Translate this page into:
A diagnostic challenge: Pathergy positivity in papulopustular lesions of Behçet disease mimicking acute localised exanthematous pustulosis
Corresponding author: Dr. Ecem Bostan, Cihanbeyli Public Hospital, Dermatology and Venereology Clinic, Cihanbeyli, Konya, Turkey. bostanecem@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bostan E, Gulseren D, Akdogan N, Ozdemir DA, Karadag O. A diagnostic challenge: Pathergy positivity in papulopustular lesions of Behçet disease mimicking acute localised exanthematous pustulosis. Indian J Dermatol Venereol Leprol 2022;88:817-19.
Sir,
Behçet disease is characterised by uveitis, recurrent oral/genital aphthae, erythema nodosum, papulopustular skin lesions, pathergy positivity besides neurologic, gastrointestinal and cardiovascular manifestations.1 Superficial folliculitis, pityrosporum folliculitis, eosinophilic pustular folliculitis, pustular psoriasis, subcorneal pustular dermatosis and acute localised exanthematous pustulosis are some other cutaneous diseases which present with pustular eruption.1 We present a case of pathergy positivity mimicking acute localised exanthematous pustulosis in a patient diagnosed with Behçet disease.
A 38-year-old woman was referred to the dermatology clinic for a pustular eruption on her left inner thigh which started one week ago. She had recurrent attacks of folliculitis involving both lower and upper extremities in the past 16 years. Her current lesions appeared after an epilation session as a few grouped pustules on her left inner thigh. She was started on oral ampicillin-sulbactam with a provisional diagnosis of folliculitis four days ago. However, the pustular eruption continued to progress despite the oral antibiotic treatment. There was no history of any other drug intake which could have provoked the development of papulopustular lesions. She reported having recurrent oral aphthae over three times within a year. She did not have any history of genital ulceration, pain or swelling in the joints, abdominal/chest pain or dyspnoea. There was no history suggestive of uveitis, erythema nodosum, photosensitivity, malar rash, alopecia, deep vein thrombosis, periodic fever, neurologic, gastrointestinal, genitourinary and cardiovascular symptoms which could be associated with Behçet disease or other rheumatologic disorders. Ophthalmologic examination was normal. Neurologic, gastrointestinal and cardiovascular examination findings did not reveal any abnormalities. The family history was unremarkable. Dermatological examination revealed a crusted plaque surrounded by discrete and confluent non-follicular pustules on erythematous base on medial aspect of left thigh [Figure 1a]. Our provisional diagnoses included acute localised exanthematous pustulosis, pathergy positivity of Behçet disease, pustular pyoderma gangrenosum, and infective folliculitis. Fungal and aerobic cultures taken from the pustules were negative. Anti-nuclear antibody, rheumatoid factor, anti-double-stranded DNA antibody, anti-neutrophilic cytoplasmic antibodies, complement C3, complement C and extractable nuclear antibodies were negative. A pathergy test was done and a biopsy was taken from the pustular eruption. Pathergy test was positive [Figure 1b]. One week after the initiation of treatment with systemic and topical corticosteroid, regression of pustules leaving desquamation and pale erythematous patches were noted [Figure 1c]. Skin biopsy revealed subcorneal/intraepidermal spongiform pustule formation expanding into the dermis [Figure 2]. According to the international criteria for Behçet disease point score system, a patient having 4 points or above was classified as having Behçet disease.2 In this point score system, ocular lesions, oral aphthae and genital aphthae are each assigned two points, while skin manifestations, central nervous system involvement and vascular manifestations are given one point each.2 The pathergy test, when positive, is given one point.2 Our patient had recurrent oral aphthae (two points), skin lesions (papulopustular eruption - one point) and a positive pathergy test (one point). Thus she scored four points which fulfilled the diagnostic criteria for Behçet disease. Additionally, she had HLA-B51 positivity which is a risk allele for Behçet disease. A partial improvement of cutaneous eruption is reported on treatment with oral colchicine3 and this was noticed in our patient as well. Even though the patient performed the epilation procedure upon the entire lower extremity, we believe the friction between the upper legs might be the contributing factor to the emergence of papulopustular eruption and pathergy positivity. Therefore, a final diagnosis of the papulopustular eruption of Behçet disease with pathergy positivity, mimicking acute localised exanthematous pustulosis was made.

- Crusted plaque surrounded by pustules on erythematous base on medial aspect of left thigh

- Pathergy test positivity showing erythematous papules and pustules
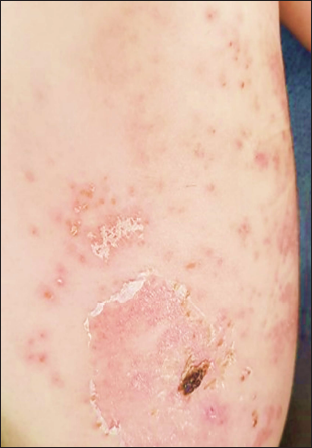
- Regression of the pustules and desquamation after treatment
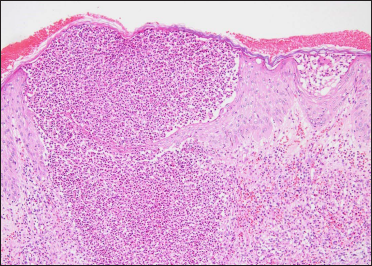
- Subcorneal intraepidermal spongiotic pustule, expanding into dermis, erythrocyte extravasation and oedema in the adjacent dermis, infiltrate consisting of mainly neutrophils and eosinophils (Hematoxylin and eosin, ×100).
Acute localised exanthematous pustulosis is an adverse cutaneous drug eruption characterised by non-follicular, sterile pustule formation in a localised area of the body. The most common incriminated drugs are beta-lactam antibiotics such as cephalosporins, amoxicillin, ampicillin and macrolides.4 Pustular eruption starts within a few days after the drug initiation and systemic symptoms such as fever and fatigue may also accompany.4 Pustular eruption on the left inner thigh in our patient had started after an epilation session similar to her previous attacks of folliculitis underlined the fact that her lesions were triggered by traumatic procedures which in a way resembles the pathergy positivity. Continuous friction between the upper inner thighs might have created a trauma which further provoked the expansion of the pustular eruption. We diagnosed her lesions as the papulopustular eruption of Behçet disease with pathergy positivity with the help of histopathological confirmation which showed subcorneal spongiform pustule formation infiltrated predominantly by neutrophils and eosinophils and no follicular based inflammation. The papulopustular lesions of Behçet disease may show various histopathological findings such as leukocytoclastic vasculitis, perifollicular/perivascular infiltration, suppurative folliculitis or intrafollicular abscess formation.5,6 Ergun et al.7 reported that intraepidermal pustule formation, polymorphonuclear and lymphocytic aggregates were the histopathological hallmarks of the pustular lesions induced by pathergy test in patients with Behçet disease, similar to our case which showed subcorneal pustule formation with neutrophilic, interstitial and lymphoplasmacytic infiltrate.
We would like to emphasize that patients with Behçet disease might be prone to develop papulopustular eruptions exacerbated by trauma, which may mimic other pustular skin diseases including acute localised exanthematous pustulosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Clinical and pathological manifestations with differential diagnosis in Behçet’s Disease. Patholog Res Int. 2012;2012:690390.
- [CrossRef] [PubMed] [Google Scholar]
- The International Criteria for Behçet’s Disease (ICBD): A collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014;28:338-47.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Behcet’s syndrome. Rheumatology (Oxford). 2020;59:iii108-17.
- [CrossRef] [PubMed] [Google Scholar]
- Two cases of amoxycillin-induced follicular acute localised exanthematous pustulosis. Australas Dermatol. 2017;58:e23-e25.
- [CrossRef] [PubMed] [Google Scholar]
- Can specific vessel-based papulopustular lesions of Behçet’s disease be differentiated from nonspecific follicular-based lesions clinically? Int J Dermatol. 2006;45:814-8.
- [CrossRef] [PubMed] [Google Scholar]
- Histopathological and clinical evaluation of papulopustular lesions in Behçet’s disease. Clin Exp Rheumatol. 2015;33:S101-6.
- [PubMed] [Google Scholar]
- The histopathology of pathergy: A chronologic study of skin hyperreactivity in Behçet’s disease. Int J Dermatol. 1998;37:929-33.
- [CrossRef] [PubMed] [Google Scholar]





