Translate this page into:
A family of Bart-Pumphrey syndrome
2 1st Otorhinolaringology-Head and Neck Surgery Clinic, Ankara Numune Education and Research Hospital, Ankara, Turkey
Correspondence Address:
M�zeyyen G�n�l
Yildiz Evler Mahallesi, 742. Sok. Aykon Park Sitesi, A Blok No: 3/3 �ankaya/Ankara
Turkey
| How to cite this article: G�n�l M, G�l �, Hizli P, Hizli �. A family of Bart-Pumphrey syndrome. Indian J Dermatol Venereol Leprol 2012;78:178-181 |
Abstract
Bart-Pumphrey syndrome (BPS) is an autosomal-dominant disorder characterized by hearing loss, leukonychia, knuckle pads and palmoplantar keratoderma. Two mutations in the extracellular domain of GBJ2 are resposible for this syndrome. To date, less than 10 case reports or clinical series about BPS have been published in the literature. Hearing loss and knuckle pads are the more commonly seen findings of this syndrome. Three generations and six family members with variable findings of knuckle pads, leukonychia, hearing loss and palmoplantar hyperkeratosis were presented in this report. We want to emphasize that dermatogists must be alert during the evaluation of these findings because some findings of this disorder may be vague or absent.Introduction
Bart-Pumphrey sydrome (BPS) or Schwann syndrome is a rare autosomal-dominant disorder caused by connexin 26 mutation. [1],[2],[3] Bart and Pumphrey reported a six-generation family with leukonychia, knuckle pads and congenital deafness. Some family members also had palmoplantar keratoderma. [4] Before the report of Bart and Pumphrey, Schwann had reported a child who was the only member of his family to manifest all of these findings. [4] Up to date, only a few case reports of BPS have been published in the literature.
We present a three-generation family with six members who had at least one finding of BPS.
Case Reports
Case 1
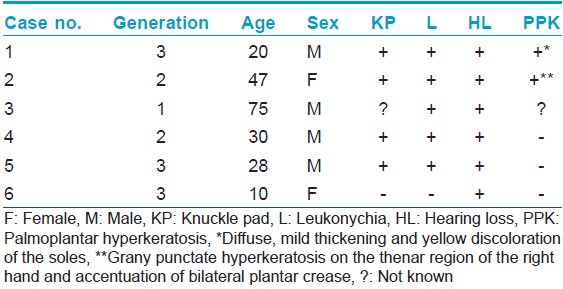
A 20-year-old male patient was admitted to our clinic with hyperkeratotic papules on his hands. In dermatological examination, multiple knuckle pads were detected on the dorsal aspects of the interphalangeal joints of the hands and feet (particularly on the proximal interphalangeal joints), metacarpophalangeal joints of both hands and right wrist. There were atrophic scars due to cryotherapy on the same location with previously described lesions. Knuckle pads had been misdiagnosed as verruca vulgaris in another medical center. He also had total leukonychia on whole nails of both hands and bilateral thumb nails [Figure - 1]. Diffuse, mild thickening and yellow discoloration of the soles was also detected [Figure - 2]. His dermatological findings had begun in childhood. All audiological tests showed mild bilateral sensorineural hearing loss [Table - 1]. The general physical examination was normal, except for dermatological findings and hearing loss.
 |
| Figure 1: Knuckle pads and leukonychia are seen on the hands and feet of case 1 |
 |
| Figure 2: Plantar yellowish hyperkeratosis and knuckle pad in the right wrist of case 1 |
Case 2
She was a 47-year-old female patient and mother of case 1. She attended our clinic by our invitation. She had bilateral congenital moderate hearing loss and she has been using hearing aids. Dermatological examination showed knuckle pads on the 4 th and 5 th metacarpophalangeal joints of the right hand, leukonychia on the whole nails of both hands and 1 st , 2 nd and 3 rd nails of the feet [Figure - 3]. Grany punctate hyperkeratosis on the thenar region of the right hand and accentuation of bilateral plantar crease were determined [Figure - 4]a and b; [Table - 1]. She was healthy otherwise. Her father and mother were closely consanguineous (primary relative). She had four sisters and three brothers. She stated that her father and one of her brothers had similar findings (hearing loss, leukonychia and knuckle pads), but other siblings were normal. She denoted that her mother was normal. She had three sons and one daughter. Two of her sons and the daughter also showed symptoms of BPS. One of her sons was case 1 [Figure - 5].
 |
| Figure 3: Leukonychia of the hands and feet nails and knuckle pads over the metacarpophalangeal joints is seen in case 2 (reddish-brown hue on the nails of feet caused by using of henna) |
 |
| Figure 4: (a, b) Grany appearence of the thenar region of the right hand of case 2 and the accentuation of plantar creases is seen (small figure) |
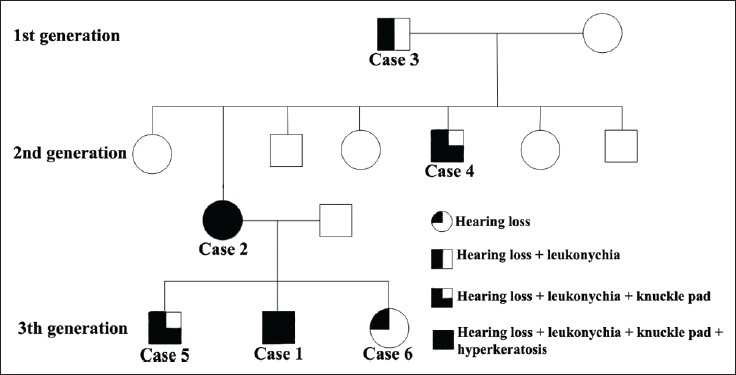 |
| Figure 5: Family pedigree showing variable expression of findings |
Case 3
This patient, the father of case 2, was reported by his daughter to have had leukonychia and hearing loss [Table - 1]. His daughter could not remember other dermatological findings of the syndrome. He could not attend our clinic despite the invitation, because he was living in a distant city.
Case 4
He was a 30-year-old male patient and brother of case 2. We could not evaluate him as he refused our invitation. Case 2 defined that he had hearing loss, leukonychia and knuckle pads [Table - 1].
Case 5
The patient was 28-years old and he has leukonychia, knuckle pads and hearing loss [Table - 1]. The information about this patient was learned from his mother, case 2, because he could not attend our clinic for examination.
Case 6
She was a 10-year-old girl. She was the sister of case 1 and daughter of case 2. There were no pathologic findings on dermatological examination. Only bilateral mild hearing loss was detected by audiogram [Table - 1].
Discussion
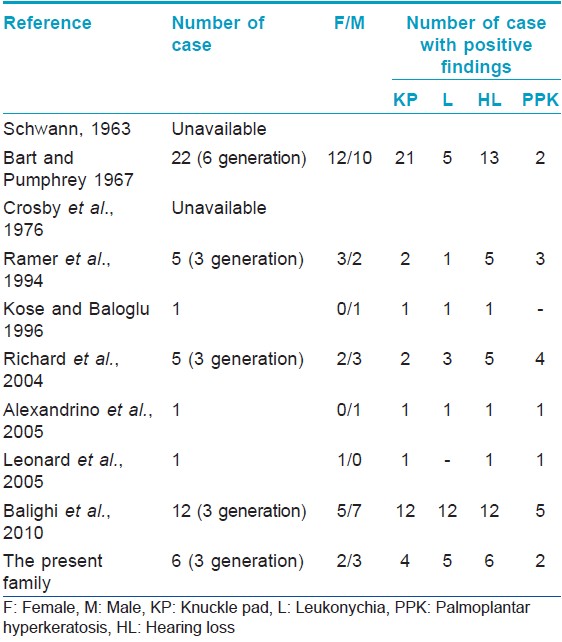
BPS is an autosomal-dominant disorder characterized by knuckle pads, leukonychia, palmoplantar keratoderma and hearing loss. To date, the number of case reports or clinical series about BPS is less than 10. [1],[3],[4],[5],[8],[9],[10] Hearing loss and knuckle pads are the most common findings of this syndrome. Leukonychia and palmoplantar hyperkeratosis are seen less frequently in BPS [Table - 2]. In the present family, hearing loss has been detected in all of the cases with BPS, although the other symptoms have shown variable presentation among the members of the family with BPS. This is similar to the current literature.
Knuckle pads are circumscribed, hyperkeratotic or fibrous growths over the dorsal aspects of the small joints of hands or feet. [5] Knuckle pads were the primary complaint of case 1, and they were misdiagnosed as verruca vulgaris. Most of the lesions localized on the proximal interphalangeal joints, and two lesions presented over the inner surface of the wrist of the right hand. Location of knuckle pads over the wrist was reported by Ramer et al., but the lesion was over the dorsum of the wrist in this case. [6]
Leukonychia that may be seen in BPS is defined as whiteness of nails that can occur either in patches or involving the total nail. Large keratohyaline granules are found in the keratinocytes, and the keratohyaline-containing cells reflected light, resulting in a white nail appearence. [7] Leukonychia is usually autosomal dominantly inherited in syndromes including BPS. [6] Total leukonychia with variable number of nail involvement was seen in each of our patients. The present family has supported the autosomal-dominant inheritance pattern with variable penetrance.
Palmoplantar hyperkeratosis of BPS may be diffuse and striate, with accentuation of crease patterns and with grainy surface. [3],[6],[8],[9] Moreover, the severity and pattern of palmoplantar hyperkeratosis may be variable in members of the same family, such as in the present family. We detected a diffuse patern of keratoderma on soles of case 1, but grainy appearence on the right palm of case 2 and accentuation crease pattern on the soles of the same patient. There was no palmoplantar hyperkeratosis in case 6. We do not know whether there is palmoplantar hyperkeratosis in our other patients and the pattern of hyperkeratosis. Mild hyperkeratosis may be ignored by the patients. We detected hyperkeratosis during the examination of cases 1 and 2, although the patients were not aware of their conditions.
In BPS, hearing loss is generally of the sensorineural type. But, mixed sensorineural and conductive loss may also be seen. [6] Hearing loss was of the sensorineural type in all cases with different severity levels (case 1, case 2 and case 6).
To date, there have been two observed mutated residues, N54K and G59S, which are responsible for the syndrome. Both mutations are in the extracellular domain of GBJ2, the gene encoding connexin-26 (C×26). Mutations in C×26 may be the cause of both non-syndromic and syndromic deafness associated with skin disorder, such as Vohwinkel syndrome and keratitis-ichthyosis deafness syndrome, besides BPS. C×26 is in gap junctions and plays a role in exchange of ions and small molecules between adjacent cells by forming intercellular channels. [2] Richard et al. investigated GJB2 mutations in a family of BPS, and reported that immunostaining of C×26 was weak or absent in lesional palmar and knuckle skin, although its adnexal expression and other epidermal connexins were not altered. They found C×30 compensatory overexpression throughout the spinous cell layers in their investigation. The autors emphasized that GJB2 mutations were responsible for dermatological disorders associated with syndromic hearing loss. [10] We could not investigate GJB2 mutation in our cases.
We present this family because of the rarity of this syndrome. We want to emphasize that some findings of this disorder may be vague or absent, even withinin the same family. This may show no complete penetrance of mutations in this syndrome or effects of other unknown factors. Dermatogists must be alert during the evaluation of these findings for a proper diagnosis and must perform complete dermatological examination including nails, hair and mucosa. Patients may only suffer from one symptom of this syndrome, and may ignore other symptoms that are mild and familial, such as the present cases.
| 1. |
Alexandrino F, Sartorato EL, Marques-de-Faria AP, Steiner CE . G59S Mutation in the GJB2 (Connexin 26) Gene in patient with Bart-Pumphrey syndrome. Am J Med Genet Am 2005;136:282-4.
[Google Scholar]
|
| 2. |
Lee JR, White TW. Connexin-26 mutations in deafness and skin disease. Expert Rev Mol Med 2009;11: e35.
[Google Scholar]
|
| 3. |
Balighi K, Moeineddin F, Lajevardi V, Ahmadreza R. A family with leukonychia totalis. Indian J Dermatol 2010;55:102-4.
[Google Scholar]
|
| 4. |
Bart RS, Pumphrey RE. Knuckle pads leukonychia and deafness: A dominant inherited syndrome. N Engl J Med 1967;276:202-7.
[Google Scholar]
|
| 5. |
Burrows NP, Lowell CR. Disorders of connective tissue. In. Burns T, Breathnach S, Cox N, Griffiths C. Rook's Textbook of Dermatology; 8th ed, Vol. 3. Chichester: Wiley-Blackwell; 2010. p. 45-8.
[Google Scholar]
|
| 6. |
Ramer JC, Vasily DB, Ladda RL. Familial leukonychia, knuckle pads, hearing loss, and palmoplantar hyperkeratosis: An additional family with Bart-Pumphrey syndrome. J Med Genet 1994;31:68-71.
[Google Scholar]
|
| 7. |
de D, Handa S. Hereditary leukonychia totalis. Indian J Dermatol Venereol Leprol 2007;73:355-7.
[Google Scholar]
|
| 8. |
Leonard NJ, Krol AL, Bleoo S, Somerville MJ. Sensorineural hearing loss, striate palmoplantar hyperkeratosis, and knuckle pads in a patients with a novel connexin 26 (GJB2) mutation. J Med Genet 2005;42: e2.
[Google Scholar]
|
| 9. |
Richard G, Brown N, Ishida-Yamamoto, Krol A. Expanding the phenotypic spectrum of C×26 disorders: Bart-Pumphrey syndrome is caused by a novel missense mutation in GJB2. J Invest Dermatol 2004;123:856-63.
[Google Scholar]
|
| 10. |
Kose O, Baloglu H. Knuckle pads, leukonychia and deafness. Int J Dermatol 1996;35:728-9.
[Google Scholar]
|
Fulltext Views
6,806
PDF downloads
3,088





