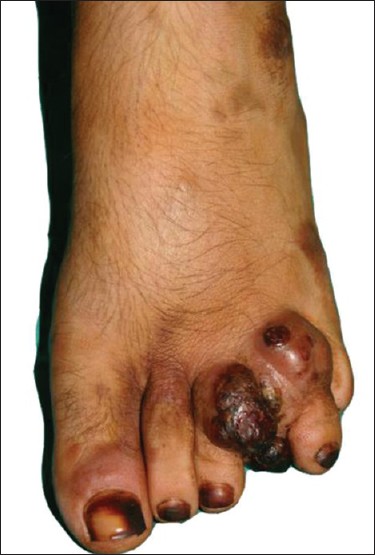 |
| Figure 2: Hemorrhagic crusted nodular lesion between the third and fourth toes |
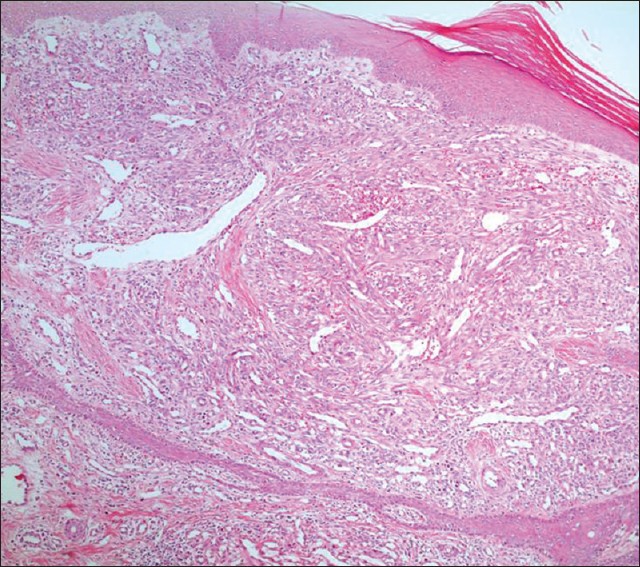 |
| Figure 3: Increased spindle cells with vascular clefts and vascular structures with a predominance of large endothelial cells (H and E, ×40) |
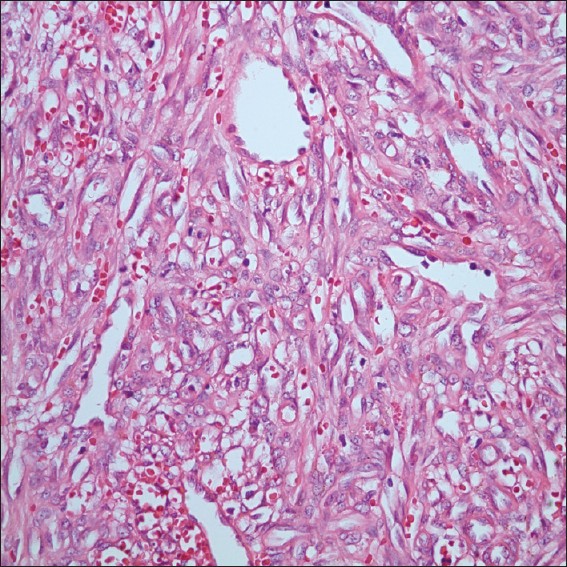 |
| Figure 4: Vascular clefts and vascular structures, higher power magnification (H and E, ×400) |
Classic KS is exceedingly rare in childhood, with only 29 reported cases worldwide in the last 50 years. These cases were idiopathic, as no known acquired or inherited risk factors could be identified. [3] The patient described herein was an HIV- seronegative 11-year-old boy. Histopathological diagnosis was established as KS. The patient had no clinical or laboratory evidence of immune deficiency and was previously healthy. There was no history of receiving immunosuppressive agents and he was seronegative for HIV. Furthermore, his disease cannot be classified as epidemic or African-endemic. Therefore, his condition best fits the classic form of KS.
The presence of HHV-8 infection has now been found in over 95% of KS tumors, supporting evidence that HHV-8 has a causal role in the development of KS. [4] It is not yet known whether HHV-8 directly produces classic KS, and several cytokines may also contribute to its development. [5] Also in our case, HHV-8 was detected by PCR and sequences. Immunohistochemical staining also supported this diagnosis as it was positive for HHV-8 latent nuclear antigen. Infection with HHV-8 is essential for the onset of KS, and detection of the virally encoded latency-associated nuclear antigen 1 (LANA-1) serves as a useful tool for distinguishing KS from its mimics, providing high sensitivity and specificity that was also positive in our patient.
The important differential diagnostic considerations are Kaposiform hemangioendothelioma and spindle cell hemangioma. Although KS and spindle cell hemangioma both are characterized by proliferations of spindle cells, KS lacks the cavernous spaces and vacuolated histiocytoid cells between spindle cells. [6] Kaposiform hemangioendothelioma is distinguished from KS by a strongly lobular architecture and lack of plasma cell infiltrates. [7] Management modalities for KS include nonintervention, surgical excision, laser surgery, radiotherapy, chemotherapy, immunotherapy, antiviral drugs, and cessation of immunosuppressive therapy in iatrogenically immunosuppressed patients. [4] The efficacy of taxanes has also been shown. [8] Pegylated liposomal doxorubicin is being used as a second-line therapy for the patients with advanced classic KS. [9]
Finally, blue-purple colored papular or nodular cutaneous lesion, ulcerated or not, on any part of the body, even in juveniles, could be an early manifestation of KS. Classic KS is extremely rare in pediatric population, despite the fact that 5% of children are reportedly exposed to HHV-8. Since physicians are not familiar with the disease in children, we would like to draw the attention to this form of KS and underline the importance of recognizing the lesions of classic KS.
| 1. |
Iscovich J, Boffetta P, Franceschi S, Azizi E, Sarid R. Classic kaposi sarcoma: Epidemiology and risk factors. Cancer 2000;88:500-17.
[Google Scholar]
|
| 2. |
Dutz W, Stout AP. Kaposi's sarcoma in infants and children. Cancer 1960;13:684-94.
[Google Scholar]
|
| 3. |
Camcioglu Y, Picard C, Lacoste V, Dupuis S, Akcakaya N, Cokura H, et al. HHV-8-associated Kaposi sarcoma in a child with IFN gamma R1 deficiency. J Pediatr 2004;144:519-23.
[Google Scholar]
|
| 4. |
Greenblatt RM. Kaposi's sarcoma and human herpesvirus-8. Infect Dis Clin North Am 1998;12:63-82.
[Google Scholar]
|
| 5. |
Landau HJ, Poiesz BJ, Dube S, Bogart JA, Weiner LB, Souid AK. Classic Kaposi's sarcoma associated with human herpesvirus 8 infection in a 13-year-old male: A case report. Clin Cancer Res 2001;7:2263-8.
[Google Scholar]
|
| 6. |
Weiss SW, Enzinger FM. Spindle cell hemangioendothelioma. A low grade angiosarcoma resembling a cavernous hemangioma and kaposi's sarcoma. Am J Surg Pathol 1986;10:521-30.
[Google Scholar]
|
| 7. |
Zukerberg LR, Nickoloff BJ, Weiss SW. Kaposiform hemangioendothelioma of infancy and childhood. An aggressive neoplasm associated with Kasabach-Meritt syndrome and lymphangiomatosis. Am J Surg Pathol 1993;17:321-8.
[Google Scholar]
|
| 8. |
Fardet L, Stoebner PE, Bachelez H, Descamps V, Kerob D, Meunier L, et al. Treatment with taxanes of refractory or life-threatening Kaposi sarcoma not associated with human immunodeficiency virus infection. Cancer 2006;106:1785-9.
[Google Scholar]
|
| 9. |
Di Lorenzo G, Di Trolio R, Montesarchio V, Palmieri G, Nappa P, Delfino M, et al. Pegylated liposomal doxorubicin as second-line therapy in the treatment of patients with advanced classic Kaposi sarcoma: A retrospective study. Cancer 2008;112:1147-52.
[Google Scholar]
|
Fulltext Views
3,676
PDF downloads
4,062





