Translate this page into:
A case of eyelid capillary telangiectasia in juvenile clinically amyopathic dermatomyositis
Corresponding author: Dr. Biswanath Behera, Department of Dermatology, AIIMS, Sijua, Patrapada, Bhubaneswar, Odisha, India. biswanathbehera61@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gowda SK, Behera B, Ameta B, Priyadharsan B, Patel RK. A case of eyelid capillary telangiectasia in juvenile clinically amyopathic dermatomyositis. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1407_2024
Dear Editor,
A seven-year-old boy was brought by his parents with a complaint of asymptomatic hyperpigmentation of both upper eyelids for two months. Parents denied preceding history of redness or swelling of the eyelid, face or other body areas. There was no history of atopy, photosensitivity, oral ulcers, recurrent angioedema or usage of eye drops. The child did not have any systemic complaints, including muscle weakness. Close examination revealed an arborising telangiectasia and a faint confluent erythematous macule on the bilateral upper eyelids [Figure 1a]. In addition, a solitary whitish papule 3 mm in size was noted on the lateral aspect of the right eyelid. Rest of the cutaneous examination revealed 2–5 mm skin-coloured, discrete, flat-topped, firm papules on the dorsal aspect of the bilateral elbows, knee, metacarpophalangeal, proximal and distal interphalangeal joints [Figure 1b] without significant erythema or oedema. A differential diagnosis of juvenile dermatomyositis (JDM), reticulate lichen planus pigmentosus were considered. Dermoscopy of the eyelid using Heine Delta 20T revealed an arborising telangiectatic vessel, linear white structureless areas and blue-gray globules in a rhomboid pattern and yellow-white structureless area suggestive of calcinosis cutis [Figures 2a and 2b]. Investigations revealed antinuclear antibody titer 1:100 with a speckled pattern, normal calcium, creatine phosphokinase levels, lactate dehydrogenase and serum glutamic oxaloacetic transaminases. Electromyography, echocardiography and chest X-ray were normal. A roentgenogram of the elbow revealed radiopaque shadows over the posterior aspect of the left elbow suggestive of calcinosis cutis [Figure 3]. Based on these findings, a myositis profile was done, that was positive for anti-transcription intermediary factor 1-gamma (TIF1γ). A final diagnosis of juvenile clinically amyopathic dermatomyositis (JCADM) was considered. Patient was started on topical steroids and methotrexate 10 mg once per week for both cutaneous signs and calcinosis cutis.

- Arborizing telangiectasia (black circle), faint confluent erythematous macule and yellow white firm papule over right eyelid.

- Discrete, flat-topped, firm papules over the bilateral metacarpophalangeal joints and proximal and distal interphalangeal joints.
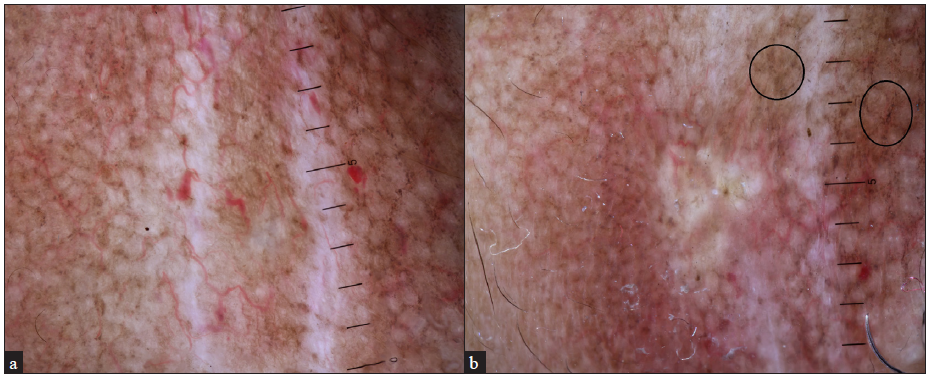
- (a) Dermoscopy reveals an arborising telangiectatic vessel, linear white structureless areas and Brown grey globules in a rhomboid pattern suggestive of poikiloderma changes. (b) Yellow-white structureless area suggestive of calcinosis cutis (Hiene Delta 20T, Polarised mode, 10x).

- X-ray demonstrating radiopaque mass over extensor of left elbow.
The diagnosis of childhood periorbital poikiloderma (eyelid telangiectasia) can be challenging as it can be due to various inherited and acquired conditions. Inherited disorders with poikiloderma predominantly on the face are Rothmund-Thomson syndrome and Kindler syndrome. Acquired conditions such as dermatomyositis (DM), systemic lupus erythematosus, graft versus host disease, drug or radiotherapy induced and poikiloderma of Civatte present as poikiloderma on the face.1 JDM is a rare autoimmune multisystem disease characterised by vasculopathy of skin with or without muscle involvement, resulting in a confluent macular erythematous cutaneous eruption and symmetrical proximal myopathy.2,3 Our case was unique due to the absence of muscle weakness, pathognomic cutaneous features of DM. The boy presented with upper eyelid telangiectasia and macular hypo- and hyperpigmentation, different from the commonly encountered periorbital heliotrope rash.
Poikiloderma atrophicans vasculare is classically described over the neck and back and is defined as the ‘V’ sign and shawl sign, categorised as compatible signs of DM. In a prospective cohort study by Wang et al., eyelid margin capillary dilation (61.37%), periungual telangiectasia (51.8%), erythema (43.9%) and palatal vessel dilatation (30.5%) were seen among 145 JDM cases.4 Thereby, telangiectasias at specific sites such as palate, periungual, and periorbital constitute one of the factors for monitoring the disease activity of JDM.5 Other factors determining the activity of JDM included skin erythema and Gottron papules. This study did not analyse whether these microvascular changes are predominant in clinically amyopathic DM (CADM). Periorbital calcinosis is extremely rare and has not been described in DM to date; it is classically seen in patients with periorbital syringomas.6 The causes of dystrophic calcinosis cutis in pediatric age include Ehler-Danlos syndrome, pseudoxanthoma elasticum, Werner syndrome, juvenile dermatomyositis, systemic sclerosis and systemic lupus erythaematosus, while metastatic calcinosis is seen in Albright hereditary osteodystrophy, sarcoidosis, milk-alkali syndrome, hypervitaminosis D and chronic renal failure.6
Autoantibodies against TIF1γ are of clinical significance in both JDM and adult DM and its presence indicates extensive erythematous cutaneous involvement over the ‘V’ area of the neck, shoulders, face and hands. It has been linked with hypomyopathic disease, telangiectasia (seen in our case), ovoid palatal patches and palmar hyperkeratosis. Though there is risk of both solid and haematological malignancies in adults with these autoantibodies, no such relationship was observed in pediatric population.3 Topical steroids/tacrolimus forms the first line treatment for cutaneous manifestations, and hydroxychloroquine 5 mg/kg/day as the 2nd line. If no response is observed after three months of therapy, methotrexate, mycophenolate mofetil or intravenous immunoglobulin may be considered.7
In conclusion, we report this case due to the rare presentation of CADM as eyelid telangiectasia and calcification. We also wanted to highlight the presence of eyelid telangiectasia as a clinical marker of disease activity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Inherited skin disorders presenting with poikiloderma. Int J Dermatol. 2021;60:1343-53.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and prevalence of inflammatory myopathies: A systematic review. Rheumatology (Oxford). 2015;54:50-63.
- [CrossRef] [PubMed] [Google Scholar]
- Reply to: ‘Comment on ‘Dermatomyositis-Clinical features and pathogenesis’. J Am Acad Dermatol. 2020;83:e23.
- [CrossRef] [PubMed] [Google Scholar]
- Skin disease is more recalcitrant than muscle disease: A long-term prospective study of 184 children with juvenile dermatomyositis. J Am Acad Dermatol. 2021;84:1610-8.
- [CrossRef] [PubMed] [Google Scholar]
- Juvenile dermatomyositis: advances in pathogenesis, assessment, and management. Curr Pediatr Rev. 2021;17:273-87.
- [CrossRef] [PubMed] [Google Scholar]
- Characterizing calcinosis cutis in a pediatric population. Pediatr Dermatol. 2020;37:317-9.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment challenges in clinically amyopathic dermatomyositis: A case series and review of new therapeutic options for skin involvement. Dermatol Ther. 2021;34:e14942.
- [CrossRef] [PubMed] [Google Scholar]





