Translate this page into:
A comparative evaluation of skin and nerve histopathology in single skin lesion leprosy
2 Department of Dermatology and STD, Bangalore Medical College, Bangalore, India
Correspondence Address:
Raghunatha R Reddy
MathaPitha Polyclinic, # 8, GK Plaza, Banasawadi Main Road, Jai BharathNagar, MS Nagar post, Bangalore, Karnataka-560033
India
| How to cite this article: Reddy RR, Singh G, Sacchidanand S, Okade R, V S, A U, Haneef NS. A comparative evaluation of skin and nerve histopathology in single skin lesion leprosy. Indian J Dermatol Venereol Leprol 2005;71:401-405 |
Abstract
Background: In spite of leprosy being a disease of nerves, ROM therapy for single skin lesion leprosy was based on clinical trials without much evidence-based studies of nerve pathology. The present study was undertaken to compare the histology of skin and nerve in single skin lesion leprosy, and to assess the scientific rationale and justification of single dose ROM therapy. Methods: Twenty-seven untreated patients with single skin lesion without significantly thickened peripheral nerves were selected. Skin and nearby pure cutaneous nerve biopsies were studied under both H&E and Fite's stain. Results: All the skin biopsies were negative for AFB and clinico-pathological correlation was positive in 51.85% of skin biopsy specimens. Histopathological diagnosis of leprosy was evident in 55.5% of clinically normal looking nerves, with AFB positivity in 29.6% of nerve biopsy specimens. Correlation between clinical diagnosis and nerve histopathology was poor (26%). Conclusions: Single skin lesion without thickened peripheral nerves as criteria for single dose ROM therapy is not logical, since the histological diagnosis of leprosy in normal looking nerves with presence of AFB is revealed in this study. Pure cutaneous nerve biopsy is a simple outpatient procedure, without complications. This study emphasizes the need to consider nerve pathology as an important tool for further therapeutic recommendations, than just clinical trials and skin pathology alone. Though single dose ROM therapy has been withdrawn recently, the principle holds good for any future therapeutic recommendations.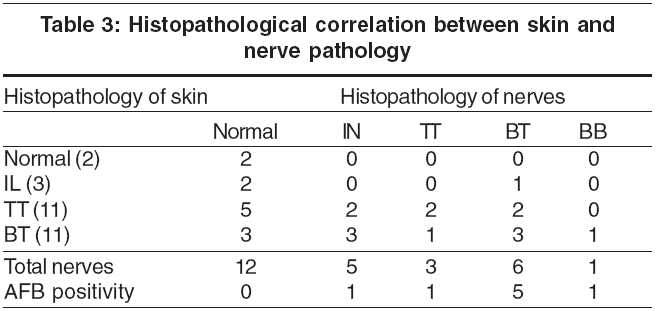
 |
 |
 |
 |
 |
 |
Introduction
In 1997, based on WHO recommendations, India and other countries implemented ROM therapy, rifampicin 600 mg, ofloxacin 400 mg and minocycline 100 mg as a single dose, for patients with single skin lesion leprosy without clinically thickened peripheral nerves.[1] Some clinical trials of single dose ROM therapy for all PB cases have subsequently been conducted with encouraging results, but all are with soft targets like resolution or disappearance of skin lesions.[2] There are few studies based on pathological evidence of the disease and with a follow up period being sufficient to determine the rate of reactions, relapses and recurrences.
Leprosy can be therapeutically better served if the following golden rules are considered:1. There is no non-neural leprosy.
2. It is better to over-treat leprosy than to under-treat it.
3. The clinical types of the disease and its pathology depend on the cell-mediated immunity, which is different in the skin and nerve in the same patient.
4. A nerve may be pathologically affected, but clinically appreciable significant nerve thickening may be delayed.
This study was started based on these facts and aimed 1. To compare the histopathology of skin and nerve in patients with single skin lesion Hansen′s disease.
2. To assess the scientific rationale and justification of single dose ROM therapy.
Methods
Twenty-seven untreated leprosy patients having a single skin lesion located near the radial cutaneous, sural or great auricular nerves, without significantly thickened peripheral nerves, were selected randomly from the Departments of Dermatology and STD of Victoria Hospital, Bangalore, SNR District Hospital and RL Jalappa Hospital and Research Centre, Kolar, during the period November 1998 to January 2003. Biopsies from skin lesions over the lower half of the forearm, lower leg, neck and inferolateral aspect of the face and from nearby pure cutaneous nerves were studied under both H and E and Fite′s stains.
Nerve biopsy procedure After obtaining informed consent and after pre-surgical preparation, partial or full thickness biopsies of the sural, radial cutaneous or great auricular nerves were taken from near the skin lesions. The sural nerve was biopsied approximately 5-7 cm proximal to the lateral malleolus, between the Achilles tendon and the lateral border of fibula, through a superficial, vertical and elliptical incision. The radial cutaneous nerve was biopsied at about 3-5 cm proximal to the radial styloid process, over the lateral border of the radius, with a vertical or transverse superficial incision, keeping in mind the position of the radial artery at the wrist. For the great auricular nerve, an oblique incision was made over the areas of the nerve crossing the sternocleidomastoid muscle at the upper and lateral aspect of the neck.
After these incisions, blunt dissection was done carefully, upto the level of the subcutis. The nerve was identified and freed for a length of about 3 cm. An artery forceps was introduced beneath the nerve trunk and its blades were separated. Both the ends of the nerve were tied. The nerve trunk was split along the length and a partial or full thickness of 2.5-3 cm length of the nerve was biopsied. The wound was sutured in layers. The specimen was preserved in 10% formaldehyde solution and sent for histopathological examination.
Results
Twenty-seven patients, 19 males and 8 females, were included in this study. The youngest patient was 7 years old and the oldest was aged 68 years; the maximum number of patients was in the age group of 25-35 years. Four patients had skin lesions over the face and neck, 9 over the lower limbs and 14 over the upper limbs. The duration of the lesions varied from 1 month to 14 months. Sensations over the skin lesions were intact in 11, decreased in 7 and absent in 9 patients. A clinical diagnosis of tuberculoid leprosy (TT) was made in 15 patients, borderline tuberculoid (BT) leprosy in 6 patients, and indeterminate (IL) leprosy in 6 patients.
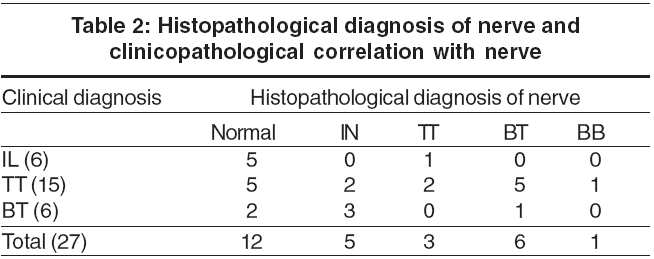
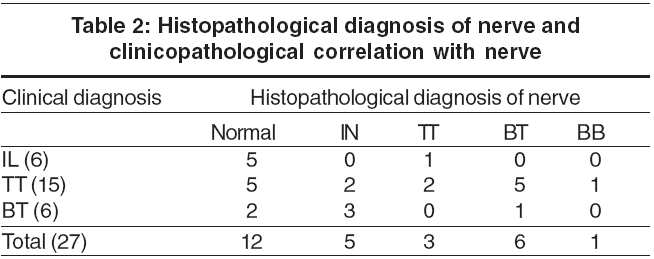
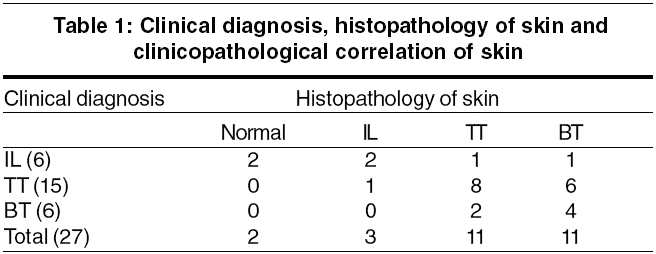
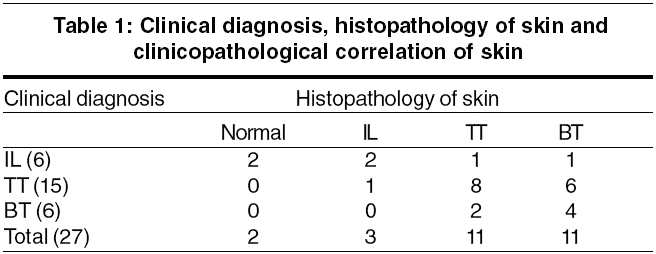
Histopathology of the skin with clinico-pathological correlation [Table - 1] : Clinico-pathological correlation with the skin biopsy findings was seen in 14 out of 27 cases (51.85%). All the skin biopsies were negative for AFB.
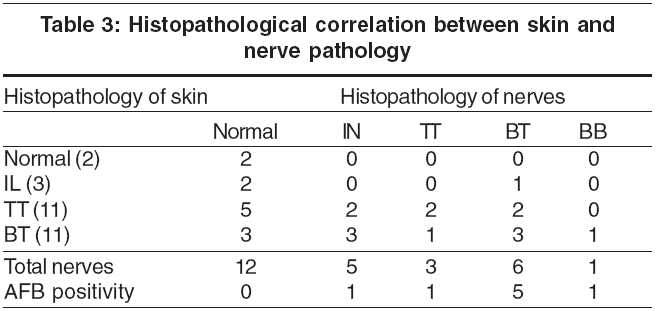
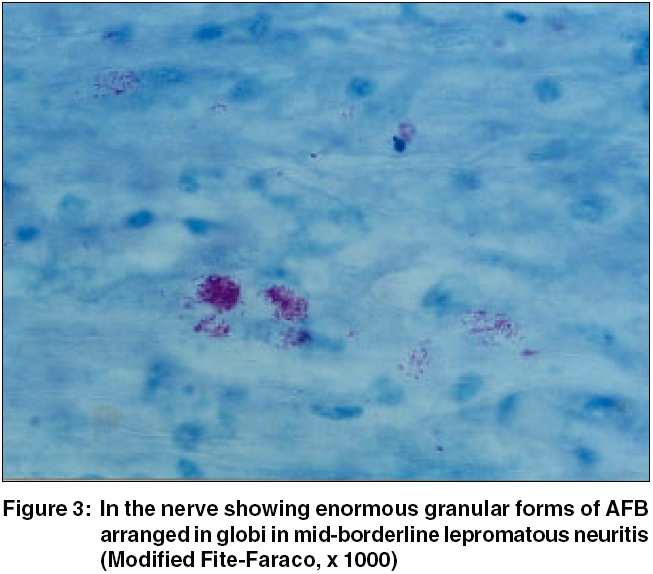
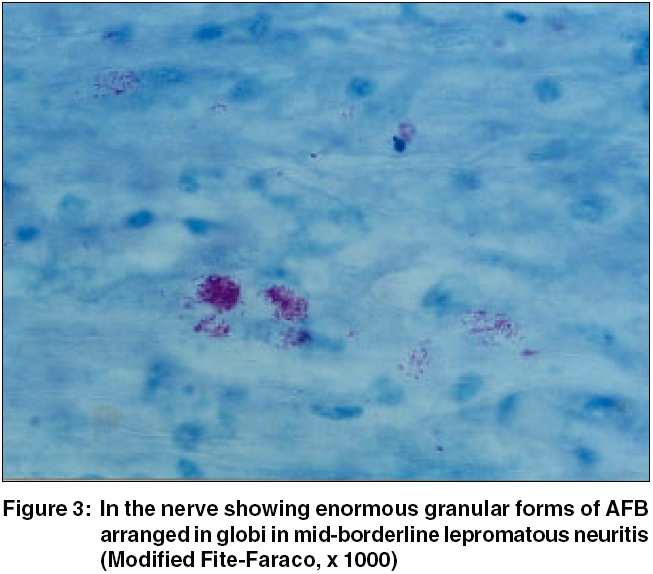
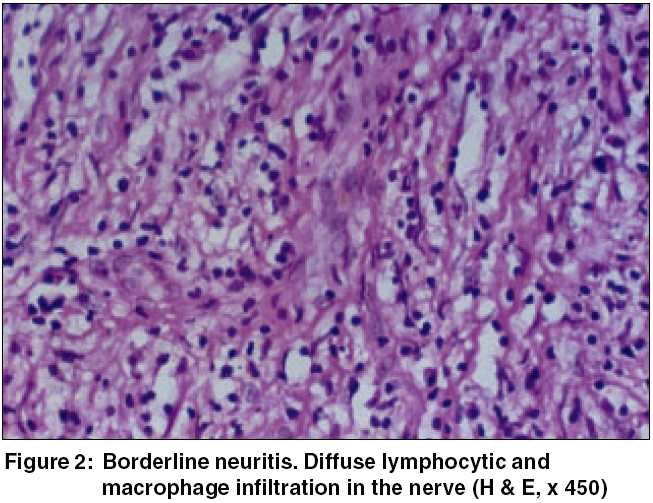
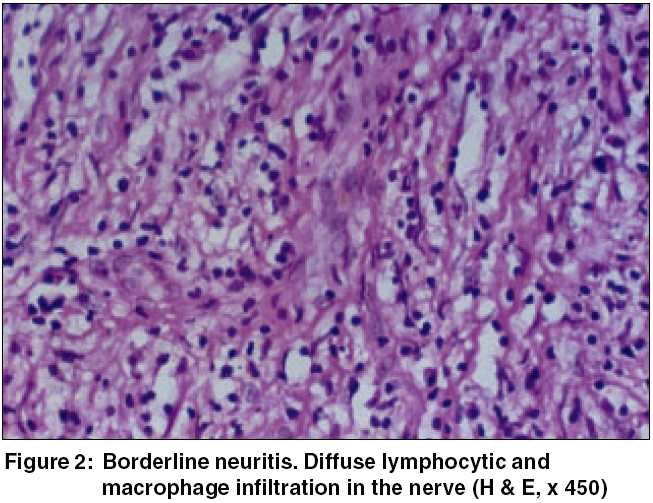
Histopathology of the nerve with clinico-pathological correlation of nerve [Table - 2]: The histopathological diagnosis of Hansen′s disease was evident in 55.5% (15/27) of nerve biopsy specimens, where the nerves were clinically not significantly thickened [Figure - 1][Figure - 2] [Figure - 3].
Histopathological correlation between skin and nerve [Table - 3]: Histopathological correlation between the skin and nerve findings was seen only in 26% (7/27) of cases. AFB were demonstrated in 29.6% (8/27) of nerve biopsies with formation of globi in 3 cases. An inflammatory infiltrate diagnostic of leprosy was seen in 55.5% cases in nerve biopsies.
Discussion
The incidence of leprosy, especially infective cases, has reduced drastically after the introduction of MDT, and yet leprosy continues to be a major public health problem. Active case detection programs show an increase in the number of single lesion cases.[3]
Leprosy is primarily a disease of nerves even though most of the criteria for diagnosis are related to the skin.[4] Pathologically, more than 30% of the nerve should be involved for functional impairment to be appreciated clinically. The entire spectrum of leprosy has been observed in nerves. Lepromatous morphology is not uncommon even in patients with thickening of a single nerve. Recent histological studies have shown deep dermal nerve involvement even in indeterminate leprosy patients. Distant uninvolved nerves may also show evidence of the disease. [5]
While the skin histology continues to be the standard tool in confirming the diagnosis and classification of leprosy, the nerve histology gives more information about the exact classification.[4],[6] Several authors have observed differences in the bacillary load and in the histopathology between the skin and nerve lesions, particularly in PB cases.[7]
In early lesions there appears to be a dichotomy in immunological grading between the skin and nerve and this needs to be explored in greater detail. The majority of reports show discordance between skin and nerve histology, showing immunologically lower spectrum of disease in nerves. Mukherjee and Misra, in a study of comparative histopathology of skin and nerve granulomas in leprosy patients showed high granuloma fraction, caseation and increased extent and severity of the disease in nerves.[8] In one report, viable bacilli were detected (by injecting suspensions into the mouse footpad) in 33% of nerve biopsies and in 19% of skin biopsies of patients after 2 years of treatment with MB-MDT.[9] A similar study from Hyderabad concluded that further studies are needed to determine the relevance of skin and nerve histology and the presence or absence of AFB in the nerves to determine the correct duration of therapy.[10] Several other studies have also shown differences in the histopathological findings of skin and nerve biopsies.[11] The nerves were found to be bacillated even after the skin lesions had cleared or regressed.[11] A nerve biopsy is more informative and specific than a skin biopsy in the diagnosis and classification of patients when the skin histology is indeterminate.[4],[6]
ROM has been accepted and implemented the world over. It is claimed to be successful in patients with single skin lesion leprosy without thickened peripheral nerves. Since the assessment and cure criteria are slightly controversial, it is difficult to decide the endpoint of treatment in neuritic leprosy. Several patients show advanced disease and are AFB positive in both the skin and the nerve even when only one or a few nerves are clinically affected. This suggests that such patients are better included in the MB group, whereas the WHO recommends PB-MDT for such patients.[12]
ROM therapy has been found to be operationally attractive, feasible and acceptable to the community, but several leprologists have reservations with specific reasons against the concept of single dose ROM therapy.[13] A double blind, placebo-controlled multicenter trial in India with ROM and PB-MDT for single skin lesion leprosy found clinical improvement to the same extent in both groups.[14] The ROM group showed 46.9% complete cure compared to 54.7% in the PB-MDT group. In this study, the measures of outcome were soft, like clinical improvement and complete clearance of lesions. Encouraged by these results, the NLEP adopted single dose ROM therapy for PB patients with 2-3 skin lesions. The results were almost similar in the patients who had lesions in the same anatomical region, but PB-MDT gave better results in patients who had lesions in different anatomical sites. This clearly suggests that apart from the number of skin lesions there are several other factors to be considered. In this study, the sample size was small, the duration of observation was only 18 months, and, most importantly, there was no information on the relapse rate.[14]
Another study conducted by the same group in a large number of PB patients with 1-5 skin lesions, with treatment for 6 months and follow up for 4 years, is expected to generate more information on cure and relapse rates.[2]
Disappearance of the granuloma was seen in 70% in ROM + Convit vaccine group, but in only 53.3% with ROM alone, which is statistically significant.[15] Recently, a WHO technical advisory group reviewed the preliminary findings of ROM trials for single skin lesion PB cases, and PB cases up to 5 skin lesions. They recommended an additional year of follow up together with full analysis of findings for the programme.[16]
Leprosy is essentially neural in inception and exhibits lower immunological grading and higher bacterial load in nerves as compared to skin, as evident in the present study. Even though a nerve biopsy is not feasible and practical in the field and in mass control programs, the utility of neural histology in selecting and monitoring therapeutic regimens to prevent drug resistance and relapse can not be overemphasized, since neural histology gives better information about classification as it is evidenced by the findings in this study.
| 1. |
WHO expert committee on leprosy: Seventh report: WHO technical report series No.874. Geneva: WHO; 1998.
[Google Scholar]
|
| 2. |
2-3 lesions multicentre trial group: A comparative trial of single dose ROM therapy for PB patients. Indian J Lepr 2001;33:131-44.
[Google Scholar]
|
| 3. |
Dharmendra, Ramu G. Type of disease in relation to prognosis in leprosy. In: Dharmendra, editor. Leprosy. Mumbai: Kothari Medical Publishing House; 1978. p. 687-98.
[Google Scholar]
|
| 4. |
Ashok Kumar SK, Reddy BS, Ratnakar C. Correlation of skin and nerve histopathology in leprosy. Lepr Rev 1996;67:119-25.
[Google Scholar]
|
| 5. |
Neuritic leprosy. ICMR Bulletin 1996;26.
[Google Scholar]
|
| 6. |
Kaur S, Sharma VK, Basak P, Kaur I, Radotra BK. Current skin and nerve histology in leprosy and its role in classification of leprosy. Lepr Rev 1993;64:110-6.
[Google Scholar]
|
| 7. |
Jorg M, Ponnighaus, Leanhardt C, Lucas S, Fine PE, Sterne JA. Comparison of bacillary indices in slit skin smears, skin and nerve biopsy: a study from Malawi. Int J Lepr 1997;65:211-6.
[Google Scholar]
|
| 8. |
Mukerjee A, Misra RS. Comparative histology of skin and nerve granulomas in leprosy patients. Lepr Rev 1988;59:177-80.
[Google Scholar]
|
| 9. |
Shetty VP, Suchitra K, Uplekar MW, Antia NH. Higher incidence of viable Mycobacterium leprae within the nerve as compared to skin among MB leprosy patients released from multidrug therapy. Lepr Rev 1997;68:131-8.
[Google Scholar]
|
| 10. |
Lakshmi TS, Rao PN, Venkata KA, Solomon VK. Histopathology of skin and nerve and clinical classification in leprosy patients. Ind J Lepr 1996;68:258-60.
[Google Scholar]
|
| 11. |
Uplekar MW, Antia NH. Clinical and histological observations in pure neuritic leprosy. Ind J Lepr 1986;58:513-21.
[Google Scholar]
|
| 12. |
Girdhar BK. Neuritic leprosy. Ind J Lepr 1996;68:35-42.
[Google Scholar]
|
| 13. |
Revankar CR, Pai VV, Bulchand HO, Ganapathi R. Relapse rate in single dose treatment in PB leprosy. Asian Leprosy Congress, Agra, India. 9th-13th Nov 2000 (Abstract No.123).
[Google Scholar]
|
| 14. |
Single lesion multicentre trial group. Efficacy of single dose MDT for the treatment of single lesion PB leprosy. Ind J Lepr 1997;69:121-9.
[Google Scholar]
|
| 15. |
Suneetha S, Arunthathi S, Chandi S, Kurian N, Chacko CJ. Histological studies in primary neuritic leprosy: changes in the apparently normal skin. Lepr Rev 1998;69:351-7.
[Google Scholar]
|
| 16. |
Report on the 6th meeting of the WHO technical advisory group on the elimination of leprosy. Geneva 9th-10th February 2004.
[Google Scholar]
|
Fulltext Views
2,715
PDF downloads
1,483





