Translate this page into:
A case of disseminated subcutaneous phaeohyphomycosis caused by Exserohilum rostratum with CARD9 mutation
Corresponding author: Dr. Mayuri Kalantri, Department of Dermatology, Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra, India. kalantrimayuri11@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kalantri M, Khopkar U, Shah A, Bargir UA, Hule G, Madkaikar M. A case of disseminated subcutaneous phaeohyphomycosis caused by Exserohilum rostratum with CARD9 mutation. Indian J Dermatol Venereol Leprol 2022;88:59-61.
Abstract
Phaeohypomycosis is a rare cutaneous and subcutaneous fungal infection caused by dematiaceous fungi. They have a widespread global distribution occasionally affecting humans. A 26-year-old woman presented with multiple skin lesions over her face and extremities for last 7 years, unresponsive to systemic amphotericin B and itraconazole. Further investigations revealed CARD9 mutation and phaeohyphomycosis caused by the pigmented fungus Exserohilum rosatratum. Lesions subsequently improved with oral flucytosine and itraconazole.
Keywords
Exserohilum rosatratum
phaeohypomycosis
CARD9
Introduction
The term phaeohyphomycosis, coined by Ajello et al. in 1974,1 refers to infections caused dematiaceous fungi belonging to a diverse group of organisms found in the soil, plants and organic debri.2 The major etiologic agents include Bipolaris, Exophiala, Curvularia, Exserohilum and Wangiella species. These fungi can infect the skin and subcutaneous tissue along with paranasal sinuses, eyes, bones or central nervous systemThese infections usually result from inconspicuous penetrating injuries. The common presentations include a solitary cutaneous nodule, plaque or deep-seated subcutaneous cyst or abscess localized to the exposed areas of body, especially the extremities.2
Susceptibility to fungal infections in otherwise healthy individuals with Mendelian disorders is being increasingly recognized due to widespread genome sequencing. Primary immunodeficiencies, characterized by various genetic defects hinder the proper development of innate and adaptive immunity. Caspase recruitment domain-containing protein 9 (CARD9) is an important regulator of innate immunity, present in neutrophils, macrophages and dendritic cells. Thus, mutations involving the CARD9 gene can lead to severe immunosuppression resulting in severe disseminated infections.3
We report this case of Amphotericin B non-responsive disseminated subcutaneous phaeohyphomycosis caused by Exserohilum rostratum, in a patient with novel CARD9 mutation.
Case Report
A 26-year-old married woman, agriculturist by profession, presented with several skin lesions affecting her face and extremeties for the last seven years; gradually increasing in size. There was no past history of known trauma. She was afebrile without any history of significant medical illness. Four years back she was prescribed anti-tubercular drugs (ATD) for nine months without any improvement of her skin lesions. Surgical excision was followed by recurrence of lesions at the same sites and distant places within six months. She also received two cycles of intravenous amphotericin B for 26 days each five months apart along with oral itraconazole, 200 mg twice daily for eight months with minimal improvement.
Cutaneous examination revealed multiple grouped, skin-colored to hyperpigmented, verrucous papules, nodules and plaques, diameters ranging from few mm to 6 cm, affecting the bilateral forearm, right knee, left leg and right cheek [Figures 1 and 2]. They were non-tender and soft to firm on palpation. No lymphadenopathy was noted.

- Well-defined, erythematous plaque on the right cheek extending to nose and chin

- Multiple grouped. verrucous, papules, nodules and plaques on bilateral forearm, right knee and left leg
Clinically, chromoblastomycosis, phaeohyphomycosis, tuberculosis verrucous cutis and atypical mycobacterial infections were considered as the differentials.
Routine biochemistry including blood sugar and serum electrolytes was within normal limits. Serum was negative for HBV, HCV and HIV viral markers.
Histological examination of a representative papule (right arm) demonstrated pseudo-epitheliomatous hyperplasia with nodular granulomatous infiltrate in the dermis and multiple pigmented septate hyphae [Figure 3].
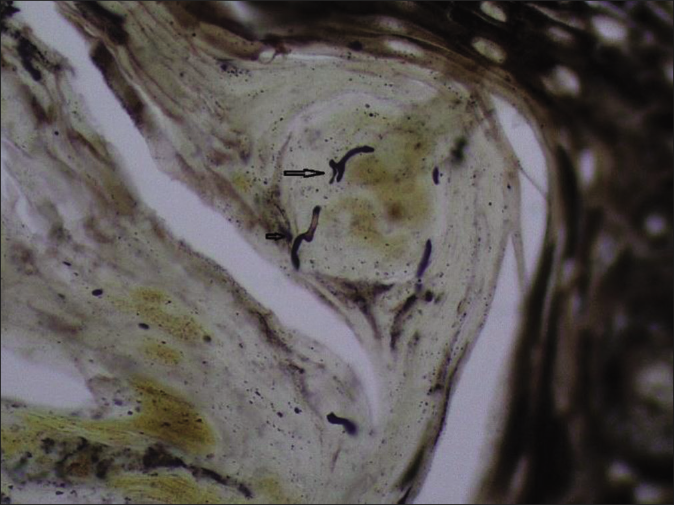
- Pigmented, septate hyphae in the stratum corneum (Gomori methenamine-silver nitrate stain GMS stain, x100)
Tissue for fungal culture yielded growth within seven days on Sabouraud’s dextrose agar. Colonies were grey to olive-brown with cottony texture and black reverse pigmentation. Slide culture showed septate hyphae. The conidiophores were long with multiple septae demonstrating sympodial geniculate growth with knobby, zigzag appearance.The conidia were elliptical with transverse septations and distinct protruding hilum at their base [Figure 4]. All these features were suggestive of the pigmented fungus Exserohilum rostratum.

- Conidia with protruding hilum (arrow) (Lactophenol cotton blue stain LCB,×100)
The lymphocyte sub-population analysis and nitro blue tetrazolium test were normal. Her serum IgE was raised (9350 IU/L). Primary immunedeficiency gene panel by next-generation sequencing detected a homozygous non-sense variation in exon 8 of the CARD9 gene HMZ p.Q370X (c.1108C>T). A whole-body CT scan (brain, chest, abdomen and pelvis) failed to show any systemic involvement.
She was administered a combination therapy of oral itraconazole 200 mg twice daily with oral flucytosine 500 mg four times daily resulting in significant improvement of her lesions within one month. [Figure 5]. Notably she failed to respond to intravenous Amphotericin B previously. We advised regular follow-up to assess the long-term therapeutic response.

- Significant improvement after 1 month of treatment
Discussion
Phaeoid fungi can cause a diverse group of infections including chromoblastomycosis (characteristic sclerotic bodies in tissue), eumycetoma (secretion of black coloured grains from the lesions) and hence, phaeohyphomycosis is a term used for other clinical presentations caused by dematiaceous fungi which form yeast-like cells, pseudohyphae, hyphae or a combination of these in the infected tissues.4
CARD9 deficiency is an autosomal-recessive disorder. Mutations in CARD9 (a key regulator of innate immunity) lead to impaired synthesis of pro-inflammatory cytokines resulting in depressed Th17- and Th22-associated anti-fungal response.5 Till now, 24 different genetic alterations in CARD9 have been described in 60 patients with fungal infections like candidiasis, dermatophytosis, phaeohyphomycosis and invasive aspergillosis resulting in CARD9 deficiency.3 This is the first Indian case of phaeohyphomycosis with a novel genetic alteration in the CARD9 gene.
The treatment of phaeohyphomycosis varies depending on their clinical presentation. Localized lesions respond to surgical excision and cryotherapy. Itraconazole and voriconazole demonstrate the most consistent in vitro activity against dematiaceous fungi while fluconazole has no role. Amphotericin B has good in vitro activity against most clinically important dematiaceous fungi. However, in vitro resistance and therapeutic failures have been reported with this drug. Flucytosine has an unique mechanism of action, inhibiting DNA and RNA synthesis. Combination therapy is often useful for refractory cases.6
Therapeutic success depends on the time of diagnosis, extent of lesions, comorbidities, the choice of anti-fungal drug and host immune status. Patients with CARD9 deficiency are often recalcitrant to conventional antifungal ltherapy.5 The use of sub-cutaneous granulocyte colony-stimulating factor as adjunctive immunomodulator in CARD9-deficient patients with CNS infection by Candida species has been described.7
In a review of 48 cases of phaeohyphomycosis caused by Exserohilum, immunosuppression (27.2%) was the commonest underlying condition followed by trauma (16.6%) and atopy (12.5%). Systemic involvement was reported in 73% patients while cutaneous (25%), corneal (16.7%) and subcutaneous (10.4%) infection were also recorded.8 There are two prior reports of subcutaneous phaeohyphomycosis due to Exserohilum rostratum from India.9,10
The underlying immunological mechanisms, particularly CARD9 mutation needs to be investigated in such apparently healthy patients with atypical, disseminated and refractory fungal infections. A multidisciplinary approach involving immunologists, microbiologists and dermatologists is necessary to gain newer insights into host immune response against fungi which may facilitate the development of newer and effective therapeutic strategies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A case of phaeohyphomycosis caused by a new species of Phialophora. Mycologia. 1974;66:490-8.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous phaeohyphomycosis in an immunocompetent Individual: A case report. Indian Dermatol Online J. 2017;8:29-31.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency and geographic distribution of CARD9 mutations in patients with severe fungal infections. Front Microbiol. 2018;9:2434.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated cutaneous phaeohyphomycosis due to Cladophialophora bantiana. Indian J Dermatol Venereol Leprol. 2015;81:491-4.
- [CrossRef] [PubMed] [Google Scholar]
- Phaeohyphomycosis caused by Phialophora americana with CARD9 mutation and 20 year literature review in China. Mycoses. 2019;62:908-19.
- [CrossRef] [PubMed] [Google Scholar]
- Successful Granulocyte colony stimulating factor treatment of relapsing Candida albicans meningoencephalitis Caused by CARD9 Deficiency. Pediatr Infect Dis J. 2016;35:428-31.
- [CrossRef] [PubMed] [Google Scholar]
- Exserohilum infections: Review of 48 cases before the 2012 United States outbreak. Med Mycol. 2014;52:376-86.
- [CrossRef] [PubMed] [Google Scholar]
- A case of subcutaneous phaeohyphomycosis caused by Exserohilum species in an immunocompromised patient. Our Dermatol Online. 2013;4:498-500.
- [CrossRef] [Google Scholar]
- A case of cutaneous phaeohyphomycosis caused by Exserohilum rostratum, its in vitro sensitivity and review of literature. Mycopathologia. 1995;131:9-12.
- [CrossRef] [PubMed] [Google Scholar]






