Translate this page into:
A female patient with purpuric lesions
Corresponding author: Professor Sanjay Singh, Department of Dermatology & Venereology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India. stoppeditt@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Agarwal A, Ansari MH, Singh S. A female patient with purpuric lesions. Indian J Dermatol Venereol Leprol 2023;89:757-9
A 24-year-old female presented with red-coloured lesions on her extremities for 4 years and 6 months. She first noticed multiple, asymptomatic, reddish lesions on her lower legs after prolonged walking [Figure 1]. These lesions appeared in crops after periods of prolonged standing or walking or sitting and disappeared in 5–6 days without residual changes. She denied a history of any constitutional symptoms. On examination, multiple petechiae and purpura were seen on the lower limbs. The systemic examination was unremarkable. Laboratory evaluation revealed normal complete blood count, general blood picture and coagulation profile, raised erythrocyte sedimentation rate and serum antinuclear antibodies (indirect immunofluorescence on human epithelioma-2 cells) levels were equivocal. Histopathological examination showed leukocytoclastic vasculitis of the superficial and deep plexuses [Figure 2]. Affected vessels showed moderate deposition of fibrin in and around the vessel wall. Rheumatoid factor and anti-Ro antibodies were positive. Serum protein electrophoresis showed hypergammaglobulinaemia and serum immunoglobulin G levels were raised [2112 mg/dL (normal range 650–1600 mg/dL)].
Question
What is your diagnosis?

- A 24-year-old woman with petechiae and purpura on lower limbs
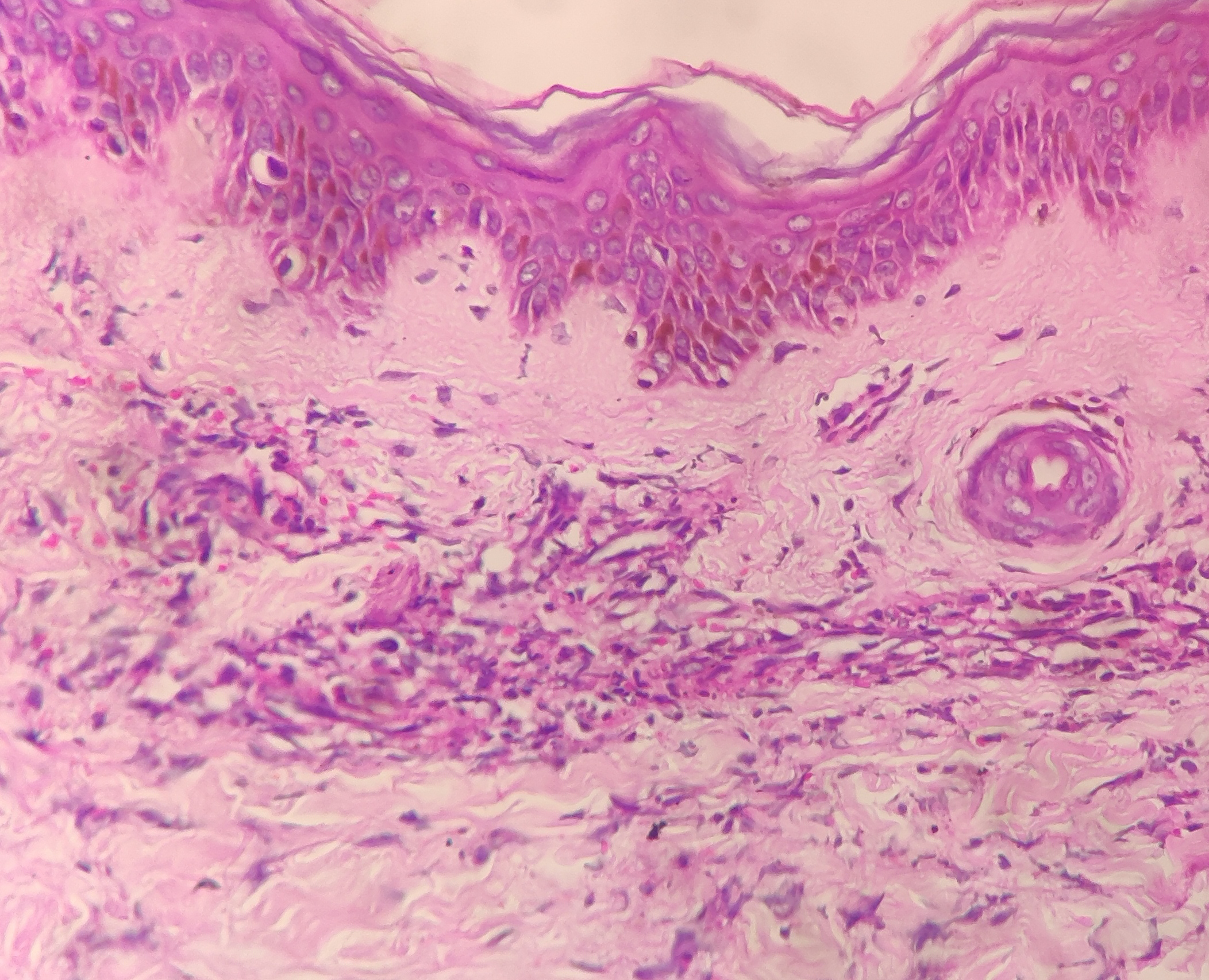
- Leukocytoclastic vasculitis of superficial and deep plexuses (fibrin deposition in the wall, extravasated red blood cells, neutrophilic nuclear dust and perivascular infiltrate) (haematoxylin and eosin, ×400)
Diagnosis
Primary hypergammaglobulinaemic purpura of Waldenström.
Discussion
Hypergammaglobulinaemic purpura of Waldenström is a polyclonal disorder characterised by recurring crops of petechiae and purpura, but there are cascades of other symptoms like different patterns of vasculitis, neutrophilic dermatosis or urticaria. Although the exact pathogenesis is not known, the symptoms are attributed to the deposition of immune complexes containing rheumatoid factor in vessel walls. 1 It may be primary or secondary. The primary form of this disease is seen in young females with positive anti-Ro antibodies and is associated with complications during pregnancy like intrauterine growth retardation and neonatal heart block. 2 The secondary form is seen in older adults and is associated with autoimmune diseases like Sjögren syndrome, systemic lupus erythematosus, rheumatoid arthritis, or haematological malignancies. 1 The primary form is diagnosed when a patient, usually a woman of 18–40 years, presents with a history of recurring crops of petechiae mainly on the lower legs after prolonged standing or walking and has raised erythrocyte sedimentation rate, raised rheumatoid factor and raised levels of gamma globulins on serum protein electrophoresis. 1 Histopathology may show leukocytoclastic vasculitis or nonspecific purpura with mild lymphocytic perivasculitis. 1
The present patient demonstrated many of the above-mentioned symptoms but had a complications-free pregnancy and gave birth to a normal healthy baby girl. She had positive anti-Ro antibodies and rheumatoid factor but had an equivocal serum antinuclear antibodies level. Despite this, she had no other features suggestive of sicca syndrome, systemic lupus erythematosus, or rheumatoid arthritis. The normal blood counts and general blood picture and the absence of M-peak on serum protein electrophoresis ruled out haematological malignancies like multiple myeloma. The patient was advised to avoid activities requiring prolonged standing or walking and was started on oral hydroxychloroquine (300 mg daily for 12 weeks and then 200 mg daily).
Before starting treatment, the patient developed skin lesions after about 15 minutes of walking or standing, and the lesions lasted for 5–6 days. During the first 12 weeks of treatment, the lesions appeared after walking or standing for 20–25 minutes and lasted for 2–3 days. Subsequently, in the next 12 weeks, the lesions appeared after 20–35 minutes of walking or standing and lasted for 1–3 days. The number of episodes per month has decreased from 6–7 pre-treatment to 1–2 now.
Even though the condition was first described in 1943, 3 it is still under-reported and misdiagnosed. With this case, we want to draw attention to (1) this rare form of thrombocytopaenic purpura to avoid waste of time and resources on a plethora of unwarranted diagnostic and therapeutic interventions and (2) the usually benign course of primary hypergammaglobulinaemic purpura of Waldenström (with the exception of pregnancy-associated complications).
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Hypergammaglobulinemic purpura of Waldenström. J Am Acad Dermatol. 1990;23:669-76.
- [CrossRef] [PubMed] [Google Scholar]
- Juvenile-onset hypergammaglobulinemic purpura and fetal congenital heart block. J Dermatol. 2006;33:714-8.
- [CrossRef] [PubMed] [Google Scholar]
- Three new cases of purpura hyperglobulinemica. A study in long-standing benign increase in serum globulin. Acta Med Scand. 1952;266:931-46.
- [CrossRef] [PubMed] [Google Scholar]





