Translate this page into:
A painless, solitary, yellow-pink colored, vascularized, firm nodule on the forehead
Corresponding author: Prof. Dr. Aylin Türel Ermertcan, Uncubozkoy Mah., 5501 Sok., 29/5 Manisa, Turkey. draylinturel@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arslan Z, Çetınarslan T, Bali ZU, Evrenos MK, Temiz P, Türel Ermertcan A. A painless, solitary, yellow-pink colored, vascularized, firm nodule on the forehead. Indian J Dermatol Venereol Leprol 2021;87:878-80.
An 88-year-old woman referred to the outpatient clinic for the painless solitary mass on her forehead. History revealed that the lesion showed slow growth and reached its final dimensions in 4 years. A yellow-pink, vascularized firm nodule sized 3.1× 2.8 cm was observed on the forehead during the dermatological examination. There was an ulcer at the center[Figure 1]. The dermoscopic examination was performed with MoleMax × 3, nonpolarized computer-based videodermoscope,×30 magnification. It revealed white-yellow structures, hairpin and linear vessels on yellowish background with a bleeding-ulcerated area in the center[Figure 2]. A wide local excision was performed under local anesthesia. On histopathological examination, tumor showing lobulated growth in the dermis with ulcerated epidermis[Figure 3] and multivacuolated translucent cytoplasm cells combined with basal cells [Figure 4] were observed. Deep and lateral surgical margins were free of tumor cells. There was no lymphadenopathy on cervical ultrasonography and no distant metastasis was detected with radiological examinations such as abdominal ultrasonography, computed tomography imaging of the brain and thorax.

- Yellow-pink colored, vascularized firm nodule on the forehead with a central ulcer in the size of 3.1 cm × 2.8 cm
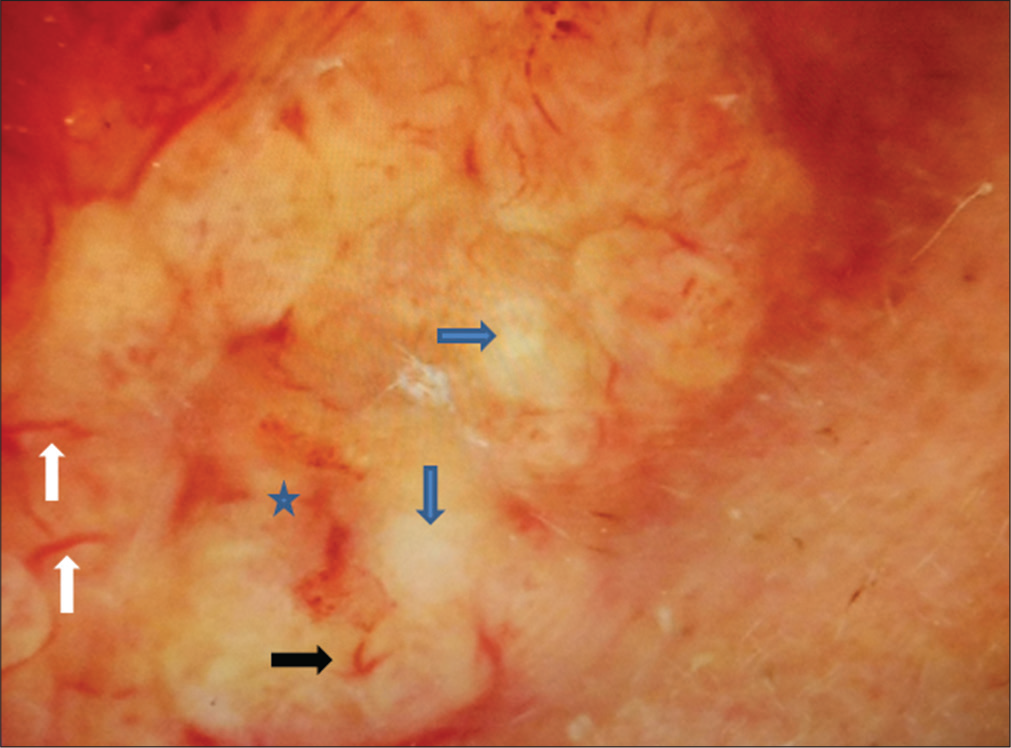
- White arrows show linear vessels, black arrow shows hairpin vessel, blue arrows show white-yellow structures and asterisks shows the bleeding-ulcerated area in the centre on a yellowish background. MoleMax 3, nonpolarized computer-based video dermoscope, ×30 magnification
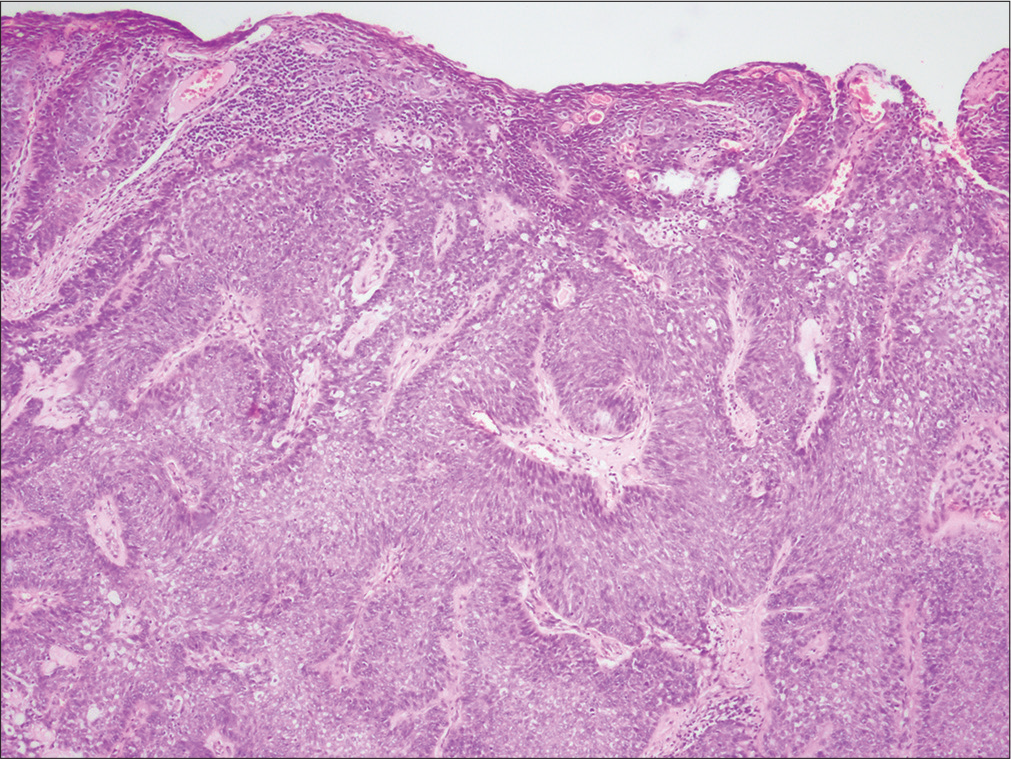
- Tumor composed of clear cells between basaloid cells with epidermal ulceration (H and E, ×40)
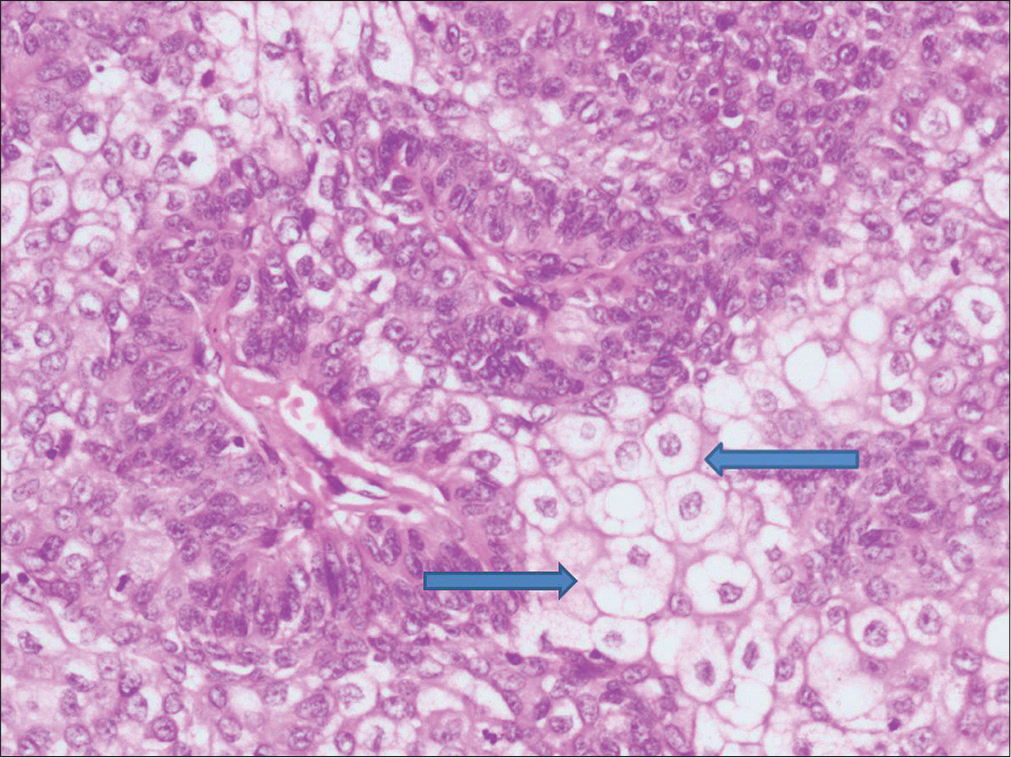
- Sebaceous tumor cells with atypical basaloid cells (H and E, ×200) (arrows show tumor cells)
What Is Your Dıagnosıs?
Diagnosis
Extraocular sebaceous carcinoma
Discussion
Sebaceous carcinoma that constitutes 0.2% to 4.6% of all malignant cutaneous neoplasms is a rare aggressive adnexal tumor arising from sebaceous glands. On the other hand, sebaceous carcinoma is the most common malignancy of the eyelids following basal cell carcinoma and squamous cell carcinoma.Extraocular localization of the sebaceous carcinoma is rare and accounts for 25% of all cases.1 The site of extraocular sebaceous carcinoma is head and neck with parotid glands being the most common followed by nose, face and neck. It has also been reported onthe external genitalia, external auditory canal, axilla, trunk and upper extremity.2 Although most sebaceous carcinomas occur sporadically, risk factors for developing sebaceous carcinoma include older age, history of irradiation, and immunosuppression after solid organ transplantation. These tumors may be a marker of Muir-Torre syndrome, an autosomal dominant disorder, considered to be a subgroup of hereditary nonpolyposis colorectal cancer syndrome (Lynch syndrome).3
Sebaceous carcinoma usually presents as slow-growing, firm, painless, pinkyellowish-red subcutaneous nodule or mass which may ulcerate and bleed spontaneously.1 The differential diagnosis of sebaceous carcinoma includes intradermal nevus, sebaceous adenoma, basal cell carcinoma and squamous cell carcinoma.2 Definitive diagnosis requires histopathological examination. Immunohistochemical staining with epithelial membrane antigen, adipose differentiation-related protein (adipophilin) androgen receptor, BerEP4 (a monoclonal antibody which detects specific epithelial glycoprotein adhesion molecules found on basal cell carcinoma cells) and cytokeratin 7 may be used to confirm the diagnosis and to differentiate basal cell carcinoma and squamous cell carcinoma. Sebaceous carcinomas are epithelial membrane antigen-positive, adipophilin-positive and androgen receptor in nearly 100% of cases.4 In our case, immunohistochemistry showed that the tumor cells were positive for epithelial membrane antigen and high molecular weight cytokeratin. Figure 5 shows the epithelial membrane antigen-positive staining.
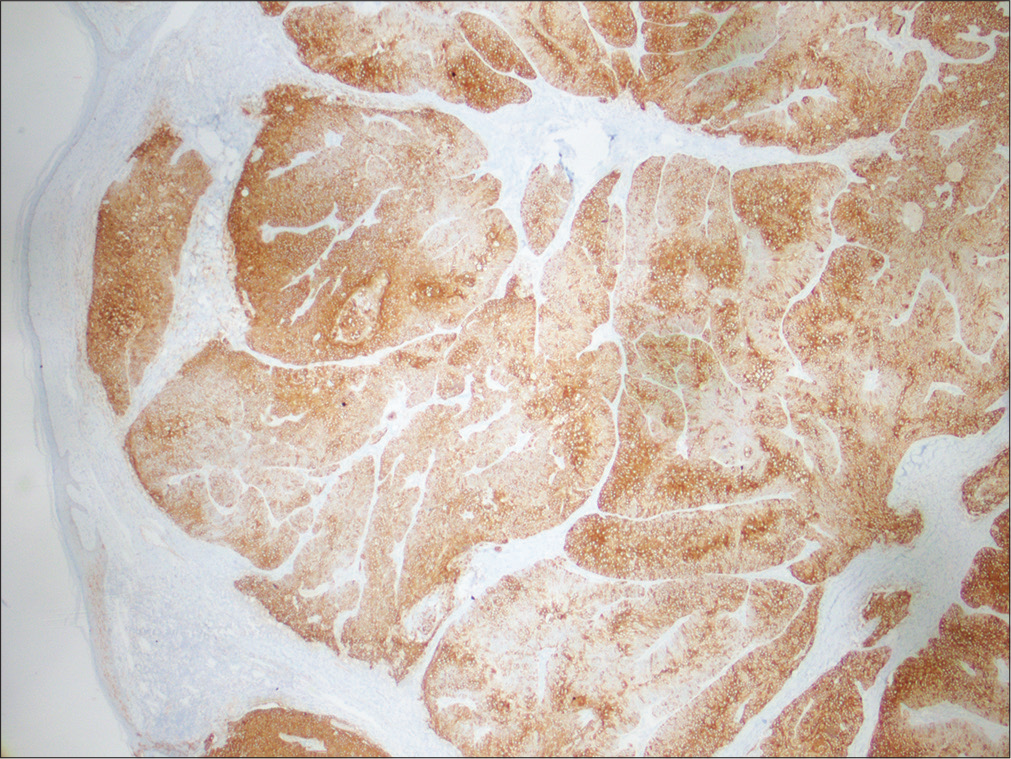
- Tumor cells positive for epithelial membrane antigen(×20)
Dermoscopy is a noninvasive, office based technique used in the diagnosis of malignant and benign skin lesions. Several studies and case reports on dermoscopy of sebaceous carcinoma have been published previously. Horimoto et al. suggested that the combination of four dermoscopic features, whitish-pink areas, yellowish structures, polymorphous vessels and ulceration might be distinctive in extraocular sebaceous carcinoma.5 Moreover, Satomura et al. suggested that polymorphous vessels with yellowish background are the main dermoscopic finding in the diagnosis of sebaceous carcinoma.6 In our case, we observed white-yellow structures, hairpin and linear vessels on yellowish background with a central bleeding-ulcerated area similar to previous reports.
Wide local excision is recommended for treatment of extraocular sebaceous carcinoma because of high local recurrence rate. Distant metastasis and mortality have been reported in 20–25% and 20% of all sebaceous carcinoma cases, respectively.3 It has been suggested that Mohs micrographic surgery should be performed to decrease the rate of local recurrence. In elderly patients, radiotherapy is the treatment of choice for recurrent tumors and metastatic lesions.1
We presented our case due to the rarity of extraocular localization of sebaceous carcinoma. Sebaceous carcinoma needs to be considered in the differential diagnosis of basal cell carcinoma and squamous cell carcinoma, especially in elderly individuals. Dermoscopy is a noninvasive, helpful technique in the differentiation of sebaceous carcinoma from non-melanoma skin cancers. When white-yellow structures, polymorphic vessels with an ulcerated area and yellowish background are observed on dermoscopic examination, sebaceous carcinoma needs to be considered as the preliminary diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Extraocular sebaceous carcinoma: A report of 2 cases. Actas Dermosifiliogr. 2012;103:919-22.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathological features of eyelid skin tumors. A retrospective study of 5504, cases and review of literature. Am J Dermatopathol. 2009;31:256-62.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and survival of sebaceous carcinoma in the United States. J Am Acad Dermatol. 2016;75:1210-5.
- [CrossRef] [PubMed] [Google Scholar]
- Role of immunohistochemistry in the diagnosis of sebaceous carcinoma: A clinicopathologic and immunohistochemical study. Am J Dermatopathol. 2015;37:809-21.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features distinctive for extraocular sebaceous carcinoma. J Dermatol. 2018;45:487-90.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of ocular and extraocular sebaceous carcinomas. J Dermatol. 2017;44:1313-6.
- [CrossRef] [PubMed] [Google Scholar]





