Translate this page into:
A cross-sectional analysis of inflammatory markers as a severity and prognostic indicator in severe cutaneous adverse drug reactions
Corresponding author: Dr. Varadraj V Pai, Department of Dermatology, Goa Medical College, Bambolim, Panaji, India. docpai@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: GS Nayana Thara, Pai VV, Kadkol A, Fernandes E, Shulka P. A cross-sectional analysis of inflammatory markers as a severity and prognostic indicator in severe cutaneous adverse drug reactions. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1284_2024
Abstract
Background
The inflammatory markers (IMs) are a set of biomarkers used clinically to assess a patient for the presence of an active inflammatory disease or disease activity. They are elevated in conditions like infections, malignancies, mental illness and drug reactions among others.
Aim
The study aimed at identifying the IMs that reflect the severity and recovery in severe cutaneous adverse drug reactions (SCARs).
Methods
A cross-sectional observational study was conducted among patients with SCARs (Stevens Johnson syndrome [SJS]/ toxic epidermal necrolysis [TEN] and drug reaction with eosinophilia and systemic symptoms [DRESS]) admitted to a tertiary care hospital over 18 months.
Results
Twenty SJS/TEN and 8 DRESS cases were included in the study. There were more females in the study (F: M = 2:1). Comparing the IMs of SJS/TEN and DRESS revealed that most markers on day 7 were lower as compared to day 0. There was a significant difference in eosinophil count (EC), procalcitonin (PCT) (p-value <0.05), and recovery time between the two groups. In the SJS/TEN group, markers like ferritin (>2000 ng/mL) and PCT (>2.0 ng/mL) were significantly higher, around the septic range, in patients with concurrent connective tissue disease and culture positivity. Ferritin (p-value- 0.025, rho- 0.578), PCT (p-value- 0.013, rho- 0.239), and ESR (p-value- 0.041, rho- 0.482) were associated with the severity of SJS/TEN. Patients with DRESS had an early recovery with a statistically significantly shorter hospital stay than SJS/TEN (p<0.005). Baseline severity-of-illness score for TEN levels, total counts, and day 7 PCT significantly reflected the time taken for recovery.
Limitations
Marker analysis was performed at baseline and on day 7 of admission, but not after complete clinical recovery, therefore indicating a trend but limited conclusive behaviour of markers at the time of recovery.
Conclusion
The progression of IMs in a SCAR follows the clinical course of the illness. IMs like ferritin and PCT, along with routine haematological investigation, aid in identifying the severity, differentiating it among patients with comorbidities, and helping predict the recovery time in SCARs.
Keywords
Inflammatory markers
ferritin
procalcitonin
severity-of-illness score for toxic epidermal necrolysis (SCORTEN)
severe adverse cutaneous drug reaction.
Introduction
Severe cutaneous adverse drugs reactions (SCAR) are a group of disorders, including Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), drug hypersensitivity reactions or drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalised exanthematous pustulosis, which are associated with significant morbidity and mortality.1 One of the important therapeutic measures in SCAR other than precise identification and stoppage of the causative drug, involves determining the necessity and type of immunosuppressive therapy. This requires careful evaluation of clinical, haematological, and biochemical parameters. The inflammatory markers (IM) are a set of biomarkers that are used clinically to assess a patient for the presence of an active inflammatory disease or disease activity. These markers are raised in a broad spectrum of diseases like infections, mental illness, malignancies, and drug reactions among others suggesting the role of inflammation in their pathogenesis as well.2 Inflammatory responses in a SCAR can be confounded by secondary infections or the patients’ underlying disease, which can cause difficulty in the interpretation of these IMs. It is important for the dermatologist to identify which IMs reflect the severity and recovery in SCARs.
Methods
An observational cross-sectional study, after obtaining due approval from the institutional ethical board, was conducted among patients admitted with SCARs in a tertiary care hospital over a period of 18 months. The SCARs included were Stevens-johnson syndrome/ Toxic epidermal necrolysis (SJS/TEN) and DRESS. These were diagnosed, and the severity was assessed based on the clinical findings and standard definitions or criteria that have been laid down, e.g., severity of illness score for toxic epidermal necrolysis (SCORTEN) and RegiSCAR group diagnosis score.2 The SJS/TEN study group was divided into three categories including (i) SJS/TEN without comorbidities the connective tissue disorder were kept as a seperate group because, (1) they are associated with increase in IM on their own, (2) there is an increase chance of drug reaction in this group the other comorbidities included were hypertension, Diabetes mellitus (DM), ishaemic heart disease, (ii) SJS/TEN with comorbidities, and (iii) SJS/TEN with connective tissue disorders (CTDs). The culture positivity which were considered were skin culture and blood culture as these can also affect the IM. They were compared across all patients in the sample. Routine baseline investigations were done in all patients and repeated at week 1. Relevant investigations were performed to rule out any focus of infection. The IMs such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), serum ferritin, serum D- Dimer, serum lactate dehydrogenase (LDH), serum procalcitonin (PCT), total counts (TC), neutrophil-lymphocyte ratio (NLR), and eosinophil count (EC) were analysed on the day of admission (D0) and after 1 week (D7). Systemic treatment for both SJS/TEN and DRESS was given as per standard protocol. The results were tabulated in an Excel sheet and statistical analysis was performed using Jamovi 2.3.28. For data analysis, the study used Shapiro- Wilk as a normality test. A paired T-test was used to interpret Intragroup D0 and D7 changes. Independent sample T-test (Student’s T-test or Mann-Whitney U test based on the distribution) was used to compare two unrelated groups. One-way analysis of variance was used to understand three or more unrelated groups. Spearman correlation test was conducted to discover the association of various markers with SJS/TEN severity degree, measured using SCORTEN. The area under the receiver operating characteristic (ROC) curve was obtained to understand which of the IMs could predict recovery better.
Results
A total of 28 patients admitted with SCAR were included in the study with 20 SJS/TEN cases and 8 DRESS cases. Females outnumbered males in our study (F: M = 2:1). There was a female preponderance in SJS/TEN and a male preponderance in DRESS. The age group ranged from 13 to 77 years. The characteristics of study groups have been given in Table 1. Antibiotics (35%) and Non steroidal Antiinflammatory drugs (25%) were the most common drugs implicated in the SJS/TEN group, whereas antiepileptics were the most commonly attributed drugs in DRESS, followed by antibiotics and anti-tubercular drugs.
| Cutaneous adverse drug reactions | Male | Female | SCORTEN <3 | SCORTEN ≥3 | Drugs |
|---|---|---|---|---|---|
| SJS/TEN overall | 4 | 16 | 11 | 9 | Antibiotic 10 |
| NSAIDS 5 | |||||
| Antiepileptic 2 | |||||
| Allopurinol -3 | |||||
| SJS/TEN without comorbidities | 2 | 7 | 6 | 3 | Antibiotic 3 |
| NSAIDS 3 | |||||
| Allopurinol -3 | |||||
| SJS/TEN with comorbidities | 2 | 5 | 3 | 3 | Antibiotic 5 |
| Allopurinol -1 | |||||
| SJS/TEN with CTDs | 0 | 4 | 1 | 3 | NSAIDS 3 |
| Antibiotics -1 | |||||
| DRESS | 5 | 3 | Antiepileptic -3 | ||
| Antibiotic – 2 | |||||
| Anti-tubercular – 2 | |||||
| Allopurinol -1 |
NSAIDS: Non steroidal antiinflammatory drug
The comparison of IMs of SJS/TEN and DRESS has been given in Table 2. Most D7 values were less than D0 in both groups. However, there was no significant intragroup variation between D0 and D7. Intergroup significant differences were noted between patients of SJS/TEN and DRESS in the eosinophil count (EC) (p-value -0.009/0.007) and PCT (p-value 0.015/0.028) values at both D0 and D7. Also, the differences between D0 neutrophil-lymphocyte ratio (NLR), D7 ferritin, and TC were significant. The recovery time was also found to be significant with DRESS patients recovering before SJS/TEN. Qualitative CRP was assessed. It was positive in 95% and 90% of cases of SJS/TEN on D0 and D7, respectively. In DRESS patients, it was positive in 87.5% and 50% on D0 and D7, respectively
| SCARs | Ferritin | LDH | D-Dimer | ESR | ESR | TC | NLR | EC | SCORTEN | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| D0 | D7 | D0 | D7 | D0 | D7 | D0 | D7 | D0 | D7 | D0 | D7 | D0 | D7 | D0 | D7 | D0 | D7 | |
| SJS/TEN | 774 | 877 | 414 | 357 | 1063 | 938 | 1.8 | 1.17 | 44.3 | 42.5 | 9852 | 8365 | 5.42 | 9.13 | 4.59 | 3.81 | 2.55 | 1.50 |
| DRESS | 295 | 305 | 403 | 330 | 1104 | 1113 | 0.23 | 0.055 | 37.7 | 31.7 | 14216 | 11681 | 2.68 | 2.33 | 13.7 | 8.09 | ||
| P –value | 0.055 | 0.047 | 0.887 | 0.387 | 0.739 | 0.404 | 0.015 | 0.028 | 0.249 | 0.095 | 0.055 | 0.034 | 0.05 | 0.198 | 0.009 | 0.007 | ||
| SJS/TEN with CM | 489 | 451 | 415 | 355 | 923 | 804 | 4.42 | 1.2 | 40 | 32 | 10010 | 9254 | 6.65 | 19.0 | 4.78 | 2.83 | 2.67 | 1.00 |
| SJS/TEN others | 376 | 458 | 390 | 333 | 690 | 801 | 0.65 | 0.413 | 44 | 44 | 9367 | 7960 | 4.89 | 5.82 | 4.13 | 3.89 | 2.22 | 1.45 |
| SJS/TEN With CTD | 2259 | 2664 | 449 | 463 | 1342 | 1543 | 1.08 | 3.2 | 47.5 | 54 | 10988 | 9058 | 5.65 | 3.56 | 5.25 | 5.75 | 3.25 | 2.50 |
| P –value | 0.050 | 0.042 | 0.762 | 0.380 | 0.456 | 0.666 | 0.080 | 0.029 | 0.776 | 0.071 | 0.936 | 0.295 | 0.675 | 0.540 | 0.996 | 0.717 | 0.213 | 0.311 |
| SJS/TEN culture positive | 1231 | 1462 | 413 | 431 | 939 | 1084 | 1.10 | 2.18 | 46.9 | 49.3 | 10371 | 8756 | 5.09 | 16.5 | 3.65 | 3.13 | 3.22 | 2.33 |
| SJS/TEN culture negative | 400 | 399 | 414 | 296 | 1188 | 972 | 2.45 | 0.339 | 42.2 | 37.0 | 9386 | 8047 | 5.70 | 3.08 | 5.36 | 4.36 | 2.00 | 0.818 |
| P –value | 0.102 | 0.030 | 0.879 | 0.128 | 0.627 | 0.791 | 0.970 | 0.025 | 0.403 | 0.073 | 0.713 | 0.425 | 0.704 | 0.063 | 0.182 | 0.098 | 0.004 | 0.017 |
SJS/TEN was further divided into three subtypes- (i) SJS/TEN with co-morbidities (CM), (ii) SJS/TEN with connective tissue disorders (CTDs), and (iii) SJS/TEN-others. Among 20 SJS/TEN cases, 9 had no comorbidities and 11 had comorbidities like CTDs (36%), diabetes (17%), hypertension (25%), ischaemic heart disease, HIV (18%), tuberculosis (16%), etc. Among CTD, three patients had systemic lupus erythematosus and one was a case of Mixed connective tissue disorder. The markers were compared among the three groups [Table 2]. Most IMs were higher in patients with CTD as compared to others. The intragroup IMs of D7 were lower than D0 except in patients with CTD, where most D7 values were higher. Among the intergroup variations, ferritin of D0 and D7 and PCT on D7 show significant differences among the three groups [Table 2].
The IMs among culture-positive and negative SJS/TEN have been compared in Table 2. In culture-positive SJS/TEN, most markers were higher on D7 as compared to D0, while in culture-negative all markers were lower on D7 as compared to D0. No significant intragroup variation was noted. The intergroup variation included significant difference in D7 ferritin and PCT. The SCORTEN score of D0 and D7 was also significant
Comparison of the severity of SJS/TEN with IMs at various intervals (Day 0 and Day 7) has been given in Table 3. The severity of SJS/TEN was assessed with the SCORTEN score (score ≥3 was considered severe [S] and <3 was considered less severe [LS]). Comparison of the IMs and severity of SJS/TEN on D0 revealed that increased ferritin levels were significantly increased in correlation to the severity of the disease (p-value 0.03, rho-0.337) [Table 3]. While comparing the initial severity of SJS/TEN (D0) with IM levels on D7, it was observed that these markers can be raised during treatment in a severe presentation. PCT, erythrocyte sedimentation rate, and serum ferritin levels were significantly raised on D7 as compared to baseline in severe type of SJS/TEN [Table 3]. The D0 IM comparison with D7 severity was studied to identify the markers that can predict the outcome (in terms of severity on day 7) at the time of presentation. None of the markers had significance but the D0 Ferritin had the lowest p- values with positive correlation (p-value- 0.066, rho-value- 0.441). By correlating D7 IM levels with disease severity on D7, we aimed to identify markers that correspond to the patient outcome. None of the markers had significance. The overall changes in the IM have been given in Figure 1.
| D0/D7 Severity vs. IM |
Severity of SJS/TEN Less severe (LS) - SCORTEN < 3 Severe (S) - SCORTEN ≥ 3 |
TC |
NLR | EC | ESR | Ferritin | LDH | PCT | D-dimer |
|---|---|---|---|---|---|---|---|---|---|
|
D0 SCORTEN Vs D0 IM |
LS | 11289 | 5.57 | 4.35 | 43.5 | 356 | 412 | 2.02 | 1047 |
| S | 8256 | 5.25 | 4.89 | 43.2 | 1285 | 416 | 1.63 | 1080 | |
| P value | 0.189 | 0.834 | 0.756 | 0.749 | 0.030 | 0.958 | 0.552 | 0.730 | |
| Spearman rho (ρ) | -0.563 | -0.036 | 0.084 | 0.084 | 0.337 | -0.153 | -0.208 | 0.049 | |
|
D0 SCORTEN Vs D7 IM |
LS | 8427 | 4.91 | 3.91 | 36.7 | 428 | 302 | 0.315 | 636 |
| S | 8238 | 14.3 | 3.69 | 49.7 | 1426 | 424 | 2.21 | 1241 | |
| P value | 0.871 | 0.882 | 0.894 | 0.041 | 0.025 | 0.158 | 0.013 | 0.077 | |
| Spearman rho (ρ) | 0.051 | 0.206 | -0.263 | 0.482 | 0.578 | 0.297 | 0.239 | 0.421 | |
|
D0 IM Vs D7 SCORTEN |
LS | 10205 | 5.88 | 4.26 | 44.3 | 544 | 417 | 1.65 | 1014 |
| S | 8866 | 4.06 | 5.60 | 44.2 | 1465 | 405 | 2.42 | 1192 | |
| P value | 0.617 | 0.295 | 0.499 | 0.982 | 0.066 | 0.877 | 0.933 | 0.849 | |
| Spearman rho (ρ) | -0.345 | -0.081 | 0.178 | -0.261 | 0.441 | -0.233 | 0.141 | 0.006 | |
|
D7 SCORTEN Vs D7 IM |
LS | 8409 | 10.6 | 3.21 | 40.7 | 730 | 361 | 1.35 | 773 |
| S | 8235 | 4.75 | 5.60 | 482 | 1319 | 344 | 0.628 | 1367 | |
| P value | 0.916 | 0.735 | 0.195 | 0.322 | 0.230 | 0.862 | 0.898 | 0.402 | |
| Spearman rho (ρ) | 0.134 | 0.090 | -0.024 | 0.253 | 0.434 | 0.213 | -0.002 | 0.180 |
Bold values represents significant values as they are less than 0.05, ESR: Erythrocyte sedimentation rate, LDH: Lactate Dehydrogenase
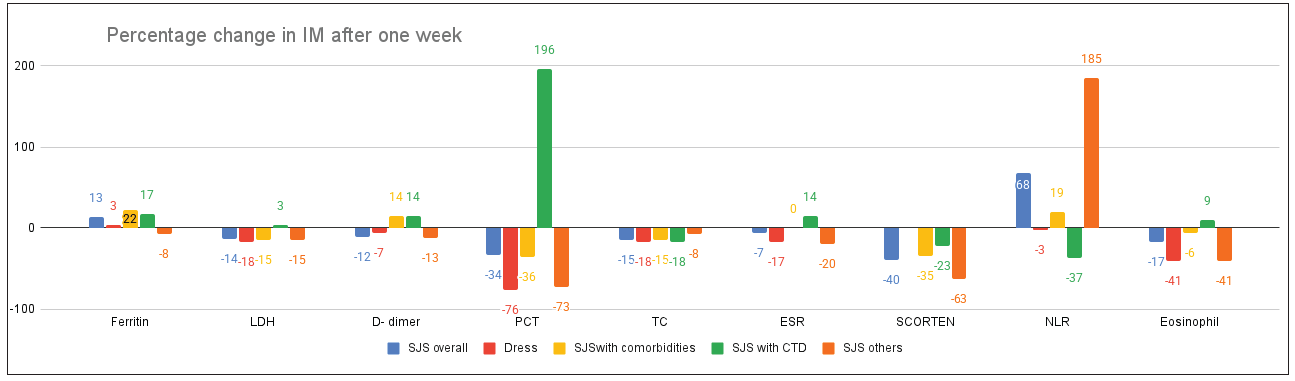
- Percentage change in IM after one week. The graph represents percentage change in IM (that is whether the IM have increased or decreased) after one week. The increase has been represented by columns above the ‘0’ line and decrease has been represented by columns below ‘0’ line. The X-axis represents the various IM which were analyzed during the drug reaction. Y-axis represents the percentage change.
Recovery
The average recovery (admission to discharge) time for all groups has been given in Figure 2. Out of 28 patients, one with MCTD expired. Patients with DRESS had an early recovery with a significantly shorter duration of hospital stay as compared to SJS/TEN (p<0.005). For SJS /TEN, the recovery of the disease was considered ‘Delayed’ if extending beyond 10 days and ‘Early’ if less than 10 days. The recovery time was compared with the D0 and D7 IMs [Table 4].

- Average recovery time. The x- axis represent the different subcategories of drug reactions. The y- axis represent the mean number of day for recovery (discharge). SJS patients required 13 days of hospital admission, DRESS patients required 7 days and so on
| Comparison group | Recovery rate | TC | NLR | EC | ESR | PCT | LDH | D-dimer | Ferritin | SCORTEN |
|---|---|---|---|---|---|---|---|---|---|---|
|
Recovery rate Vs D0 markers |
Early | 7008 | 4.76 | 3.39 | 42.6 | 1.93 | 442 | 1119 | 489 | 2.09 |
| Delayed | 11512 | 5.87 | 5.39 | 45.4 | 1.79 | 395 | 1036 | 964 | 2.92 | |
| P value | 0.052 | 0.476 | 0.250 | 0.599 | 0.473 | 0.505 | 0.616 | 1.000 | 0.029 | |
| Spearman rho | 0.319 | 0.238 | 0.038 | -0.078 | 0.276 | 0.100 | 0.045 | 0.025 | 0.470 | |
|
Recovery rate Vs. D7 markers |
Early | 8146 | 5.15 | 3.88 | 35.8 | 0.217 | 333 | 656 | 488 | 1.13 |
| Delayed | 8513 | 11.8 | 3.77 | 47.1 | 1.80 | 373 | 1076 | 1137 | 1.75 | |
| P value | 0.802 | 0.571 | 0.949 | 0.083 | 0.023 | 0.661 | 0.325 | 0.473 | 0.326 | |
| Spearman rho | 0.187 | 0.333 | -0.181 | 0.364 | 0.460 | 0.201 | 0.265 | 0.250 | 0.154 |
Bold values represents significant values as they are less than 0.05
Comparison of recovery time with D0 markers revealed that the baseline SCORTEN score (p-value 0.029, (ρ)- 0.470) and total count (TC) (p-value 0.05, (ρ)- 0.319) were significant markers of recovery, demonstrating a positive correlation with improved outcome across all groups [Table 4]. The area under the curve (AUC) values of SCORTEN, total count and neutrophil-lymphocyte ratio, in decreasing order, were the best indicators of overall patient recovery at the time of admission [Figure 3]. PCT was the only D7 marker significantly associated with recovery (p-value- 0.023, (ρ)- 0.460). The AUC values of D7 PCT>D-dimer> Ferritin were the best indicators that patients were likely to recover early [Figure 4].
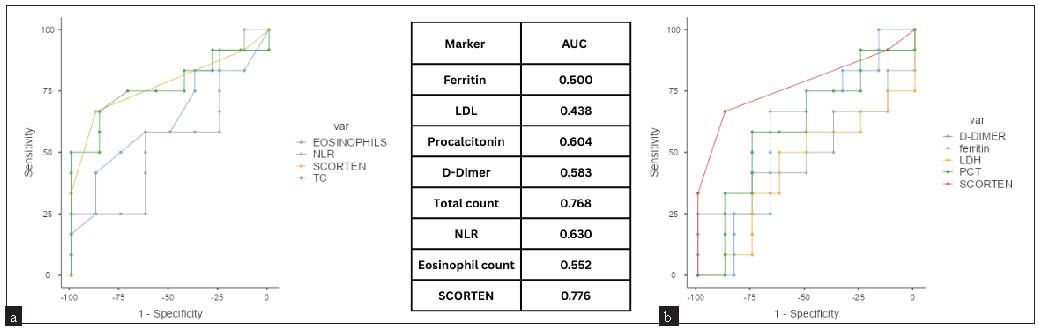
- AUC values of baseline IM with recovery time.(a) ROC curves for eosinophilia, NLR, SCORTEN and Total count, (b) ROC curves for D-Dimer, Ferritin, LDH, PCT and SCORTEN.
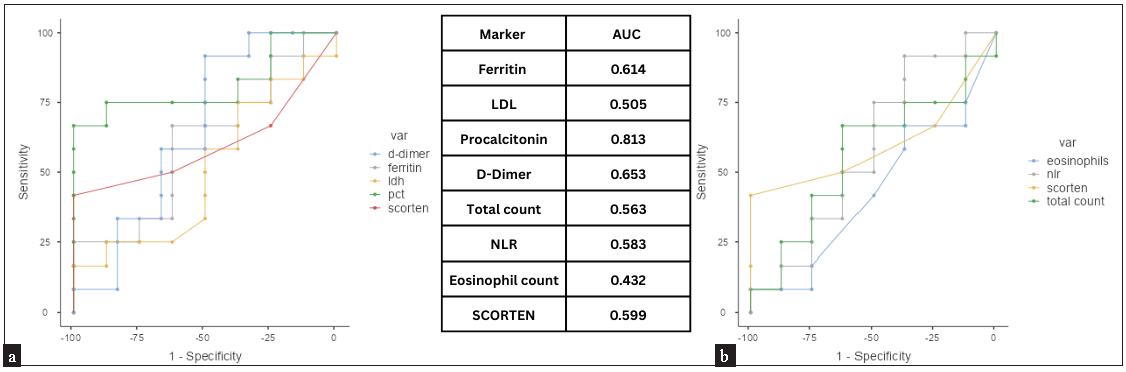
- AUC values of D7 IM with recovery time. (a) ROC curves for D-Dimer, Ferritin, LDH, PCT and SCORTEN, (b) ROC curves for eosinophilia, NLR, SCORTEN and Total count.
Discussion
IMs can potentially serve as biomarkers for disease diagnosis, prognosis, and therapeutic decision-making. Various IMs and their clinical significance have been given in Table 5.3-12 Among the 28 cases of SCAR, the majority of patients were above 40 years, which aligns with findings from other studies. Age is one of the important demographic parameters in the SCORTEN severity assessment for SJS/TEN. The increased incidence of SJS/TEN with age can be attributed to the intake of multiple medications, comorbidities, and decreased renal clearance function among this population.11,13,14
| PCT | PCT is the 116 amino acid precursor of the calcium-regulating peptide, calcitonin. It is increased in bacterial sepsis, drug reactions, anaphylaxis, malignancies, pancreatitis, rhabdomyolysis, cardiac disorders, and trauma. Values upto 0.5 ng/mL are seen in local infections and inflammation, levels between 0.5–2 ng/mL in systemic infections, 2–10 ng/mL in sepsis, and >10 ng/mL in severe sepsis.3,4 |
| Ferritin | Ferritin, a key iron storage protein, is a sensitive biomarker of immune dysfunction. Elevated ferritin levels are seen in cytokine storms and various diseases, including infections, metabolic syndrome, arthritis, septic shock, and alcoholism. Clinically, ferritin levels have proven valuable for both diagnosis and prognosis. In children with septic shock, a ferritin level above 500 ng/mL significantly increased the risk of mortality. Furthermore, ferritin levels exceeding 591.5 ng/mL independently predicted the severity and outcome of sepsis5-7 |
| ESR | The ESR measures the distance red blood cells settle in a vertical tube of anticoagulated blood within one hour. As fibrinogen is responsible for reducing the charge on RBC, ESR is used to indirectly measure fibrinogen activity. In inflammatory conditions, ESR rises between 24-48 hours after the onset of the disease.3 |
| LDH | Serum LDH is commonly increased in patients with haematological malignancies and solid tumours. Elevated LDH correlates with the epidermal injury seen in various skin diseases, including atopic dermatitis and exfoliative dermatitis.8 |
| d-dimer | D-dimers are protein fragments generated by fibrinolysis of a thrombus. D-dimer assays are widely used in the diagnosis of pulmonary embolism and deep vein thrombosis and can predict chances of recurrent thromboembolism. Elevated D-dimer levels are not only seen in vasculitic conditions like eosinophilic granulomatosis with polyangiitis, Henoch-Schönlein purpura and Kawasaki disease but also in non-vasculitic conditions like bullous pemphigoid and chronic urticaria, suggesting D-dimers may serve as a broader marker of inflammation.9 |
| TC | Leukocytosis is defined as an increase in the total number of white blood cells. The specific type of leukocytosis is determined by the predominant WBC subtype contributing to the increase. Infections, inflammatory processes, and adverse drug reactions are among the numerous etiologies of leukocytosis.10 |
| NLR | NLR combines information of two opposite immune paths (innate immune system -neutrophils and adaptive immune system – lymphocytes). Therefore, it is considered a better prognosticator as compared to a single parameter. NLR has been used in several conditions to study disease activity like autoimmune diseases and drug reactions.11 |
| EC | Eosinophils are innate immune cell involved in host defence. Stimulation of pattern recognition receptors leads to degranulation of toxic granule proteins and subsequent immune responses and organ dysfunction predominantly through IL-5. In patients with DRESS, eosinophils can be seen in both, the lesional skin and blood.12 |
PCT: Procalcitonin, ESR: Erythrocyte sedimentation rate, LDH: Lactate dehydrogenase, TC: Total count, NLR: Neutrophil- lymphocyte ratio, EC: Eosionphil count
Females outnumbered males in our study (F: M = 2:1). There was a female preponderance among SJS/TEN and a male preponderance in DRESS. The higher incidence of SJS/TEN among females can be attributed to the occurrence of several conditions like pregnancy, lactation, and autoimmunity in this group.11 However, in DRESS there was a slight male preponderance, which is in contrast with many previous studies.2,15 This may be due to the small sample size of our study.
In our study antibiotics (35%) and Non steroidal anti inflammatory drugs (NSAIDs) (25%) were the most common drugs implicated in the SJS/TEN group, whereas antiepileptics were the most common, followed by antibiotic and anti-tubercular drugs among patients with DRESS. These findings are at par with other studies.15,16
A comparison of IMs in SJS and DRESS revealed a decrease in most D7 values compared to D0 in both groups, indicating an overall improvement in inflammation following treatment. As expected, significant intergroup eosinophilia was noted on both D0 and D7. Eosinophilia is an important criterion for diagnosing DRESS as per the REGISCAR and Japanese consensus group. It is present in 66–95% of patients. In DRESS syndrome, drug antigens can activate specific T-lymphocytes or natural killer cells (NKCs), leading to the production of various cytokines and chemokines.12,17 Patients with DRESS had significantly lower D0 NLR and PCT and D7 ferritin and PCT levels and higher D0 and D7 TC as compared to SJS/TEN. The recovery time was also found to be significantly shorter in DRESS patients than in SJS/TEN patients. We noted a 76% decrease in PCT following treatment. Therefore, serum PCT value can be used as a prognostic marker among DRESS patients [Figure 1]. The usefulness of PCT levels was assessed in a study done by Rhyou HI et al. in differentiating DRESS from bacterial infection among 91 patients, which noted that PCT value in DRESS is associated with severity.18
NLR has been studied as a prognostic parameter to decide whether a patient requires hospital admission. Although the TC in our study was higher in DRESS as compared to SJS/TEN on both days, the NLR of DRESS was lower, indicating predominant non-neutrophilic white blood cell activity in DRESS. The D0 NLR was significantly higher in the SJS/TEN group as compared to DRESS. It showed a non-significant negative correlation with respect to the severity of SJS/TEN. Therefore, NLR was not able to reflect the disease severity nor the recovery rate, unlike other studies.11,19
Categorisation of SJS/TEN subtypes [SJS/TEN with co-morbidities (CM), SJS/TEN with CTDS, and SJS/TEN-others] was done to identify whether any comorbidities can predict the severity of drug reactions. We found that all the IMs, along with the SCORTEN score, were consistently high in patients with CTD. The D0 ferritin, D7 ferritin, and PCT levels were significantly higher among the connective tissue group, with ferritin and PCT reaching the septic range (>2000ng/ml and >2.0ng/ml respectively). A study by Chan et al. showed that individuals with systemic lupus erythematosus (SLE) are 4.69 times more likely to experience drug allergies as compared to controls. This may be due to the dysregulated immune system in connective tissue diseases, which can lead to an increase in hypersensitivity reactions.20 The presence of SCAR in a patient with CTD exacerbates this patho-mechanism as seen in our patients.
Patients with SJS/TEN have an increased risk of infections due to extensive peeling of skin, pre-existing co-morbidities, or use of therapeutic immunosuppressives. Both skin and blood cultures were performed for these patients. Most of the D7 markers in the culture-positive group were higher than D0, indicating an additional inflammatory response to infection. The D7 PCT was in the septic range (>2 ng/mL) in culture-positive SJS/TEN. Similar findings were seen in a study by Yoon et al. where they found serum PCT to be significantly high among patients with bacterial infection. They also reported that the severity of drug eruptions affected the PCT levels.21 PCT levels greater than 0.5 ng/mL are considered consistent with bacterial infection. However, in critically ill patients with non-infectious diseases, PCT values are usually < 0.5 ng/mL. The higher levels of PCT in DRESS may be due to drug-specific T-cell activation, which releases many cytokines like IL-2, IL-5, IL-6, TNF-α, and IFN-γ. Said et al observed elevated serum PCT (>0.5 ng/mL) in 31.9% patients diagnosed with DRESS without bacterial infection (91).22-26 In our study, PCT levels exceeded 0.5 ng/mL in 90% of SJS/TEN patients and all DRESS with persistently high levels even after D7. Notably, the average PCT levels in patients with comorbidities, CTD, and infections were in the septic range [Table 1].
Ferritin levels higher than 591.5 ng/mL have been suggested as an independent prognostic predictor of sepsis.5 Using the 600 ng/mL value as a marker of sepsis, we noted that the ferritin levels in culture-positive SJS/TEN (1462 ng/mL i.e. 7x above normal) were higher than overall SJS/TEN levels (877 ng/mL i.e. 4x above normal) and culture-negative SJS/TEN (399 ng/mL i.e. 2x above normal) indicating that it is a good marker of infection and inflammation in SCAR. The value of serum ferritin on both days was above 600 ng/mL and below 600 ng/mL among the culture-positive and culture-negative group of the SJS/TEN group, respectively. Given that infections can be a confounding factor for interpreting elevated IM in the septic range, it is important to recognise that higher levels are seen in sepsis as compared to the drug reaction alone.
Comparison of the IM with the severity of SJS/TEN showed baseline ferritin as the only marker with a significant positive correlation (p-value- 0.03, rho- 0.337), indicating its potential to reflect disease severity on the D0. Our study also revealed that a severe presentation of SJS/TEN at the time of admission can cause a significant positive increase in PCT, ESR, and ferritin on D7 [Table 2]. None of the markers performed at the time of admission could predict the severity of the disease on the D7 though D0 ferritin had the lowest p-value with positive correlation (p-value- 0.066, rho- 0.441) [Table 2]. Also, the D7 markers did not correlate with D7 disease severity and response. This may be due to the delay in a decrease of the markers as compared to the patient response. This indicates that the clinical response precedes the biochemical response. Therefore, our study indicated that while our markers have the potential to reflect the disease severity on only on D0, their role at a later stage needs to be further studied. Pan et al also noted that the ferritin levels correlate with the severity of drug reactions in the early stage. They found that the serum ferritin level was significantly higher in the SCAR group compared with the non‐severe SCARs group (P<.001) and a higher level of serum ferritin was associated with more severe outcomes.7
Recovery
The average duration of the hospital stay in patients with DRESS was lower than in the SJS/TEN group. However, the average overall recovery period in DRESS may range from 6 to 9 weeks but can persist for several weeks to months with relapses in more than 20% of cases.27 The length of stay in SJS/TEN showed variation across different studies. A meta-analysis of 42 studies observed that the average length of stay was 19.9 days. In a single-centre study, the 11-year experience of 192 patients of SJS/TEN found that female patients had significantly longer inpatient stays (21 days) as compared to 11 days for males.28,29 Higher baseline SCORTEN values and TC were significant markers of increased recovery time with a positive correlation, while a high PCT marked a delayed recovery on D7 [Table 3] [Figures 3 and 4]. Rhyou HI et al noted that that the patients with high PCT at the time of admission had A poor prognosis with a longer duration for remission and recovery period.18 Some researchers suggested D0 PCT levels to be considered as an independent prognostic marker for SJS/TEN, while others found PCT > 0.67 ng/mL as a significant risk factor for death during hospitalisation.4,30 We observed that though increased PCT levels were seen in both days, the D7 value correlated with severity and recovery than the baseline value [Tables 1 and 4, Figure 4]. Our study showed that a decrease in PCT (76%) was a better prognostic marker than a decrease in EC in patients with DRESS (41%). Therefore, PCT is a valuable tool in distinguishing different types of SCARs, identifying patients with superadded sepsis, and monitoring recovery. The SCORTEN score is a validated, most preferred disease severity score and mortality predictor used in many countries.31 In our study, the baseline SCORTEN scores when combined with IMs like ferritin and PCT were good predictors of severity. Though NLR has been reported in many studies to be significantly high among SJS/TEN compared to other types of cutaneous drug reactions, in our study did not reflect the severity or the recovery rate. A high TC at admission indicated a delayed recovery.
Limitations
One of the limitations of this study is that marker analysis was performed at baseline and on D7, but not after complete recovery. While the D7 marker definitely indicates a trend, confirmatory conclusions about marker behaviour during recovery may require the IM levels at the time of discharge. Furthermore, a therapeutic confounding factor analysis was not done and will require a larger study group.
Conclusion
In conclusion, the progression of IMs in SCARs follows the clinical course of illness. Most SCARs showed a decrease in IMs over the course of one week, except in SLE/TEN with connective tissue diseases and culture positivity. IMs in DRESS were significantly lower than SJS/TEN, except TCs and eosinophil levels. IMs like ferritin and PCT along with routine haematological investigation, aid in identifying the severity, differentiating it among patients with comorbidities, and help in predicting the recovery time in SCARs. The study indicated that the markers have the potential to reflect the disease severity on admission; their role at a later stage has to be further studied.
Ethical approval
The research/study was approved by the Institutional Review Board at Goa Medical college, number GMCIEC/2022/126, dated 6/9/22.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Severe cutaneous adverse reactions. Indian J Dermatol Venereol Leprol. 2011;77:3-6.
- [CrossRef] [PubMed] [Google Scholar]
- RegiSCAR DRESS (Drug reaction with eosinophilia and systemic symptoms) validation scoring system and Japanese consensus group criteria for atypical drug-induced hypersensitivity syndrome (DiHS): A comparative analysis. Indian Dermatol Online J. 2022;13:40-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Physiology, acute phase reactants. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519570/
- [Google Scholar]
- Sepsis assessment in SJS/TEN: An important point overlooked? An Bras Dermatol. 2019;94:773-4.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of serum ferritin on the prognosis of patients with sepsis: Data from the MIMIC-IV database. Emerg Med Int. 2022;2022:2104755.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The relationship between serum ferritin level and clinical outcomes in sepsis based on a large public database. Sci Rep. 2023;13:8677.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Association between serum ferritin and the severity of drug eruptions. J Clin Lab Anal. 2020;34:e23043.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Significance of elevated serum LDH (lactate dehydrogenase) activity in atopic dermatitis. J Dermatol. 1990;17:477-81.
- [CrossRef] [PubMed] [Google Scholar]
- D-dimer levels as a marker of cutaneous disease activity: Case reports of cutaneous polyarteritis nodosa and atypical recurrent urticaria. JAMA Dermatol. 2014;150:880-4.
- [CrossRef] [PubMed] [Google Scholar]
- Mank V, Azhar W, Brown K. Leukocytosis. 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560882/ [accessed on 10 Feb 2025].
- The correlation of neutrophil-lymphocyte ratio and eosinophil count with SCORTEN in SJS/TEN. Clin Cosmet Investig Dermatol. 2022;15:547-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Eosinophils in skin diseases. Semin Immunopathol. 2021;43:393-409.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermatological adverse drug reactions due to systemic medications – A review of literature. J Pak Assoc Dermatol [Internet].. 2017;16:28-3.
- [Google Scholar]
- Prevalence of cutaneous drug eruption in hospitalized patients: A report from Sina Hospital of Tabriz. Iran J Dermatol. 2009;12:16-9.
- [Google Scholar]
- Drug reaction with eosinophilia and systemic symptoms: Observations from a tertiary care institution. Indian J Dermatol Venereol Leprol. 2014;80:221-8.
- [CrossRef] [PubMed] [Google Scholar]
- Drug-induced Stevens-Johnson syndrome in Indian population: A multicentric retrospective analysis. Niger J Clin Pract. 2017;20:978-83.
- [CrossRef] [PubMed] [Google Scholar]
- Drug reaction with eosinophilia and systemic symptoms (DRESS): An interplay among drugs, viruses, and immune system. Int J Mol Sci. 2017;18:1243.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Procalcitonin as a diagnostic marker for differentiating DRESS syndrome from bacterial infection. Ann Allergy Asthma Immunol. 2019;123:307-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophil-to-lymphocyte ratio is a prognostic predictor in emergency department patients with cutaneous adverse drug reaction. Am J Emerg Med. 2021;47:279-83.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and impact of reported drug allergies among rheumatology patients. Diagnostics (Basel). 2020;10:918.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Serum procalcitonin as a biomarker differentiating delayed-type drug hypersensitivity from systemic bacterial infection. J Allergy Clin Immunol. 2013;132:981-3.
- [CrossRef] [PubMed] [Google Scholar]
- High procalcitonin levels in patients with severe drug reactions. Arch Dermatol. 2007;143:1591.
- [CrossRef] [PubMed] [Google Scholar]
- Marked elevation of procalcitonin in a patient with a drug related infusion reaction to rituximab. Clin Chem Lab Med. 2016;54:e101-3.
- [CrossRef] [PubMed] [Google Scholar]
- Serum procalcitonin for differentiating bacterial infection from disease flares in patients with autoimmune diseases. J Korean Med Sci. 2011;26:1147-51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- DRESS is a cause of increased serum procalcitonin level without bacterial infection. P94 Clinical & Translational All. 2014;4
- [CrossRef] [PubMed] [Google Scholar]
- Drug-induced hypersensitivity syndrome with high procalcitonin levels due to piperacillin/tazobactam and meropenem: A case report. Front Med (Lausanne). 2022;9:951714.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- DRESS syndrome: A literature review and treatment algorithm. World Allergy Organ J. 2023;16:100673.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of multiple medical interventions on mortality, length of hospital stay and reepithelialization time in toxic epidermal necrolysis, Steven-Johnsons syndrome, and TEN/SJS overlap - metanalysis and metaregression of observational studies. Burns. 2022;48:263-80.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics associated with disease prevalence, SCORTEN, length of stay, and mortality in hospitalized SJS/TEN patients: A single-center, eleven-year experience. Burns Open. 2022;6:110-5.
- [CrossRef] [Google Scholar]
- RDW-SD and PCT are potential prognostic factors for in-hospital death in patients with Stevens-Johnson syndrome/Toxic epidermal necrolysis. Allergy Asthma Immunol Res. 2023;15:812-24.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- SCORTEN accurately predicts mortality among toxic epidermal necrolysis patients treated in a burn center. J Burn Care Res. 2008;29:141-6.
- [CrossRef] [PubMed] [Google Scholar]






