A case series and literature review of erythema palmare hereditarium (Lane’s disease)
Corresponding author: Dr. Meryem Aktas, Marmara University, Istanbul, Turkey Marmara University Pendik Education and Research Hospital, Department of Dermatology Fevzi Cakmak , Muhsin Yazicioglu Street. No: 10 34899 Pendik, Istanbul, Turkey. meryemaktas72@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Özer EC, Demir G, Aktas M, Salman A. A case series and literature review of erythema palmare hereditarium (Lane’s disease). Indian J Dermatol Venereol Leprol 2021;87:64-6.
Sir,
Erythema palmare hereditarium, also known as Lane’s disease, is characterized by an early-onset palmar erythema in the absence of any underlying causes1 We believe that an increased awareness of this rarely-reported, or possibly under-recognized, entity is important to assure the patients and their families regarding the benign nature of erythema palmare hereditarium. Herein, we report two unrelated families with erythema palmare hereditarium and review the previously published data.
An 18-year-old lady presented with asymptomatic palmar erythema which was present since her childhood. Dermatological examination showed diffuse bilateral palmar erythema without any scaling [Figure 1a]. Family history revealed that her father had similar lesions on both palms as long as he could remember [Figure 1b].Telangiectasias on a homogenous pink background were noticed on dermoscopic examination [Figure 1c].

- Diffuse palmar erythema and telangiectasias

- Mild erythema and telangiectasias on her father’s palms
- Telangiectasias on a homogenous pink background on dermoscopy (Heine Delta 20, non-polarized dermoscope, ×10)
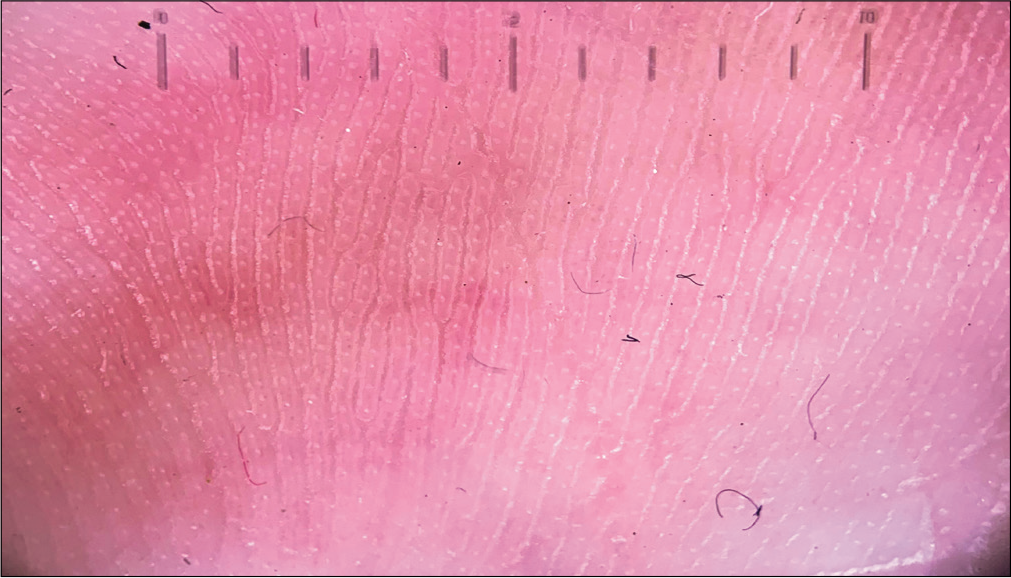
A 5-year-old girl presented with asymptomatic palmar redness. The lesions were first noticed shortly after her birth. The dermatological examination was normal except for the ill-defined erythematous patches on palms [Figure 2a]. Similar lesions were also evident on bilateral palms of her elder brother [Figure 2b]. Dermoscopic examination revealed homogenous pink-red areas [Figure 2c].

- Ill-defined erythema on palms

- Erythematous patches on the palms of her elder brother

- Telangiectasias on dermoscopy (Heine Delta 20, non-polarized dermoscope, ×10)
The other possible causes of palmar erythema, including pregnancy, liver dysfunction, connective tissue diseases and medications were excluded through a detailed history, physical examination and laboratory tests. The lesions were not associated with any physical stimuli such as changes in temperature. Therefore, a diagnosis of erythema palmare hereditarium were made based on the clinical, laboratory findings and positive family history in all patients. Palmar erythema may occur as a primary/physiologic condition or may be a cutaneous manifestation of hepatic, endocrine, autoimmune, infectious diseases or neoplasms. Primary or physiologic palmar erythema can be classified as idiopathic, pregnancy-related and hereditary, the latter being the most common form of primary palmar erythema among children.2
Erythema palmare hereditarium was first described in two adult patients presenting with diffuse palmar erythema without any underlying cause by Lane in 1929.3 We found only 17 patients who have been reported with this condition since then in literature.1,4-12 We think that the paucity of the reports in literature might be attributed to under-recognition, rather than the rarity of the condition. Females were more commonly affected than males, with 11 of 17 patients reported in the literature being female. All patients had positive family history and very early-onset palmar erythema. Recessive or dominant transmissions have been suggested. However, the exact mode of inheritance has not been elucidated yet. The increased recognition of this condition may lead to diagnosis of more patients and help the elucidation of the underlying genetic defect, if any. The clinical characteristics of previously reported patients with erythema palmare hereditarium are given in Table 1.
| Reference | Number of patients | Female/male | Family history (n) | Involvement | Symptoms |
|---|---|---|---|---|---|
| Lane, 1929 | 2 | 0/2 | 2/2 | Bilateral palmar | None |
| Meirowsky, 1933 | 1 | 0/1 | 2 | Bilateral palmar, thenar and hypothenar eminences | None |
| Walsh, 1941 | 2 | 2/0 | 1/1 | Bilateral palmar erythema | None |
| Dorn, 1958 | 1 | 1/0 | 1/1 | Palmar erythema | None |
| Rupec, 2000 | 1 | 1/0 | 4 | Bilateral palmar, thenar and hypothenar eminences | None |
| Sarma and Wang, 2007 | 1 | 0/1 | 2 | Bilateral palmar | None |
| Kluger, 2010 | 1 | 1/0 | 1 | Bilateral palmar monticule, thenar and hypothenar eminences, phalanges | None |
| Langanauer, 2014 | 1 | 1/0 | 0 | Bilateral palmar, hypothenar eminences | None |
| Duriex, 2016 | 1 | 1/0 | 2 | Bilateral palmar, thenar and hypothenar eminences, the palmar aspect of fingers | None |
| Gurioli, 2017 | 5 | 3/2 | 1/1/0/1/1 | Bilateral palmar, thenar and hypothenar eminences | None |
| de lorenzi, 2019 | 1 | 1/0 | 2 | Bilateral palmar erythema with telangiectasia to the thenar and hypothenar eminences | None |
| Present report | 4 | 2/2 | 1/1/1/1 | Bilateral palmar erythema | None |
n: Number of patients
The diagnosis of erythema palmare hereditarium requires a positive family history, onset shortly after birth or during childhood and exclusion of any systemic disease through a careful history and physical examination.1,11
The dermoscopic features of erythema palmare hereditarium have been previously defined in only one study.11 A dermoscopic pattern consisting of arborizing vessels on a red, structureless background, similar to observation in our patients, was reported to be suggestive of erythema palmare hereditarium. Future studies might help to understand if the use of dermoscopy in the diagnosis of erythema palmare hereditarium is of benefit.
In conclusion, erythema palmare hereditarium is an innocuous, familial form of palmar erythema and should be kept in mind in patients with early-onset palmar erythema without any underlying cause. Considering the comprehensive list of differential diagnosis of secondary palmar erythema, increased recognition of this entity among physicians seems important to prevent patients from undergoing excessive laboratory testing which might cause anxiety in patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Erythema palmare hereditarium (Lane's red palms): A forgotten entity? J Am Acad Dermatol. 2010;63:e46.
- [CrossRef] [PubMed] [Google Scholar]
- Über das Krankheitsbild des Erythema palmo-plantare symmetricum hereditarium. Arch Dermatol Syph. 1933;168:420-8.
- [CrossRef] [Google Scholar]
- Erythema palmare and naevus-araneus-like telangiectases. Arch Dermatol. 1941;44:616.
- [CrossRef] [Google Scholar]
- Unregelmäßig dominanter Erbgang bei Erythema palmare et plantare (Lane) Z Haut Geschl Kr. 1958;25:141-5.
- [Google Scholar]
- Erythema palmare hereditarium ("red palms") Hautarzt. 2000;51:264-5.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema Palmare hereditarium (red palms): Lane's disease. Dermatol Online J. 2007;13:28.
- [Google Scholar]
- Erythema palmare hereditarium ('Red Palms', 'Lane's Disease') Case Rep Dermatol. 2014;6:245-7.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema palmare hereditarium (Lane's disease): Report of a paediatric case. Ann Dermatol Venereol. 2016;143:32-5.
- [CrossRef] [PubMed] [Google Scholar]
- Lane's disease (Erythema Palmare Hereditarium): A report of five cases and a review of the literature. Pediatr Dermatol. 2017;34:590-4.
- [CrossRef] [PubMed] [Google Scholar]





