Translate this page into:
A case of metastatic malignant melanoma in congenital systemic dermal melanocytosis
Correspondence Address:
Sung-Ae Kim
Department of Dermatology, School of Medicine, Keimyung University, 1095 Dalgubeol-Daero, Dalseo-Gu, Daegu 42601
Korea
| How to cite this article: Kim WO, Ryoo YW, Kim SA. A case of metastatic malignant melanoma in congenital systemic dermal melanocytosis. Indian J Dermatol Venereol Leprol 2020;86:308-311 |
Sir,
Dermal melanocytoses are characterized by the presence and increased number of melanin-producing dendritic melanocytes in the dermis.[1] Malignant transformation of dermal melanocytosis is very rare and there has been only one prior report of malignant melanoma arising in a case of disseminated dermal melanocytosis.[2]
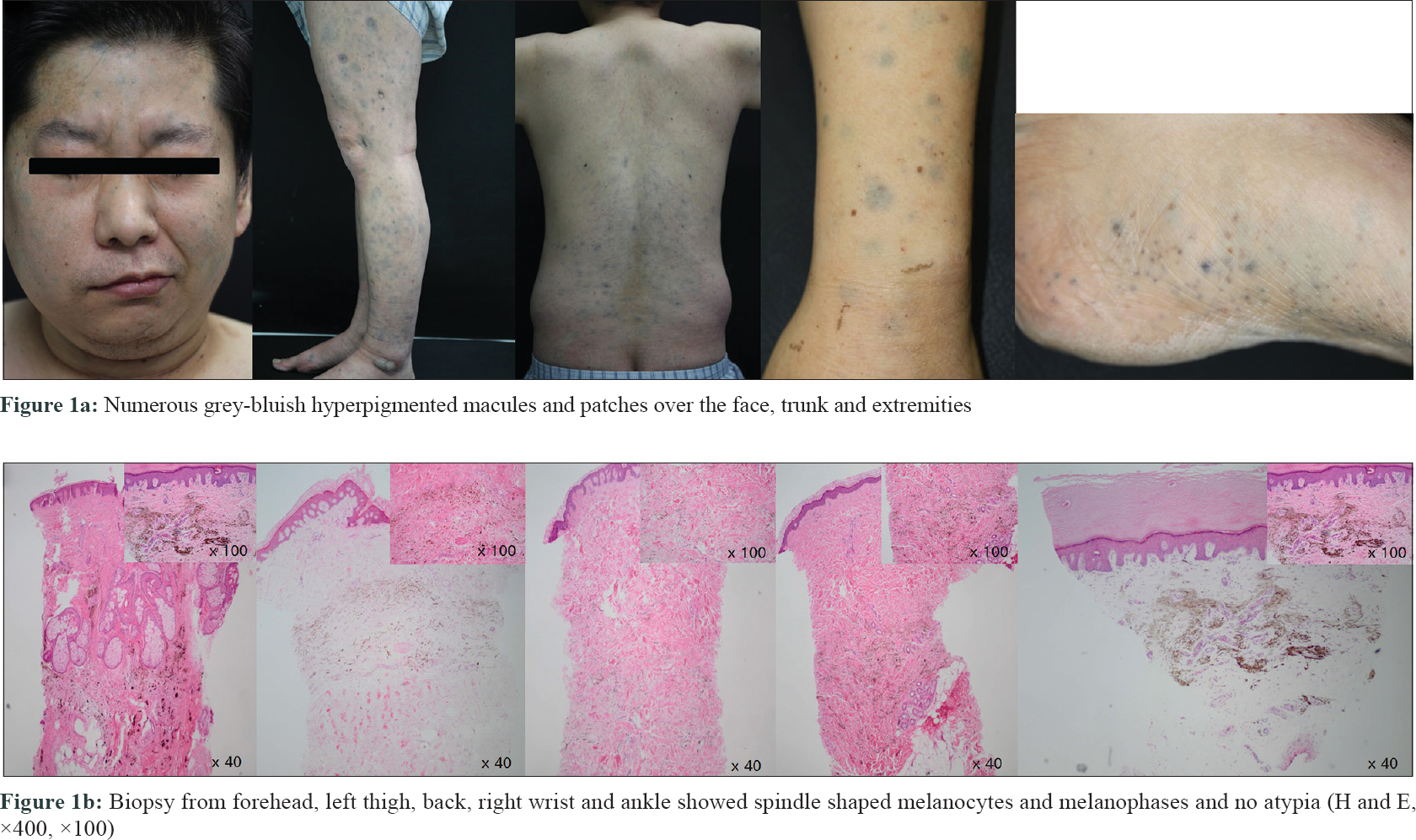
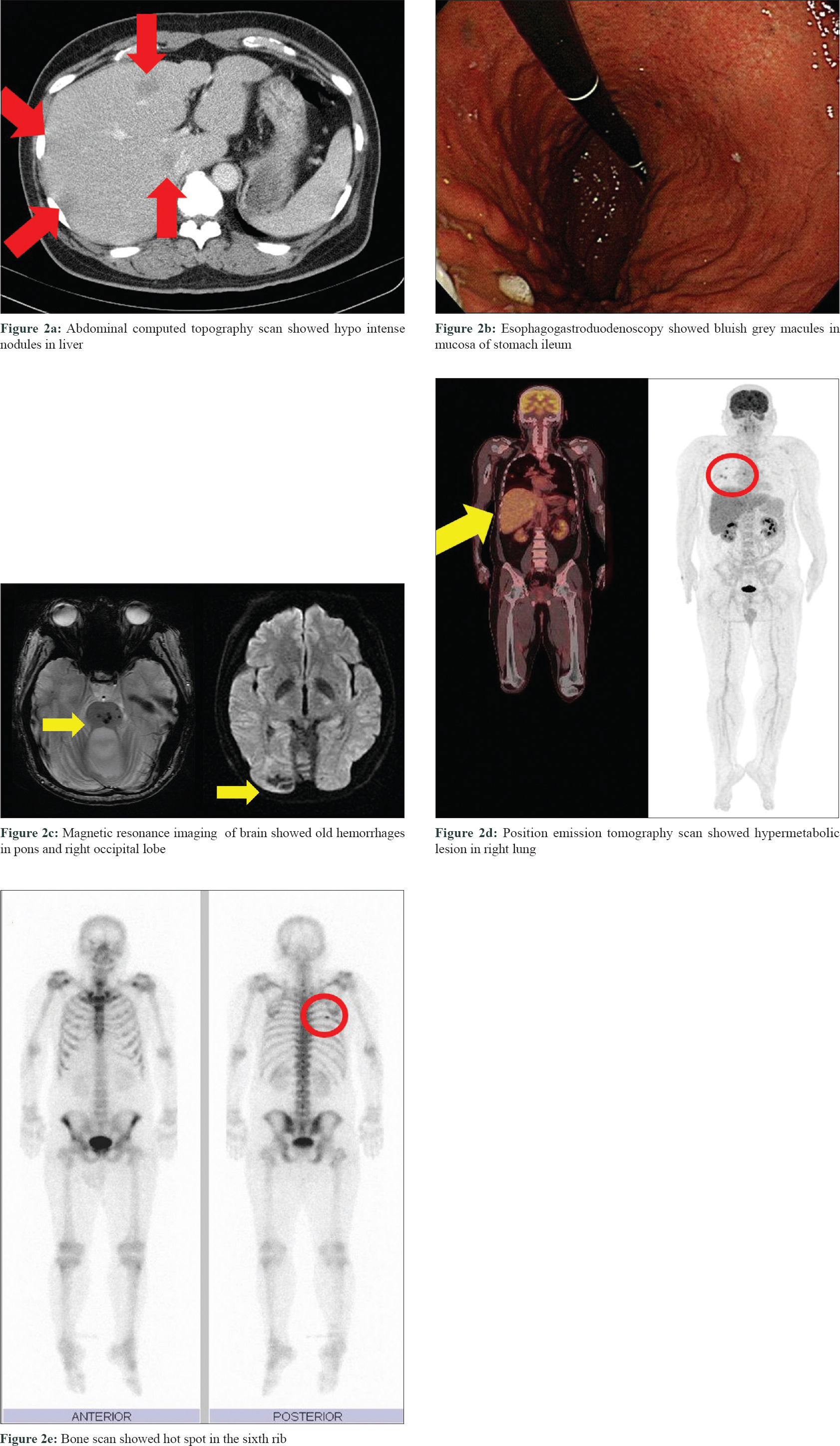
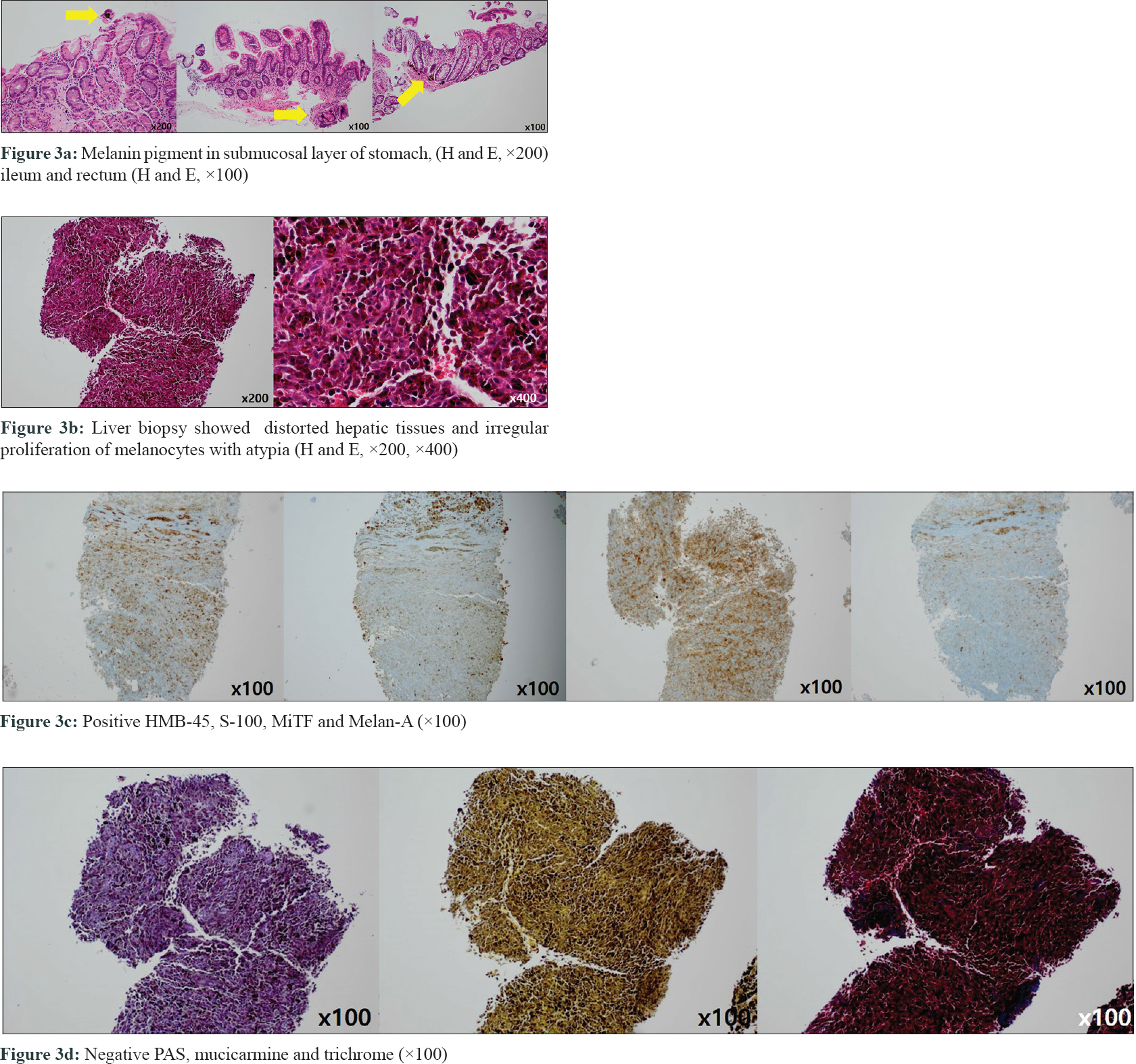
A 42-year-old man presented with numerous bluish-grey hyperpigmented macules and patches on the face, trunk and both extremities since birth [Figure - 1]a. He had fever and abdominal pain for the past 4 days. On physical examination, he had abdominal distension and right sided facial palsy. Abdominal computed tomography scan showed hypointense nodules in the liver which were biopsied [Figure - 2]a. Esophagogastroduodenoscopy and colonoscopy showed bluish grey macules in the mucosa of the stomach, ileum and rectum. Biopsies were done from each site [Figure - 2]b. On histopathology, melanin pigment was seen in the submucosal layer [Figure - 3]a. Liver biopsy showed distorted hepatic tissues and irregular, abnormal proliferation of melanocytes with atypia [Figure - 3]b. Immunohistochemistry was positive for HMB-45, S-100, MiTF and Melan-A [Figure - 3]c and negative for periodic-acid-S chiff, mucicarmine and Masson's trichrome [Figure - 3]d.
 |
| Figure 1: |
 |
| Figure 2: |
 |
| Figure 3: |
Magnetic resonance imaging of the brain showed no intracranial metastasis, except for the old microhemorrhages in the pons and subacute infarction with a hemorrhagic change in the right occipital lobe [Figure - 2]c. His right facial palsy was considered to have been contributed by multiple old microhemorrhages.
Positron emission tomography scan showed hypermetabolic lesions in the right lung and lower peribronchial area [Figure - 2]d. Bone scan showed a hot spot on the right sixth rib [Figure - 2]e. He was diagnosed with metastatic malignant melanoma and referred to our department to rule out primary cutaneous malignant melanoma.
Skin lesions were asymptomatic and there was no recent change in size, color or number of lesions. On examination there was no evidence of malignant change like ugly-duckling sign. Skin biopsy was done from the five most suspicious and variable lesions (on the forehead, left thigh, back, right wrist and left ankle). Biopsy showed pigmented spindle-shaped melanocytes with no atypia and melanophages in all five lesions [Figure - 1]b. He was finally diagnosed with metastatic malignant melanoma with the unknown primary site. He underwent nivolumab chemotherapy but died 2 months later due to hepatic failure.
The etiology of dermal melanocytosis is not fully understood.[1],[3] The arrest of melanocyte migration from neural crest to interfollicular and follicular epidermis is believed to be responsible.[1] While malignant transformation has been reported in blue nevus, nevus of Ota and Ito; malignant melanoma arising from other types of dermal melanocytosis has never been reported.[2],[4] Except by Levene, where no primary site was discovered.[2] In our case also, we did not find the primary focus of malignant melanoma in the skin lesions. However, we consider it is reasonable to believe the malignant transformation arose from the skin lesions of melanocytosis.
In 1948, Carleton and Biggs described a 14-year-old girl with profuse bluish spots covering her entire skin surface since the age of 3 years.[5] Later, in 1979, the evolution of this case was reported by Levene.[2] At the age of 43, she had developed metastatic malignant melanoma involving the lymph nodes and liver but no primary site was identified. She died soon after admission and autopsy demonstrated widespread dermal, visceral and cranial melanosis. This is the only case in the literature of disseminated dermal melanocytosis with malignant melanoma.[2]
Mutations in the guanine nucleotide-binding protein q polypeptide gene (GNAQ) and guanine nucleotide-binding protein alpha 11 genes (GNA11) have been described in mice with dermal melanocytosis and mutations in GNAQ also have been demonstrated in humans with dermal melanocytosis and uveal melanoma.[3]CDKN2A, BRAF, N-RAS and KIT mutations are found in malignant melanoma.[3] Since no direct relation or common gene mutation has been demonstrated between dermal melanocytosis and malignant melanoma, further study of the pathogenesis of dermal melanocytosis and association with malignant melanoma will be required. Our patient did not undergo any genetic studies except for the negative BRAF mutation.
Through careful consideration, we reached a diagnosis of “congenital systemic dermal melanocytosis” since skin lesions were present since birth and were disseminated throughout the skin. Systemic involvement was diagnosed in view of the grey-bluish macules in hollow organs such as the stomach, small and large intestines. Finally, a skin biopsy showed dermal melanocytosis.
In conclusion, it is important to look for malignant transformation in cutaneous and extracutaneous sites in a patient of systemic dermal melanocytosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIP) (No. 2014R1A5A2010008).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Franceschini D, Dinulos JG. Dermal melanocytosis and associated disorders. Curr Opin Pediatr 2015;27:480-5.
[Google Scholar]
|
| 2. |
Levene A. Disseminated dermal melanocytosis terminating in melanoma. A human condition resembling equine melanotic disease. Br J Dermatol 1979;101:197-205.
[Google Scholar]
|
| 3. |
Pessach Y, Goldberg I, Sprecher E, Gat A, Harel A. An unusual presentation of congenital dermal melanocytosis fitting the rare diagnosis of dermal melanocyte hamartoma. Cutis 2014;94:E16-7.
[Google Scholar]
|
| 4. |
Tse JY, Walls BE, Pomerantz H, Yoon CH, Buchbinder EI, Werchniak AE, et al. Melanoma arising in a nevus of Ito: Novel genetic mutations and a review of the literature on cutaneous malignant transformation of dermal melanocytosis. J Cutan Pathol 2016;43:57-63.
[Google Scholar]
|
| 5. |
Carleton A, Biggs R. Diffuse mesodermal pigmentation with congenital cranial abnormality. Br J Dermatol Syph 1948;60:10-3.
[Google Scholar]
|
Fulltext Views
3,398
PDF downloads
2,437





