Translate this page into:
A case of cutaneous Rosai-Dorfman disease presenting with auricular enlargement as the first manifestation
2 Department of Mycology, Institute of Dermatology, Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing, Jiangsu Province, China
Correspondence Address:
Yi-Qun Jiang
No. 12, Jiangwang Temple Street, Xuanwu District, Nanjing, Jiangsu Province
China
| How to cite this article: Gan L, Liu WD, Yu WT, Sun JF, Jiang YQ. A case of cutaneous Rosai-Dorfman disease presenting with auricular enlargement as the first manifestation. Indian J Dermatol Venereol Leprol 2019;85:518-522 |
Sir,
Rosai-Dorfman disease, originally known as sinus histiocytosis with massive lymphadenopathy, is a non-Langerhans cell histiocytosis. It generally involves lymph nodes as well as extranodal organs among which skin involvement is the most common.
When the skin gets involved it is termed cutaneous Rosai-Dorfman disease which usually presents as papules, nodules, plaques or lesions in combination.[1] A yellow hue is characteristic for skin lesions of Rosai-Dorfman disease, while the overall appearance is erythematous or sometimes hyperpigmented. Initial presentation with plaque on the ear is uncommon and therefore may be easily misdiagnosed. We describe a case of cutaneous Rosai-Dorfman disease on the right ear of a 47-year-old man.
The patient presented with a 10-month history of unilateral auricular enlargement. The lesion was initially an erythematous papule that progressively enlarged to form a reddish-purple plaque and there was no significant pain or pruritus [Figure - 1]. The patient complained of hearing loss but denied otalgia or otorrhea. On examination, cranial nerve and vestibular examinations were unremarkable. The Weber tuning fork test lateralized to the right and Rinne's test was negative bilaterally. The audiogram showed a right-sided mild conductive hearing loss with a sensorineural component at high frequencies. On the basis of a biopsy taken from a local hospital which showed dermal inflammatory infiltration of lymphocytes and histiocytes, he was initially diagnosed as possible infectious granuloma. Further study of the formalin-fixed paraffin embedded tissue by periodic acid–Schiff and acid-fast bacilli stains as well as fresh tissue submitted for tissue culture showed no evidence of fungi or mycobacteria. One month later, a plaque with overlying nodules developed on the back [Figure - 2]. The patient was otherwise in good health. He denied any history of trauma and preceding or concurrent illnesses, including fever. No lymphadenopathy or extracutaneous involvement were documented in physical examination and imaging studies which included computed tomography scan of the chest and ultrasound of the abdomen. Routine laboratory test results were within normal limits, including blood and urine routine analysis, liver and kidney functions and serum immune electrophoresis. Repeat biopsies were obtained from both the ear and the back lesions. The biopsy from the ear lesion showed dense dermal infiltrates of plasma cells, lymphocytes and some pale histiocytes with no epidermal and dermo-epidermal junction changes [Figure - 3] and [Figure - 4]. However, the specimen from the back showed sheets of histocytes with abundant foamy cytoplasm and lymphocytes which were engulfed in those large histiocytes (emperipolesis). Aggregates of plasma cells along with lymphocytes were seen dispersed in between large pale histiocytes [Figure - 5], [Figure - 6], [Figure - 7]. A diagnosis of Rosai-Dorfman disease was strongly suspected and further immunohistochemical studies for both lesions were performed. The histiocytes were strongly positive for CD68 and S100 protein, and negative for CD1a [Figure - 8] and [Figure - 9]. Therefore the diagnosis of cutaneous Rosai-Dorfman disease was made. Because the external auditory canal blockage by the lesion had affected his hearing, therapy using oral methylprednisolone 12 mg/day and thalidomide 100 mg/day were administered.[1],[2] An improvement was observed in 4 weeks and the enlargement of the right ear was significantly reduced in 8 weeks. The doses were gradually tapered in about 3 months and there was no recurrence.
 |
| Figure 1: Reddish purple plaque of the right ear at the initial presentation, leading to partial blockage of the external auditory canal |
 |
| Figure 2: A plaque of 1 cm × 1 cm studded with several yellowish red nodules on the back at the initial presentation |
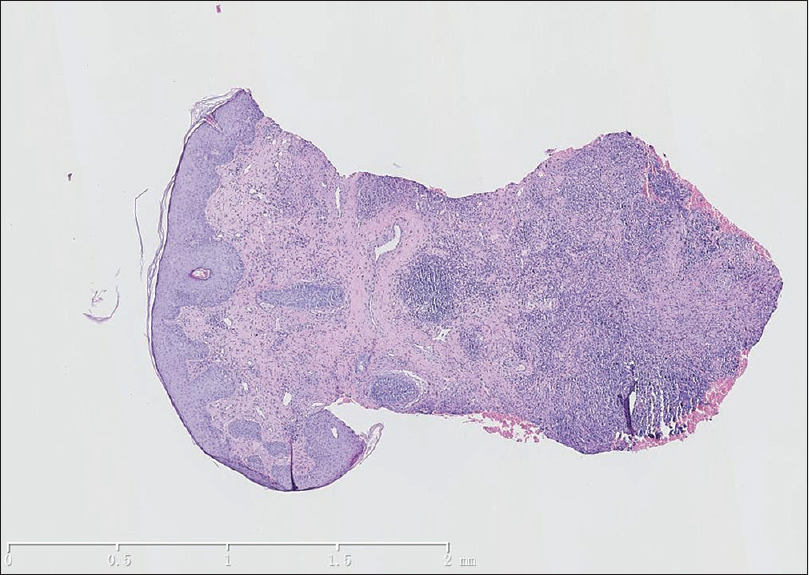 |
| Figure 3: Dense dermal infiltrates of lymphohistocytes with no remarkable dermo-epidermal junctional changes (hematoxylin and eosin, ×25, site: earlobe) |
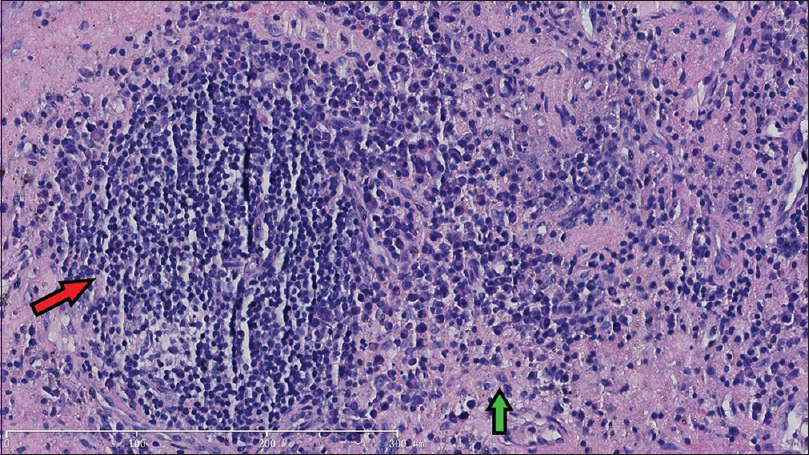 |
| Figure 4: A few pale histiocytes (green arrow) along with dense lymphoplasmocytic infiltration (red arrow) (hematoxylin and eosin, ×200, site: earlobe) |
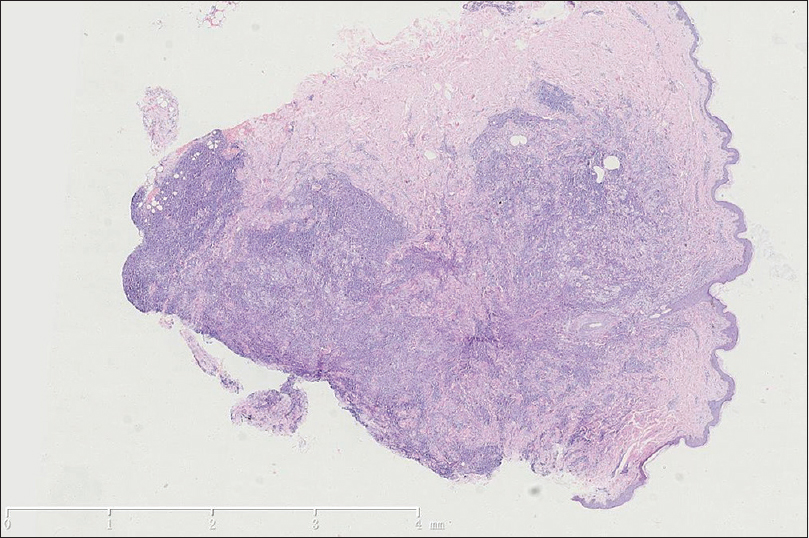 |
| Figure 5: Sheets of dermal infiltration with pale regions while the superimposed epidermis was normal (hematoxylin and eosin, ×12.5, site: back) |
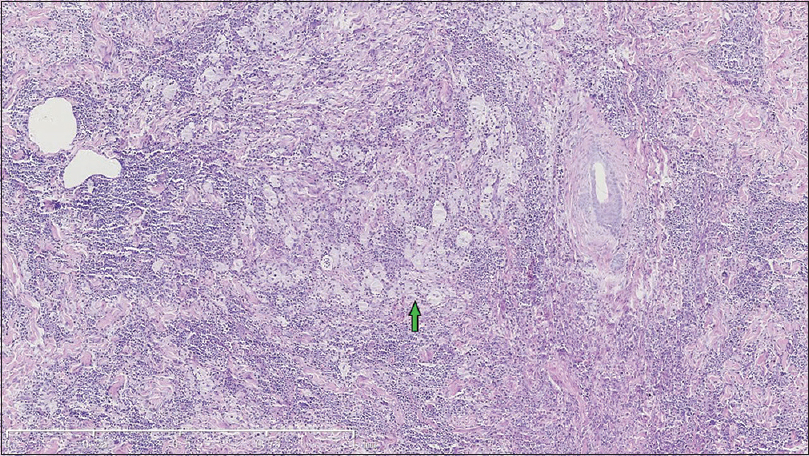 |
| Figure 6: Sheets of histocytes with abundant foamy cytoplasm (green arrow) along with aggregates of plasma cells in the background of lymphocyte infiltrates (hematoxylin and eosin, ×50, site: back) |
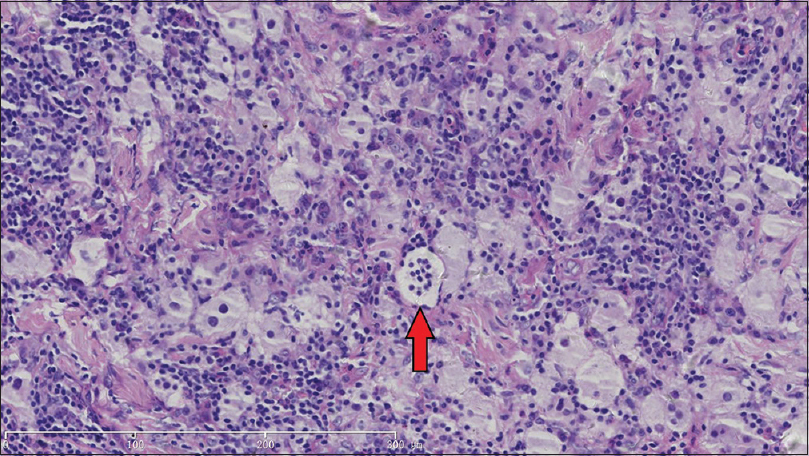 |
| Figure 7: Emperipolesis (red arrow) (hematoxylin and eosin, ×200, site: back) |
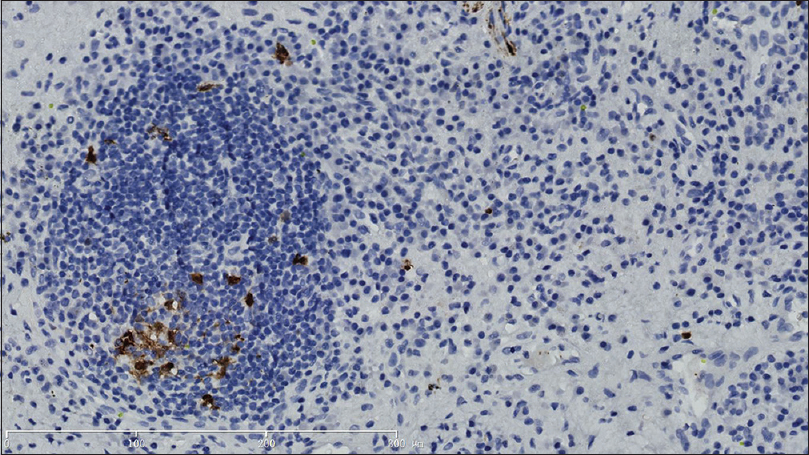 |
| Figure 8: S100 stain highlighted the positive histocytes (immunohistochemical stain, ×200, site: earlobe) |
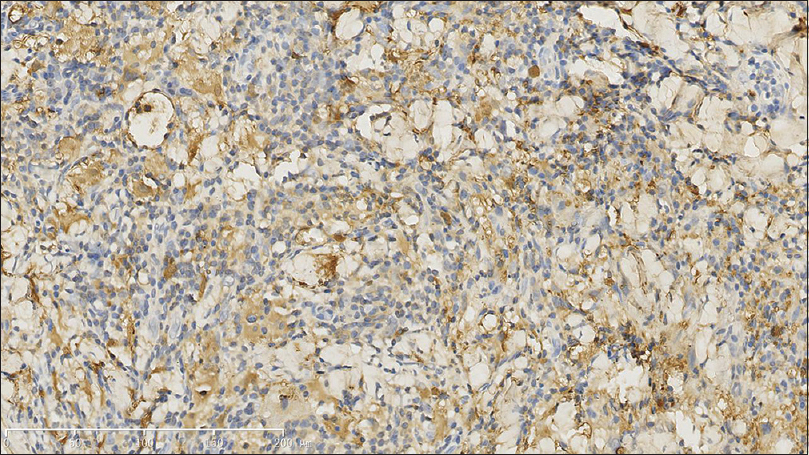 |
| Figure 9: Histiocytes were positive for CD68 (immunohistochemical stain, ×200, site: back) |
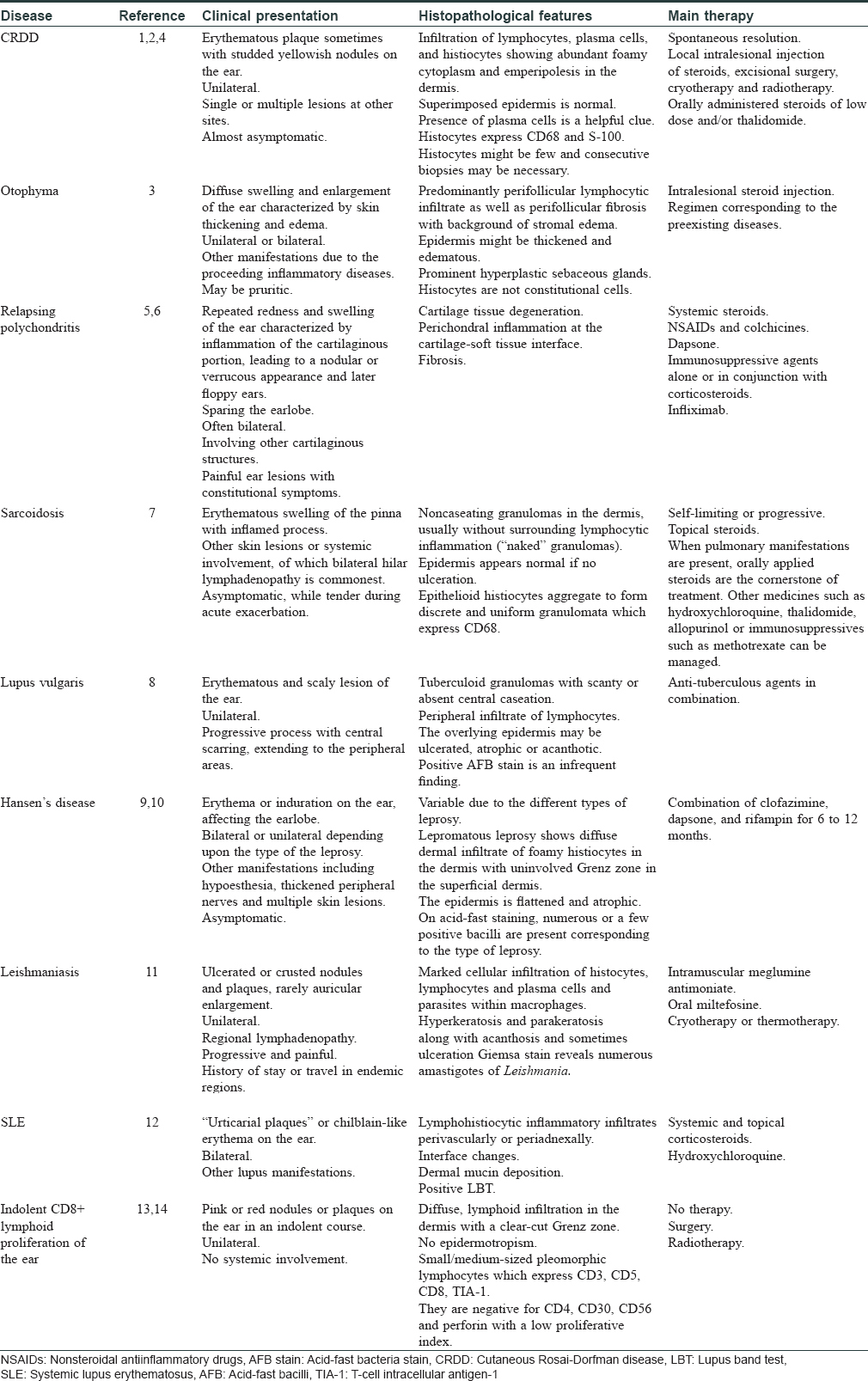
Swelling and enlargement of ear in Rosai Dorfman disease is relatively rare, and there are only a few previous similar reports. Otophyma can present as either unilateral or bilateral enlargement of the ear, probably due to lymphedema which is considered as the end-stage of some chronic inflammatory disorders such as rosacea.[3] Histologically, it is distinct from cutaneous Rosai-Dorfman disease with predominantly dermal perifollicular lymphocytic infiltrate as well as perifollicular fibrosis with background of stromal edema. Prominent hyperplastic sebaceous gland is another hallmark of this entity. Among other differential considerations are sarcoidosis, lupus vulgaris/non-tuberculous mycobacterial infections, Hansen's disease, leishmaniasis, systemic lupus erythematosus and lymphomas [Table - 1]. In our case, the clinical manifestation of the back lesion and histopathological features observed in both sites helped us reach the final diagnosis. The presence of foamy histocytes with emperipolesis may be variable in different cases, and increased plasma cells could be a strong indicator of cutaneous Rosai-Dorfman disease in this situation.[4]
Only a few cases of cutaneous Rosai-Dorfman disease involving the ear have been reported so far.[15],[16] Consistently, no systemic involvement has been identified and it was so in our case too. Nevertheless, it is still compulsory to differentiate cutaneous Rosai-Dorfman disease from systemic Rosai-Dorfman disease with skin involvement. Systemic Rosai-Dorfman disease typically presents as painless, bilateral lymphadenopathy, in children or young adults, with a male preponderance. However, cutaneous Rosai-Dorfman disease seems to occur at an older age, has a female preponderance and also has a higher prevalence in Asians compared with classic systemic Rosai-Dorfman disease. Patients with cutaneous Rosai-Dorfman disease are generally in normal health and characteristically do not show lymphadenopathy, fever or night sweats, and their laboratory findings are within normal limits.[1],[4]
In conclusion, despite distinctive histological features, the clinical diagnosis of cutaneous Rosai-Dorfman disease is sometimes difficult because its clinical presentation varies and may be nonspecific in the absence of characteristic lymphadenopathy. Correlation of the clinicopathologic features and close follow-up to rule out other pathological processes are critical.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
CAMS Innovation Fund for Medical Sciences (CIFMS-2017-I2M-1-017).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Warren TG, Terry LB. Rosai-Dorfman disease. In: Bolognia JL, Schaffer JV, Cerroni L, editors. Dermatology. 4th ed. Philadelphia: Elsevier Limited; 2018. p. 1628-30.
[Google Scholar]
|
| 2. |
Chen E, Pavlidakey P, Sami N. Rosai-Dorfman disease successfully treated with thalidomide. JAAD Case Rep 2016;2:369-72.
[Google Scholar]
|
| 3. |
Carlson JA, Mazza J, Kircher K, Tran TA. Otophyma: A case report and review of the literature of lymphedema (elephantiasis) of the ear. Am J Dermatopathol 2008;30:67-72.
[Google Scholar]
|
| 4. |
Wang KH, Chen WY, Liu HN, Huang CC, Lee WR, Hu CH. Cutaneous Rosai-Dorfman disease: Clinicopathological profiles, spectrum and evolution of 21 lesions in six patients. Br J Dermatol 2006;154:277-86.
[Google Scholar]
|
| 5. |
Cantarini L, Vitale A, Brizi MG, Caso F, Frediani B, Punzi L, et al. Diagnosis and classification of relapsing polychondritis. J Autoimmun 2014;48-49:53-9.
[Google Scholar]
|
| 6. |
Lipsker D, Gattorno M. Relapsing polychondritis. In: Bolognia JL, Schaf-fer JV, Cerroni L, editors. Dermatology. 4th ed. Philadelphia: Elsevier Limited; 2018. p. 726-8.
[Google Scholar]
|
| 7. |
Adelola OA, Fernandez R, Ahmad R, Leamy M, Moriarty BG. Sarcoidosis of the external ear – Literature review and report of a case. J Laryngol Otol 2007;121:289-92.
[Google Scholar]
|
| 8. |
Lhote R, Raskine L, Gottlieb J, Mougari F, Lafaurie M, Vignon-Pennamen MD, et al. Cutaneous tuberculosis of the ear due to Mycobacterium bovis. Ann Dermatol Venereol 2016;143:611-5.
[Google Scholar]
|
| 9. |
Ma S, Kovarik C. Erythema and induration on the right ear and maxilla. Cutis 2016;98:26.
[Google Scholar]
|
| 10. |
Pruthi P, Munganda H, Bangia A, Rani U, Budhiraja R, Brajpuriya S. Leprosy with atypical skin lesions masquerading as relapsing polychondritis. Case Rep Infect Dis 2016;2016:7802423.
[Google Scholar]
|
| 11. |
Robati RM, Qeisari M, Saeedi M, Karimi M. Auricular enlargement: An atypical presentation of old world cutaneous leishmaniasis. Indian J Dermatol 2011;56:428-9.
[Google Scholar]
|
| 12. |
Lela AL, Victoria PW. Lupus erythematosus. In: Bolognia JL, Schaffer JV, Cerroni L, editors. Dermatology. 4th ed. Philadelphia: Elsevier Limited; 2018. p. 662-80.
[Google Scholar]
|
| 13. |
Géraud C, Goerdt S, Klemke CD. Primary cutaneous CD8+ small/medium-sized pleomorphic T-cell lymphoma, ear-type: A unique cutaneous T-cell lymphoma with a favourable prognosis. Br J Dermatol 2011;164:456-8.
[Google Scholar]
|
| 14. |
Atkar RK, Meligonis G, Godic A, Fife K, Burrows NP. Solitary lesion on the ear. Clin Exp Dermatol 2015;40:583-5.
[Google Scholar]
|
| 15. |
Lin SK, Guralnick MP, Cassarino DS. Elusive diagnosis of left ear nodules. Cutaneous Rosai-Dorfman disease (RDD). JAMA Dermatol 2014;150:81-2.
[Google Scholar]
|
| 16. |
Bunick CG, Leffell D, Bosenberg M, Yahalom J, Choi JN. Cutaneous Rosai-Dorfman disease of the right ear responsive to radiotherapy. J Am Acad Dermatol 2012;67:e225-6.
[Google Scholar]
|
Fulltext Views
3,582
PDF downloads
1,732





