Translate this page into:
A patient with multiple asymptomatic yellow papules on the scalp
Corresponding author: Dr. Ruzhi Zhang, Department of Dermatology, The Third Affiliated Hospital of Soochow University, Changzhou, China. zhangruzhi628@163.com
-
Received: ,
Accepted: ,
How to cite this article: Wang H, Zhang R. A patient with multiple asymptomatic yellow papules on the scalp. Indian J Dermatol Venereol Leprol. 2024;90:244–6. doi: 10.25259/IJDVL_224_2023
A 68-year-old woman presented with numerous asymptomatic yellow papules on the scalp for 20 years, gradually increasing in size and number over time. Recently, a yellowish-red nodule appeared among the existing lesions. The patient had no specific past medical history besides hyperlipidemia.
Physical examination revealed approximately 50 yellow to skin-coloured papules and a yellowish-red nodule on her occipital region [Figure 1]. Dermatoscopy from the yellowish papules revealed a uniform bright yellow structureless material [Figure 2a]. The yellowish-red nodule had dilated capillaries on its surface and lipid accumulation below that [Figure 2b].
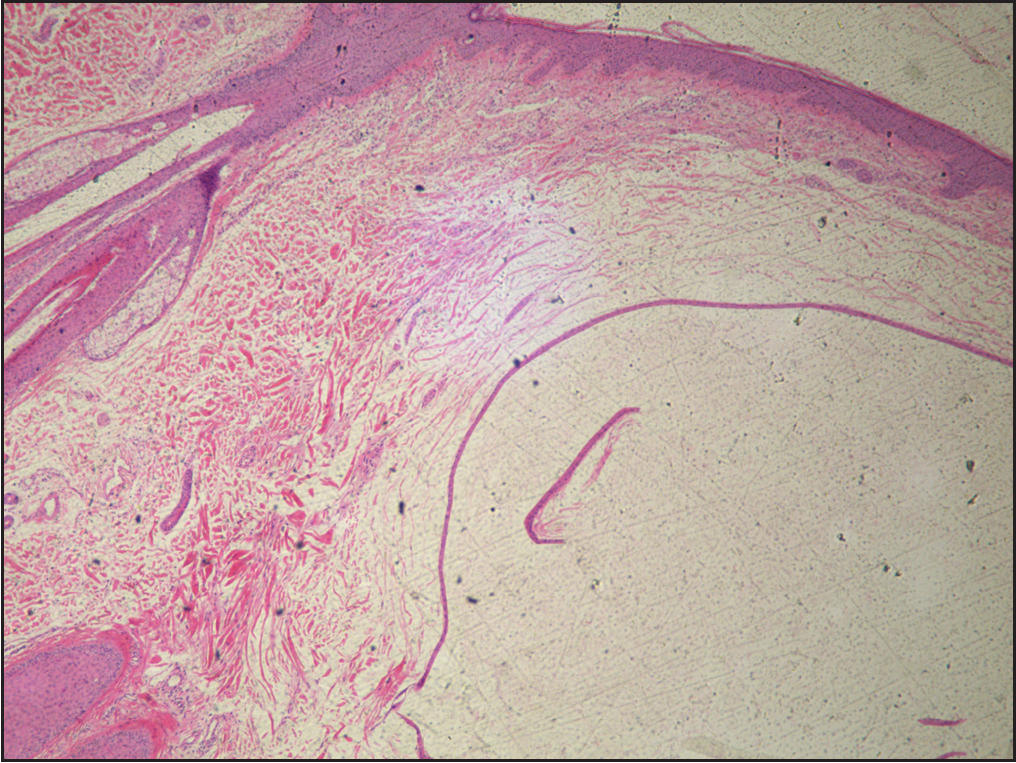
Histopathological analysis of one of the yellow papules showed the presence of a cyst containing eosinophilic keratinous material in the dermis, with the cystic wall consisting of several layers of epithelium without a granular layer. Sebaceous gland lobules were observed near the cystic wall [Figures 3a and 3b]. Histopathology of the yellowish-red nodule revealed nodular masses composed of predominantly lymphocytes and histiocytes in the superficial and mid dermis, with multinucleated giant cells and keratotic material also present [Figures 3c and 3d].
Question
What is your diagnosis?

- Approximately 50 smooth-surfaced, yellow or skin-coloured, dome-shaped papules with diameters ranging from 3–10 mm located on the occipital region

- There was a yellowish-red nodule with a diameter of approximately 7 mm among the yellowish papules
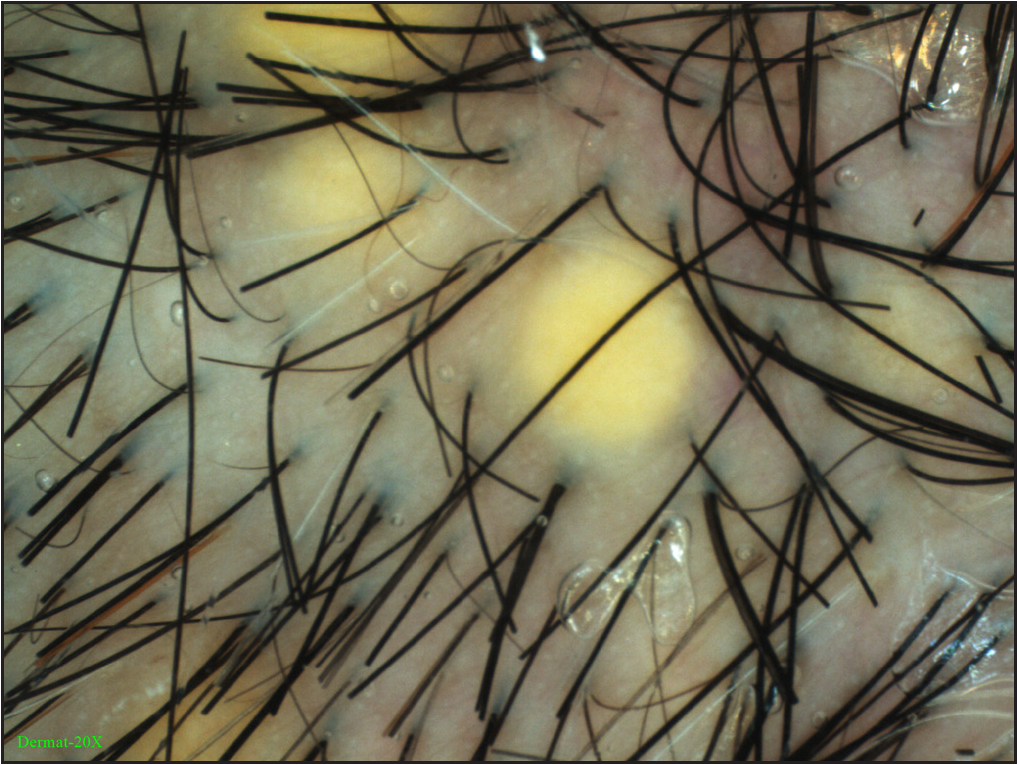
- The yellowish papules revealed a uniform bright yellow structureless material
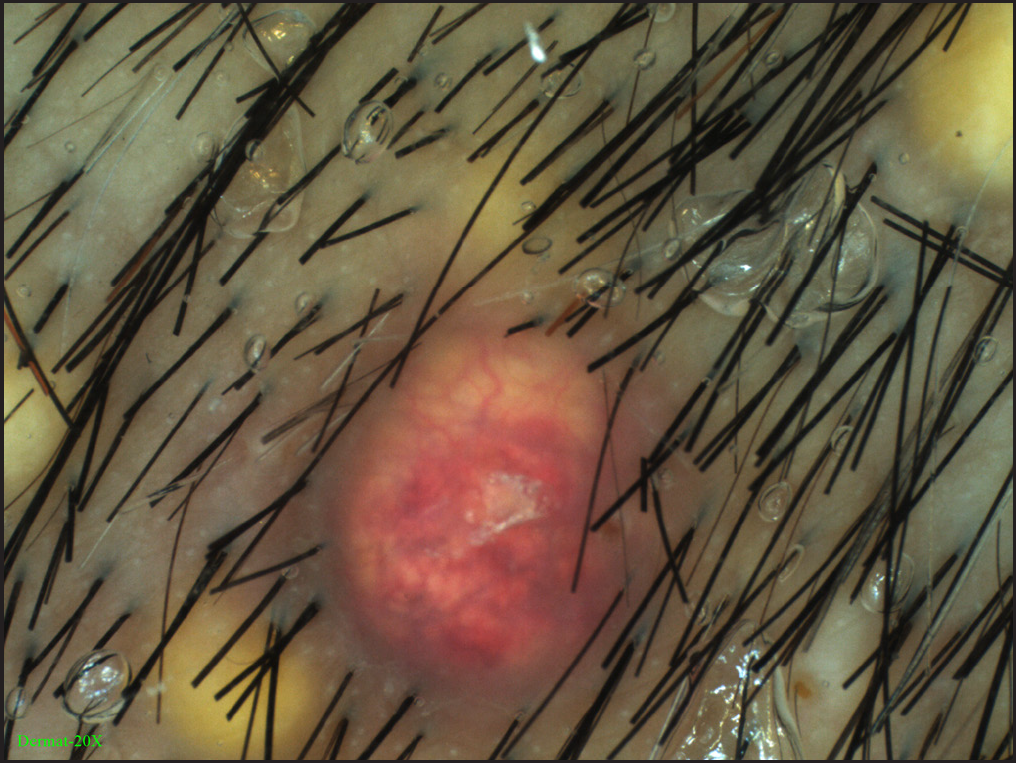
- The yellowish-red nodule had dilated capillaries on its surface and lipid accumulation below that
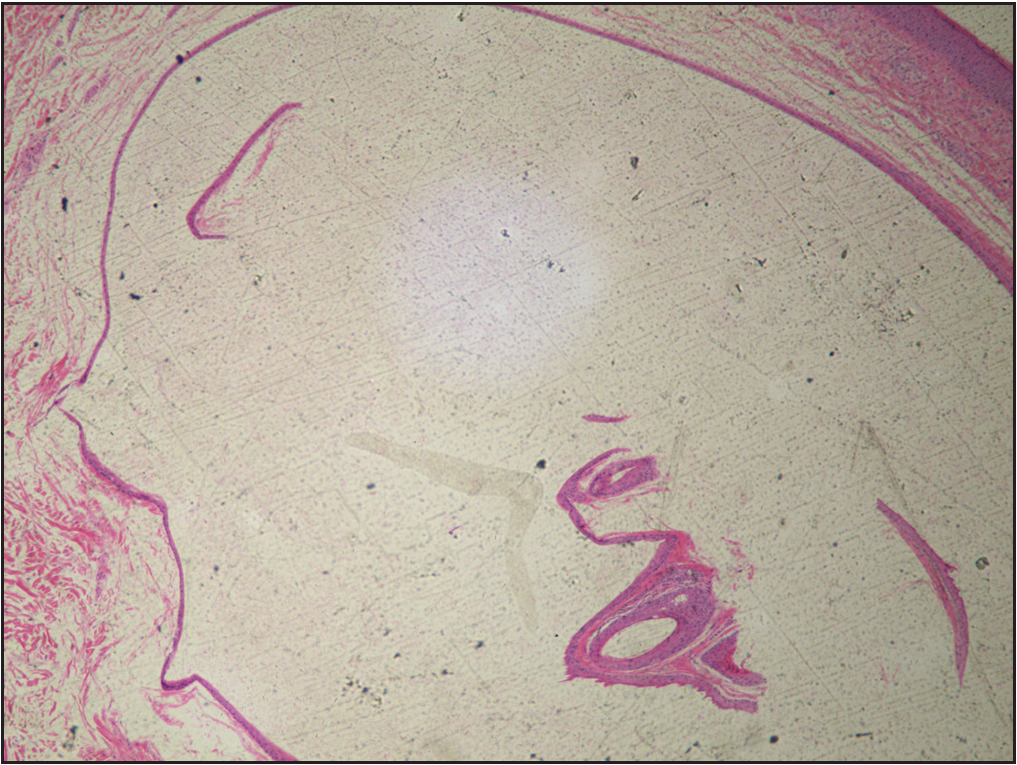
- A cyst contained eosinophilic keratinous materials located in the dermis, with the cystic wall consisting of several layers of epithelium without a granular layer (H&E, 100x)
- Sebaceous gland lobules were observed near the cystic wall (H&E, 100x)
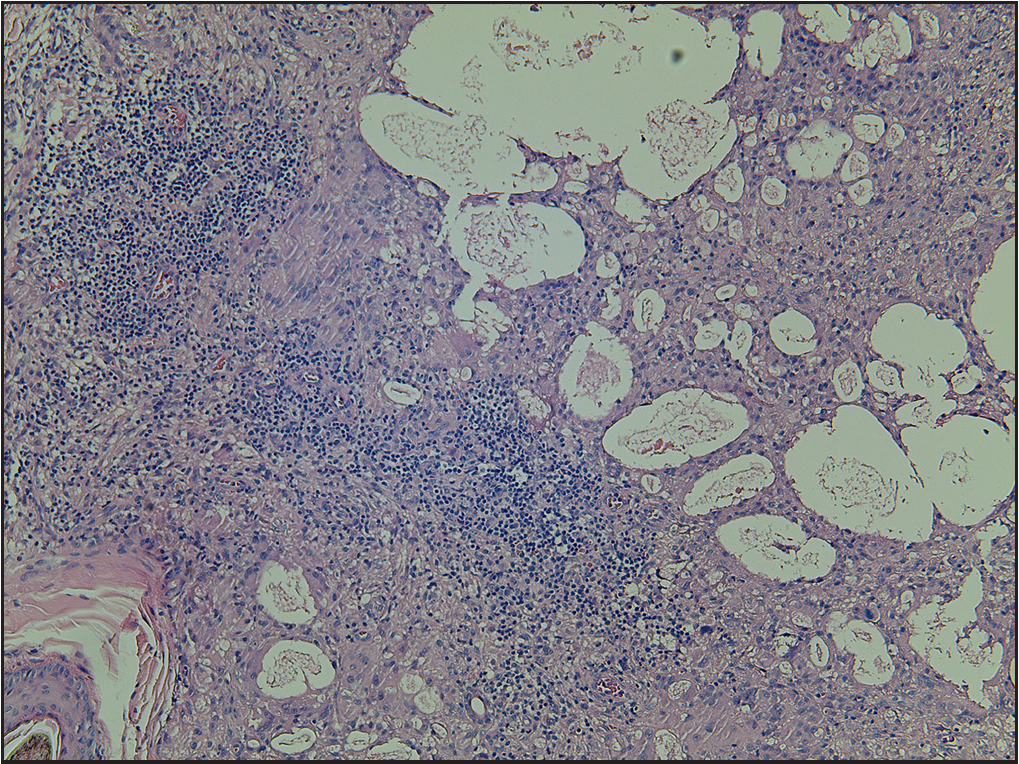
- Nodular masses were composed of predominantly lymphocytes and histiocytes in the superficial and mid dermis (H&E, 100x)
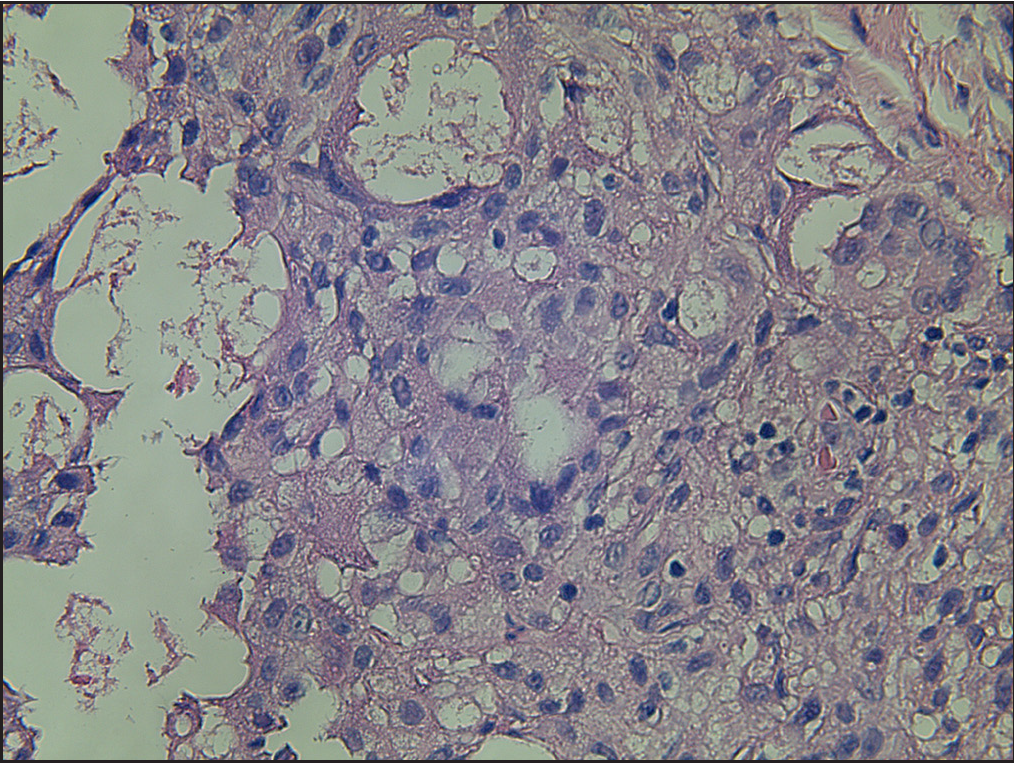
- Multinucleated giant cells and keratotic material were also present (H&E, 400x)
Diagnosis
Steatocystoma multiplex accompanied by foreign-body granuloma.
Discussion
Steatocystoma multiplex is a rare and benign skin disorder typically arising during adolescence or early adulthood. Despite the lack of a well-defined aetiology and pathogenesis, studies have demonstrated that mutations in the KRT17 gene are prevalent in many steatocystoma multiplex patients.1 Steatocystoma multiplex lesions tend to occur in areas of the body that are rich in sebaceous glands, with the most common locations being the trunk, axillae, extremities, face and scalp, and rarely the genitals and breasts.2 However, there have been a few reports of lesions that are strictly confined to the scalp. Steatocystoma multiplex is typified by the presence of multiple small, skin-coloured or yellowish cutaneous cysts that are generally asymptomatic. Nonetheless, its clinical presentation can often imitate other frequently encountered dermatological conditions such as acne vulgaris, vellus cysts, and epidermoid or dermoid cysts.2
We report a case of steatocystoma multiplex exclusively localized on the scalp of a 68-year-old woman. Sina et al. described a case of steatocystoma multiplex, which manifested as foreign body granulomas.3 The author proposed that a foreign body granuloma could be formed if the cysts were ruptured spontaneously or by trauma. Presently, various modalities such as CO2 laser, surgical excision, cryotherapy and isotretinoin have been employed to treat steatocystoma multiplex.2 However, counselling is often advised in cases where the lesions are located on the scalp and face since potential treatments may result in scarring. When informed about the benign nature of these lesions, our patient declined further treatment and is presently undergoing regular follow-ups.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Mutation analysis of the KRT17 gene in steatocystoma multiplex and a brief literature review. Clin Exp Dermatol. 2020;45:132-34.
- [CrossRef] [PubMed] [Google Scholar]
- Numerous asymptomatic dermal cysts: diagnosis and treatment of steatocystoma multiplex. Can Fam Physician. 2018;64:892-99.
- [PubMed] [PubMed Central] [Google Scholar]
- Steatocystoma multiplex manifesting as a foreign body granuloma. Cutis. 1984;33:401-2.
- [PubMed] [Google Scholar]





