Translate this page into:
A case report of lichen nitidus: From classical to perforating
Corresponding author: Dr. Huan Wang and Zhifang Zhai, Department of Dermatology, Southwest Hospital, Army Medical University, Chongqing, China. wanghuan20061228@163com and zhaizf1004@163.com
-
Received: ,
Accepted: ,
How to cite this article: Zhang M, Li J, Zhou X, Zhang L, Wang H, Zhai Z. A case report of lichen nitidus: From classical to perforating. Indian J Dermatol Venereol Leprol. 2024;90:643-6. doi: 10.25259/IJDVL_457_2022
Dear Editor,
Lichen nitidus is a rare dermatosis characterised by multiple, discrete, pinpoint-sized, skin-coloured papules with flat, shiny surfaces, commonly occurring on the flexor surface of the upper limb, genitalia, chest, abdomen and dorsum of the hand. The histological characteristics comprise a dense, sharply circumscribed infiltrate composed of lymphocytes, epithelioid cells and Langhans giant cells. Elongated rete ridges adhere to and surround the infiltrate, in a “ball-in-claw” configuration that is usually confined to two or three dermal papillae. Lichen nitidus variants include the linear, spinous follicular, generalised, actinic and perforating types. Here, we report a case of lichen nitidus in which classical and perforating lesions appeared successively.
An otherwise healthy 24-year-old Chinese Han man presented with an asymptomatic papule on the upper limb that had persisted for 1 year. Physical examination revealed multiple, discrete, pinpoint-to-small, rice grain-sized, skin-coloured, firm, shiny, monomorphic papules on his left wrist [Figure 1a]. Skin biopsy revealed a dense, superficial lymphohistiocytic infiltrate bounded by elongated rete ridges in a broadened dermal papilla [Figure 1b]. He was diagnosed with lichen nitidus and administered topical flumetasone ointment twice daily and tazarotene gel every night for 6 months. The lesions subsided completely following the treatment. However, he returned to our clinic 10 months later with similar lesions on both palms. These lesions had coalesced into patches with umbilicated centres [Figure 1c]. Dermoscopy revealed a yellowish-brown central keratotic core with marginal lifting, surrounded by annular, pale white halo-like scales [Figure 1d]. Reflectance confocal microscopy showed three concentric areas with elliptical, poorly refractile centre, an irregular brightly refractile area and a peripheral halo with poorer refraction [Figure 1e]. Punch biopsy of the left palm revealed a dense lymphohistiocytic infiltrate covered by atrophic epidermis and bounded by elongated rete ridges in a broadened dermal papilla. Keratin and lymphohistiocytic cells extended to the surface via a transepithelial perforation channel [Figure 1f]. Masson-trichrome stain identified no transepithelial collagen migration. The final diagnosis was perforating lichen nitidus [Figure 1g]. He was prescribed betamethasone dipropionate cream twice daily and 0.1% tretinoin cream every night for 4 weeks. The lesions showed slight improvement and regular follow-up is ongoing.

- Multiple, small, skin-coloured, shiny papules on the wrist (indicated by red arrow).
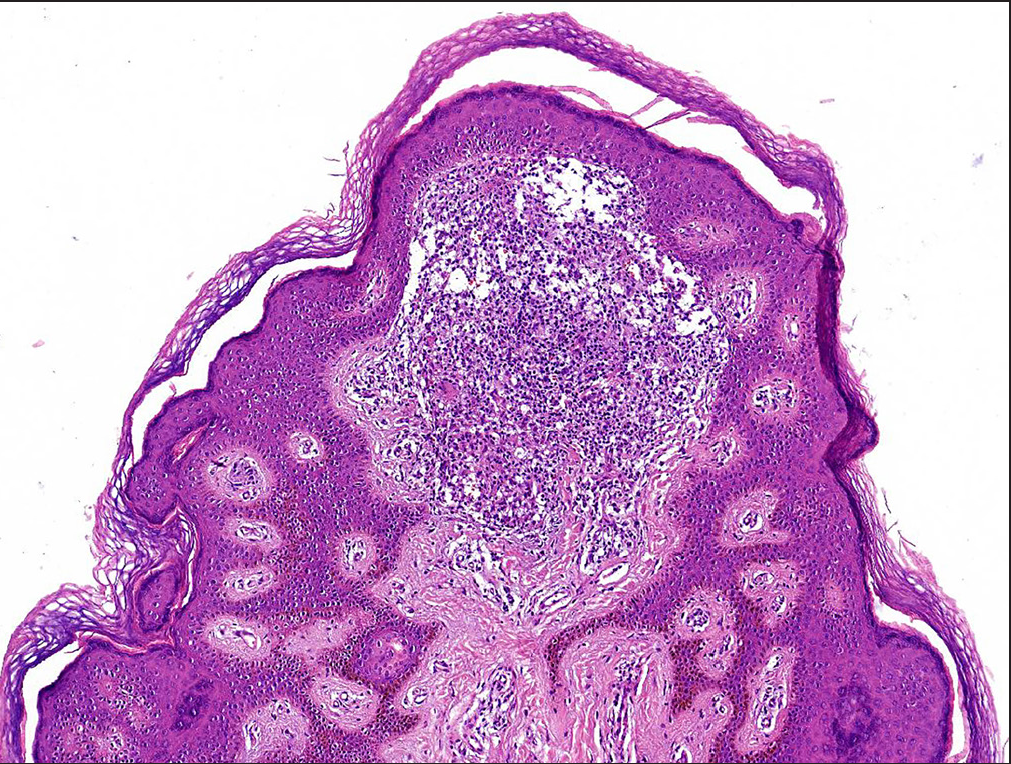
- A dense, superficial lymphohistiocytic infiltrate bounded by elongated rete ridges (H&E, 100x).
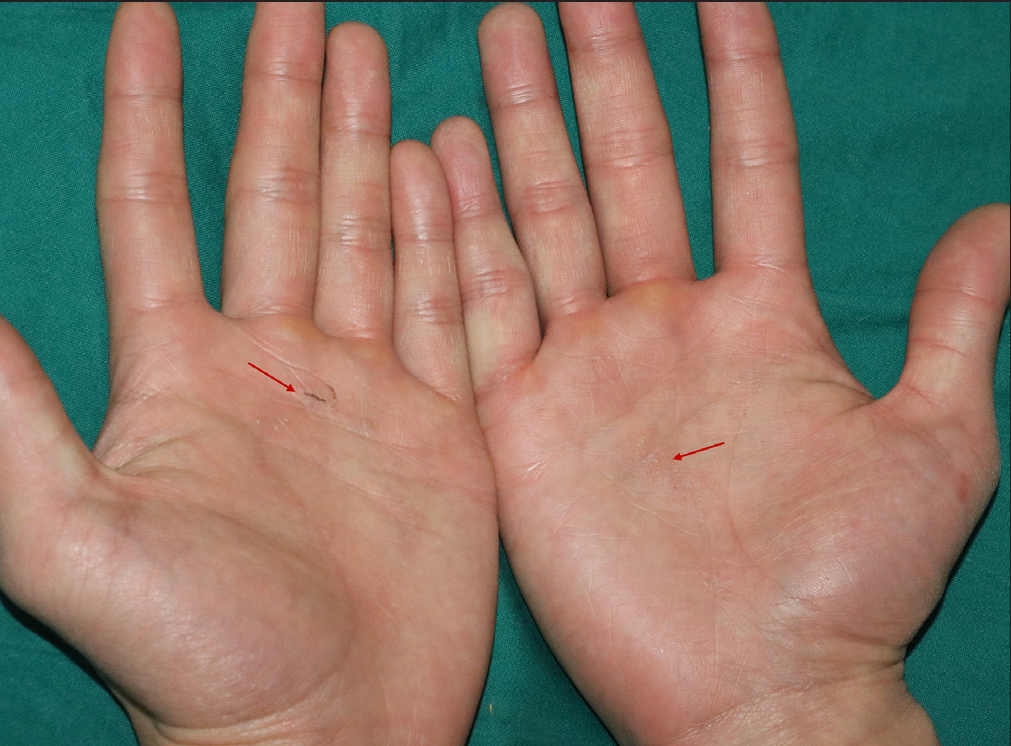
- Umbilicated papules coalesced into patches on both palms (indicated by red arrow).

- Dermoscopy: yellowish-brownish central keratotic core with marginal lifting, surrounded by annular, pale white halo-like scales (50x).
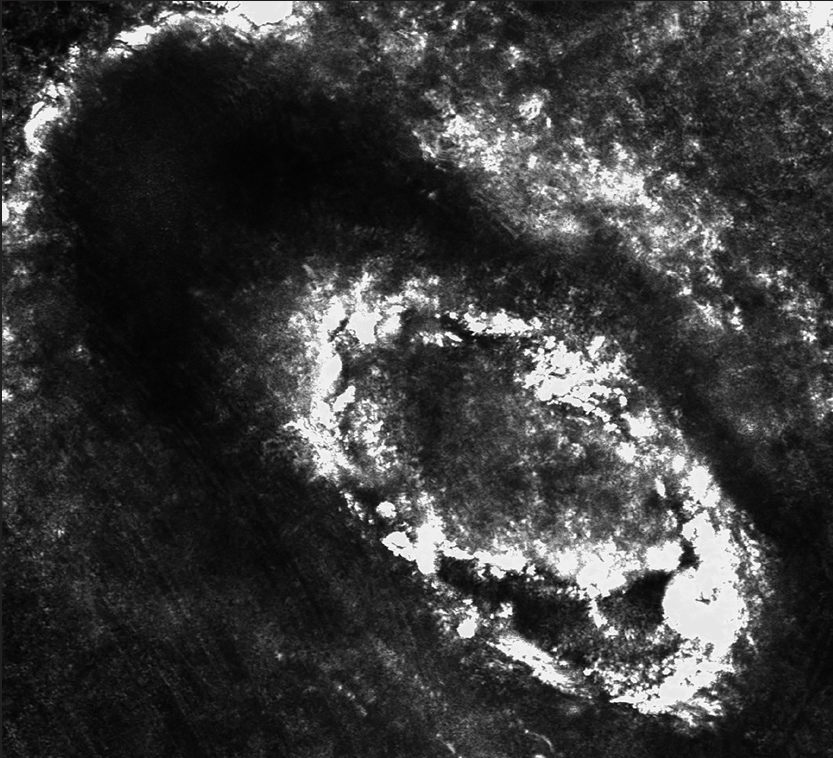
- Reflectance confocal microscopy: three concentric areas with elliptical poorly refractile centre, an irregular brightly refractile area and a peripheral halo with poorer refraction.
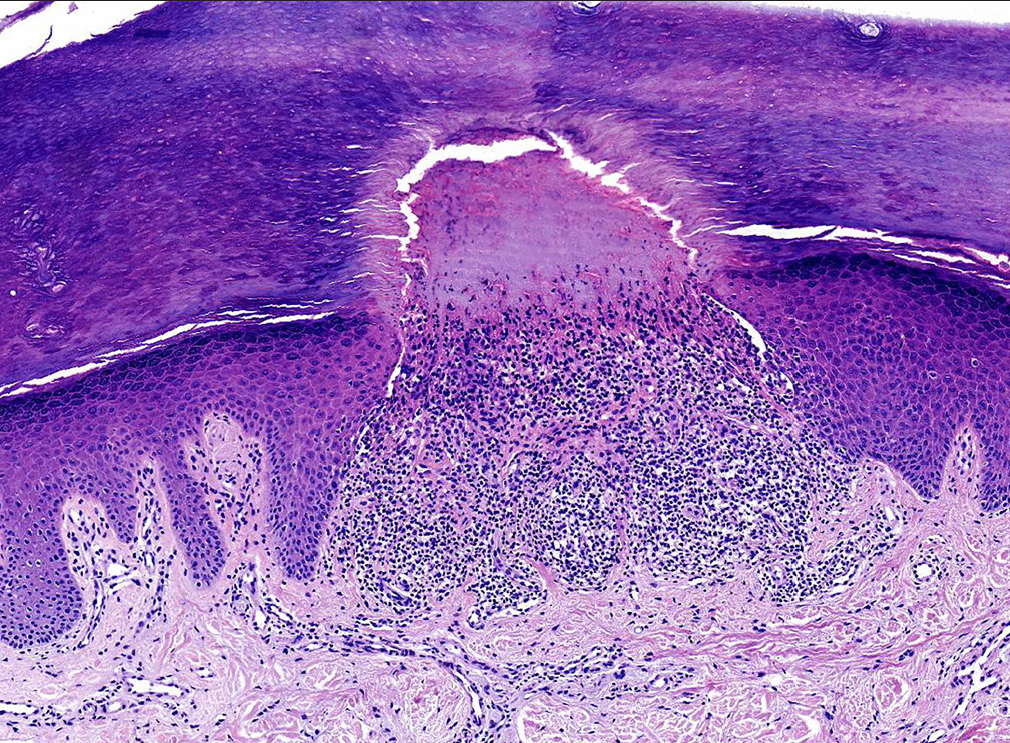
- A dense lymphohistiocytic infiltrate covered by atrophic epidermis and bounded by elongated rete ridges in a broadened dermal papilla. Keratin and lymphohistiocytic cells extended to the surface via a transepithelial perforation channel (H&E, 100x).
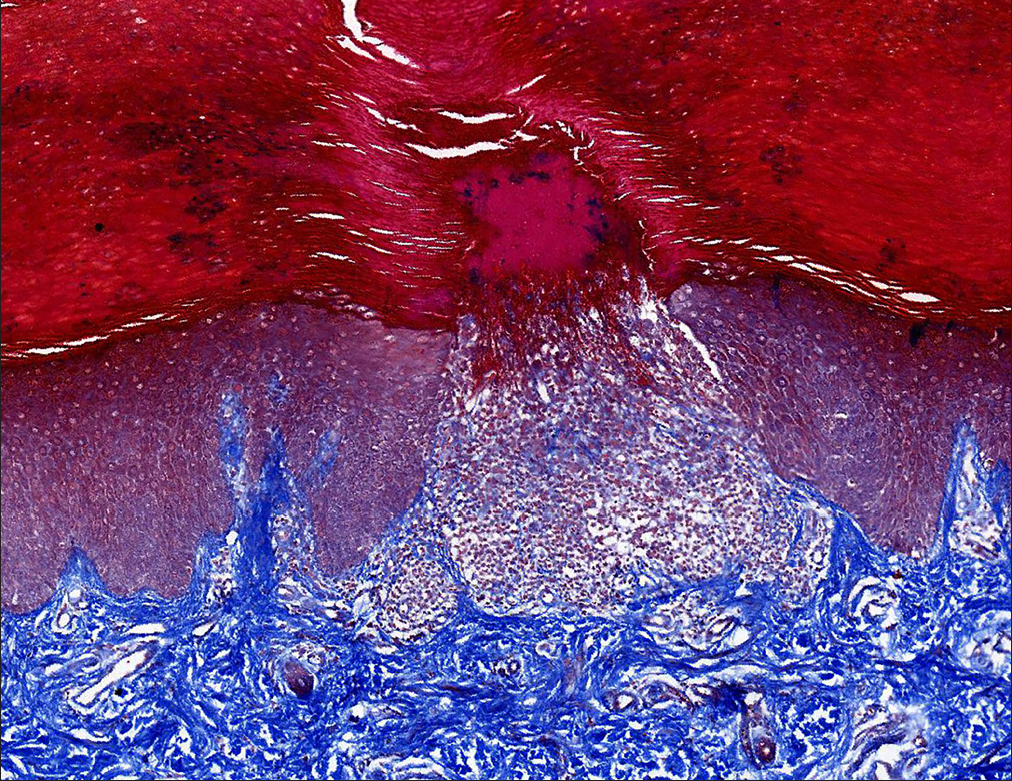
- No extrusion of collagen fibres in the perforating channel (Masson stain, 100x).
Perforating lichen nitidus is a rare clinical variant first reported in 1981 by Bardach. 1 Only 13 cases, including ours, have been described to date. 1–11 The characteristics of the disease are summarised in Table 1, according to our systematic literature review. Perforating lichen nitidus occurs most commonly in children and young adults, with 10 (76.9%) patients aged 10–30 years. The 13 reported cases comprised eight Asians, four Caucasians and one African-American. Perforating lichen nitidus lesions are similar to classical lichen nitidus lesions except for the appearance of central umbilicated papules seen in seven (53.9%) cases. According to previous reports 9–11 and our findings, dermoscopic findings of perforating lichen nitidus demonstrated a well-defined, light-brown keratin plug surrounded by a ring-shaped, silvery-white area, whereas classical lichen nitidus lesions usually defined with a round, elevated, shiny and smooth appearance.12 The most important histopathological feature is a transepidermal perforating channel that can extrude the dermal material into the stratum corneum. The treatment options for perforating lichen nitidus include topical glucocorticoids and tretinoin; however, in one patient, the lesions healed spontaneously. 4
| Cases | Ethnicity | Age (year)/Duration | Sex | Diseased parts | Lesion appearance | Dermoscopy | Therapy response |
|---|---|---|---|---|---|---|---|
| Bardach 1 | Caucasians | 8/Few months | Male | Trunk and extremities | Flat, shiny papules | None | None reported |
| Banse-Kupin et al. 2 | African American | 22/1 month | Male | Trunk, extremities and penis | Flesh-coloured, dome-shaped papules | None | None reported |
| Itami et al. 3 | Asian | 32/3 years | Male | Hand and fingers | Discrete, pinhead-sized or half-rice corn-sized, flesh-coloured papules | None | None reported |
| Yoon et al. 4 | Asian | 18/2 years | Female | Hands, wrists, forearms, elbows and knees | Skin-coloured, flat shiny papules | None | Improvement after topical steroid for 1 year |
| Yoon et al. 4 | Asian | 20/11 months | Female | Wrists, elbows, knees and dorsal feet | Flat shiny papules, some of them were umbilicated | None | Spontaneous clearance |
| Arrue et al. 5 | Caucasians | 35/>20 years | Male | Palms, feet and lateral border fingers | Skin-coloured, shiny, firm, monomorphic papules | None | No response to topical corticosteroid |
| Vijaya et al. 6 | Asian | 14/6 months | Female | Dorsum of the hands and feet | Small, shiny papules, some of them were umbilication | None | None reported |
| Zhang et al. 8 | Asian | 15/5 years | Male | Right palm | Small, skin-coloured papules with central umbilication | None | None reported |
| Zussman et al. 7 | Caucasians | 25/1 year | Male | Dorsal digit | Small papules grouped into patches | None | No response to topical acid wraps or clobetasol spray |
| Martinez-Mera et al. 9 | Caucasians | 30/1 year | Male | Dorsal of hands and fingers | Umbilicated papules grouped into patches | Light-brown keratin plug surrounded by a whitish, annular cloud-like area | Slightly improvement to topical corticosteroid for several weeks |
| Li et al. 11 | Asian | 10/2 years | Male | Upper extremities, trunk, lower jaw, and nape | Numerous, flesh-coloured, shiny papules, some of them were umbilicated | Whitish-brownish keratin plug in the centre, whitish annular cloud-like area and a peripheral brown pigmentation | Slightly improvement to topical corticosteroid for 2 weeks, but relapsed after discontinuation |
| LeWitt et al. 10 | Asian | 32/2 months | Male | Dorsal of hands and feet, palms, soles | Small white to pink molluscum-like umbilicated papules | Depressed central keratotic core rimmed by fine white scale | Significant improvement with topical corticosteroid for 6 weeks |
| Present case | Asian | 24/10 months | Male | Palms | Umbilicated papules grouped into patches | Yellowish-brownish keratotic core surrounded by pale-white halo-like scales | Slight improvement with topical corticosteroid for 4 weeks |
There are four documented cases of co-existence of classical and perforating lichen nitidus, including ours, suggesting that different types of lichen nitidus can occur in the same patient. 4,6,11 In addition, we performed the first reflectance confocal microscopy feature analysis of perforating lichen nitidus. The poorly refractile area in the centre corresponds to the histopathology of perforated keratin and lymphohistiocytic cells in the surface. The irregular, brightly refractile area correlates on histopathology with the fissure of the stratum corneum overlying the infiltrate. The peripheral halo with poorer refraction correlates with the adjacent stratum corneum. The reflectance confocal microscopy characteristics of perforating lichen nitidus differ from those of the classical type. 13
Several mechanisms, including an abnormality of epidermal proliferation and differentiation, alteration of connective tissues, mechanical disruption, participation of immunological factors and binding of altered dermal constituents or foreign bodies to some unidentified receptors have been proposed to explain the transepithelial perforation phenomenon. 3,14 However, given the paucity of documented cases, it is difficult to clarify the specific mechanism of perforation in lichen nitidus. Hence, the identification of more cases of this phenomenon will lead to a better understanding of its aetiology, pathophysiology and clinical course in future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work was supported by the National Science Foundation of Chongqing, China (no: cstc2021jcyj-msxmX0140).
Conflicts of interest
There are no conflicts of interest.
References
- Two cases of perforating lichen nitidus. J Dermatol. 2006;33:278-80.
- [CrossRef] [PubMed] [Google Scholar]
- [Perforating lichen nitidus on an atypical site] Actas Dermosifiliogr. 2009;100:429-31.
- [PubMed] [Google Scholar]
- Perforating lichen nitidus. Indian J Pathol Microbiol. 2010;53:162-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of a perforating lichen nitidus. Australas J Dermatol. 2018;59:61-2.
- [CrossRef] [PubMed] [Google Scholar]
- Perforating lichen nitidus. JAAD case reports. 2021;8:4-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopy of perforating lichen nitidus: A case report. Chin Med J (Engl). 2020;133:2135-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Different dermoscopic patterns of palmoplantar and nonpalmoplantar lichen nitidus. J Am Acad Dermatol. 2015;73:e101-e103.
- [CrossRef] [PubMed] [Google Scholar]
- In vivo reflectance confocal microscopy for evaluating seborrheic keratosis, verruca plana, syringoma and lichen nitidus. Skin Res Technol. 2021;27:272-6.
- [CrossRef] [PubMed] [Google Scholar]
- Transepidermal elimination: Historical evolution, pathogenesis and nosology. Indian J Dermatol Venereol Leprol. 2018;84:753-7.
- [CrossRef] [PubMed] [Google Scholar]





