Translate this page into:
A prospective study of the epidemiological and clinical patterns of recurrent dermatophytosis at a tertiary care hospital in India
2 Department of Microbiology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
3 Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Sunil Dogra
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 014
India
| How to cite this article: Pathania S, Rudramurthy SM, Narang T, Saikia UN, Dogra S. A prospective study of the epidemiological and clinical patterns of recurrent dermatophytosis at a tertiary care hospital in India. Indian J Dermatol Venereol Leprol 2018;84:678-684 |
Abstract
Background: Recurrent and clinically unresponsive dermatophytosis is being increasingly encountered in our country. It runs a protracted course with exacerbations and remissions. However, there is little information regarding the extent of the problem and the characteristics of recurrent dermatophytosis in published literature.
Aims: We sought to determine the prevalence, risk factors and clinical patterns of recurrent dermatophytosis in our institution. We also investigated the causative dermatophyte species and antifungal susceptibility patterns in these species.
Methods: One hundred and fifty patients with recurrent dermatophytosis attending the outpatient department of the Postgraduate Institute of Medical Education and Research, Chandigarh, India were enrolled in the study conducted from January 2015 to December 2015. A detailed history was obtained in all patients, who were then subjected to a clinical examination and investigations including a wet preparation for direct microscopic examination, fungal culture and antifungal susceptibility tests.
Results: Recurrent dermatophytosis was seen in 9.3% of all patients with dermatophytosis in our study. Trichophyton mentagrophytes was the most common species identified (36 patients, 40%) samples followed by T. rubrum (29 patients, 32.2%). In-vitro antifungal susceptibility testing showed that the range of minimum inhibitory concentrations (MIC) on was lowest for itraconazole (0.015–1), followed by terbinafine (0.015–16), fluconazole (0.03–32) and griseofulvin (0.5–128) in increasing order.
Limitation: A limitation of this study was the absence of a suitable control group (eg. patients with first episode of typical tinea).
Conclusion: Recurrence of dermatophytosis was not explainable on the basis of a high (MIC) alone. Misuse of topical corticosteroids, a high number of familial contacts, poor compliance to treatment over periods of years, and various host factors, seem to have all contributed to this outbreak of dermatophytosis in India.
Introduction
Dermatophytosis is a common superficial mycosis causing significant cutaneous morbidity. Itching is severe, and disabling lesions on the genital and other areas cause social embarrassment and impair quality of life.[1] The rising prevalence of dermatophytosis has been attributed to many factors including tropical climate, overcrowding, urbanization, shared accommodation such as living in hostels, the use of occlusive footwear, tight-fitting clothes, community showers and sports activity.[2]
There is no standard definition for the term “recurrent dermatophytosis.” It has been loosely referred to as dermatophytosis that runs a protracted course with episodes of exacerbations and remissions.[3] These patients are a potential source of infection to their family members and others closely associated with them. Various mechanisms contributing to chronicity and recurrences have been proposed but the exact reasons have not been elucidated.[4] Despite the increasing incidence of recurrent dermatophytosis, information on the extent of the burden in our country is scarce.[4]
Objectives
The study was designed to determine the prevalence, risk factors, clinical patterns, pathogen profile and its antifungal susceptibility patterns associated with recurrent dermatophytosis at our institution.
Methods
This cross-sectional study was conducted at the Postgraduate Institute of Medical Education and Research, Chandigarh, India from January to December 2015. The study was approved by the Institutional Review Board. All patients with dermatophyte infections visiting the outpatient department during this period were screened. One hundred and fifty patients with recurrent dermatophytosis were recruited by consecutive sampling and informed consent was obtained. The sample size was calculated on the basis of reported studies of superficial fungal infections as there were no previous studies of recurrent dermatophytosis. For the purpose of this study, a diagnosis of “recurrent dermatophytosis” was made in patients who had at least one episode of relapse of dermatophytosis within 4 weeks of stopping antifungal drugs in the preceding 6 months as per the standard recommendations.[5] Patients with only tinea ungium, those on immunosuppressants, pregnant and lactating women were excluded.
A detailed history was taken focussing on possible risk factors for recurrent dermatophytosis such as a history of contact with pets, atopy, a family history of dermatophytosis, treatment with topical or systemic antifungals alone or in combination with corticosteroids, alcoholism, frequency of habits, type of clothes, other daily habits and familial characteristics. The area of involvement was calculated in terms of hand units. One hand unit (measured as the palm plus the volar surface of all digits) was taken as approximately equivalent to 1% of the total body surface area.
Sample for mycological study
After cleaning the infected area with 70% alcohol, samples were collected by scraping the lesion from the center to the edge, crossing the lesion margin with a sterile scalpel blade. Roofs of vesicles and bullae, if present, were clipped and included in the sample.
Sample processing
Wet-mount preparation of the samples were performed using calcofluor white (Sigma, Bengaluru, India) and 10% potassium hydroxide. Direct microscopic examination of the wet-mount was performed under a fluorescent microscope.
Specimens were also cultured on Sabouraud's dextrose agar with chloramphenicol alone and separately on Sabouraud's dextrose agar with both chloramphenicol and cycloheximide (Difco, USA), and incubated at 37 and 25°C respectively for up to 4 weeks.
Antifungal susceptibility testing
Antifungal susceptibility testing was performed as per the microbroth dilution technique of Clinical and Laboratory Standards Institute guidelines (CLSI M38-A2) with minor modifications. Fluconazole, itraconazole, terbinafine and griseofulvin antifungal agents were tested. (MIC) for the antifungals used were also interpreted according to the M38-A2 CLSI guidelines.
Histopathological examination
A punch biopsy from the lesion was performed in 42 patients under aseptic conditions and examined for the presence of hyphae within the stratum corneum and the type of inflammatory infiltrate in the dermis. Periodic acid Schiff stained specimens highlighting the fungal hyphae were also examined.
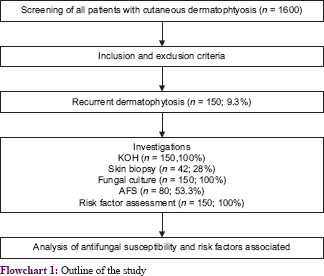
[Flowchart 1] mentions the basic study outline along with the percentage of patients involved.
Results
Out of the total 1600 patients with dermatophyte infections, 150 (9.3%) had recurrent disease. The mean age of affected patients was 32.5 years and males comprised 63% (95/150 patients). All 150 recruited patients had experienced multiple recurrences (range 3-10) usually within a few days to 4 weeks of stopping the antifungal treatment.
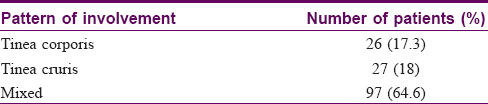
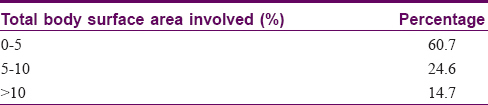
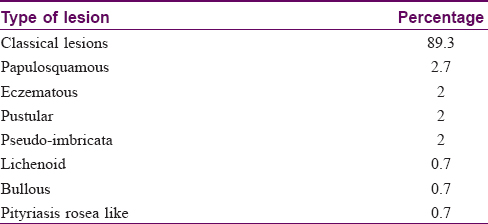
An itching or burning sensation was the most common symptom. The symptoms had been present for more than a year in 57 (38%) patients, from 6 and 12 months in 38 (25%) and for less than 6 months in 55 (37%) patients. Multiple sites (tinea corporis, cruris, faciei, pedis and manuum) were involved in 97 (64.6%) patients. Tinea cruris alone was seen in 28 (18%) and tinea corporis alone in 26 (17.3%) patients [Table - 1]. One patient had lesions on the shaft of the penis. Most patients (91, 60.7%) had less than 5% body surface area involvement [Table - 2] but extensive lesions (>10% body surface area) were seen in 22 (14.7%). The lesions were inflammatory in 121 (80.6%) patients while in the remainder they were dry and noninflammatory. Annular lesions were seen in 134 (89.3%) patients. Papulosquamous, eczematous, pustular, pseudo-imbricata, lichenoid, pityriasis rosea like and bullous lesions all were also seen in a few cases each [Table - 3] and [Figure - 1], [Figure - 2], [Figure - 3], [Figure - 4].
 |
| Figure 1: A case of tinea faciei: pseudoimbricata type |
 |
| Figure 2: A case of tinea corporis: pityriasis rosea type |
 |
| Figure 3: A case of tinea corporis: bullous type |
 |
| Figure 4: A case of tinea on trunk involving the shaft of penis |
A history of atopy was uncommon (29 patients; 19.3%) as was a family history of atopy (14 patients; 9.3%). Few patients (23 patients, 15.3%) kept pets.
Over half of the patients (66/150; 53.2%) (80/150;53.3%) had used topical corticosteroids either alone or in combination with antibacterial and antifungal agents (eg. Panderm®, Quadriderm®, Candid-B®, Betnovate®, Ringuard® and Itchguard®) for varying periods of time before presentation. A majority of the patients (106/150; 70.6%) had received systemic antifungals such as terbinafine, itraconazole and griseofulvin for durations ranging from 3 to 4 months. Most of these patients (96/106, 90.5%) had completed the full course of antifungal, while the rest stopped the treatment immediately after clearance of lesions. In most cases the lesions cleared completely but reappeared within a few days to 2 weeks of stopping treatment. The lesions reappeared within 3 to 4 days of stopping the treatment in 56 (37.3%) patients. The lesions usually recurred at the same site starting from the borders (105, 70%), but in the remaining cases the new lesions appeared in other areas as well.
Family members of 108 (72%) patients had dermatophytosis, the spouse being frequently (87/108, 80.5%) affected. Two or more family members (including siblings and parents) were involved in 48 (44.4%) cases.
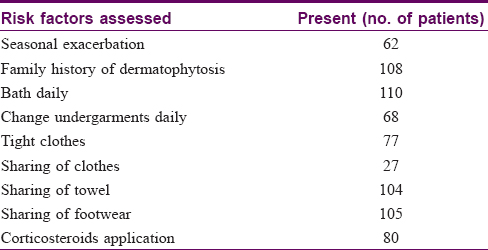
Although most (110/150, 73%) patients bathed daily, some (30, 20%) bathed on alternate days. Ten (7%) of the patients admitted to having infrequent baths (twiceweekly or less) especially in winters. Less than half (68, 45.3%) the patients changed their undergarments daily. Sharing footwear among family members was common (105 patients, 70%), as also was sharing of towels (104, 69%). However, only 27 (18%) patients admitted to sharing clothes. All household clothes were washed together in the majority of patients, but in 22 (15%) patients the clothes were washed separately. Tight clothes such as jeans were worn by over half (76, 51%) the patients and these were infrequently washed - often only once or twice in a month [Table - 4].
Direct microscopic examination of wet-mount specimens was positive for septate hyphae in 148 (98.7%) patients [Figure - 5]. Dermatophytes grew in cultures from samples collected from 90 (60%) patients. T. mentagrophytes was the most common species isolated in 36 (40%), followed by T. rubrum in 29 (32.2%) and T. interdigitale in 10 (11.1%) [Figure - 6] and [Figure - 7]. Other dermatophytes were infrequently isolated and included M. gypseum in 4 (4.4%) cases, T. tonsurans in 3 (3.3%), M. canis in 2 (2.2%) and T. schoenleinii and T. violaceum in 1 case each.
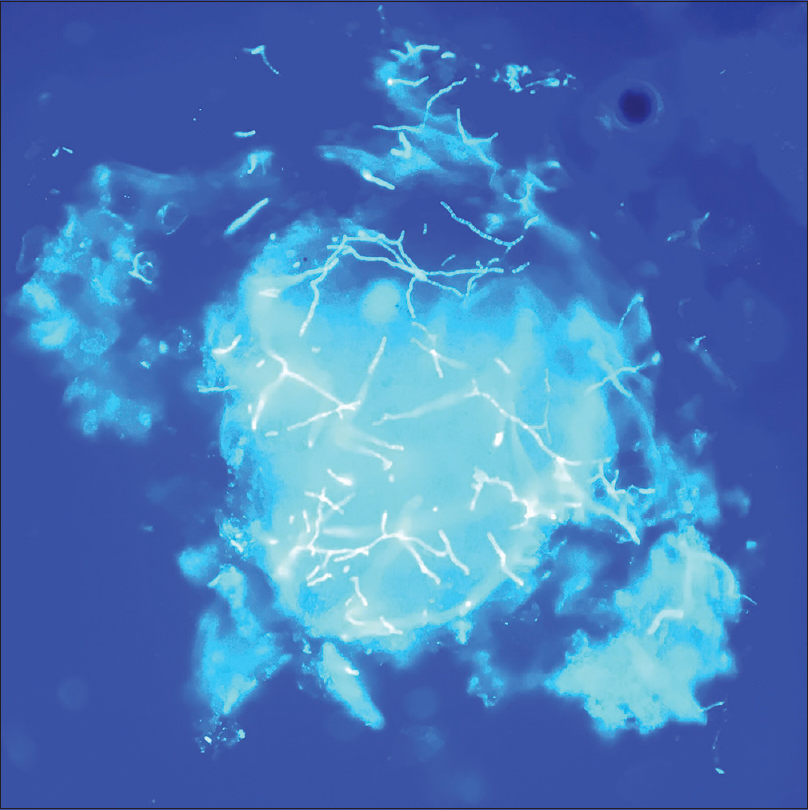 |
| Figure 5: Thin septate hyphae of dermatophytes on calcofluor wet-mount examined under fluorescent microscope |
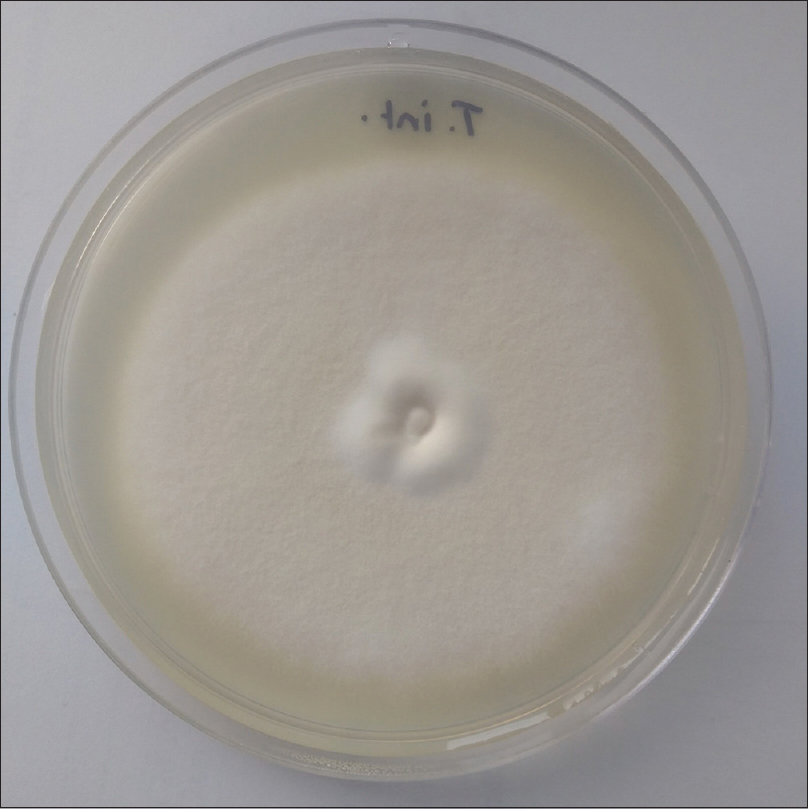 |
| Figure 6: Yellowish white colony of Trichophyton interdigitale on Sabourauds dextrose agar after one week incubation |
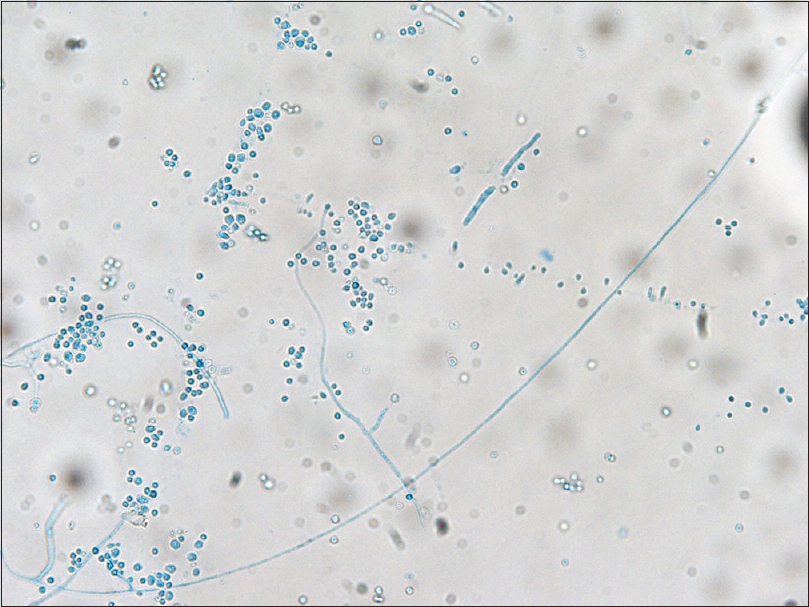 |
| Figure 7: Slide culture of Trichophyton interdigitale predominantly showing round-to-oval microconidia arranged in grape-like clusters (lactophenol cotton blue mount; 40x) |
Histopathological examination of skin lesions performed in 42 patients revealed epidermal changes including hyperkeratosis in 9 (21.4%) and acanthosis in 18 (42.8%) biopsy samples. Fungal hyphae were detected in 8 (19%) specimens on hematoxylin and eosin stain, and in 13 (30.9%) with periodic acid Schiff stain. A perivascular lymphocytic infiltrate was the predominant dermal change noted.
Antifungal susceptibility testing: In-vitro antifungal susceptibility testing with fluconazole, itraconazole, terbinafine and griseofulvin was performed on 80 isolates of Trichophyton species. MIC-50 and MIC-90 values were calculated for species with 10 or more isolates (i.e. T. mentagrophytes, T. rubrum and T. interdigitale) [Table - 5].
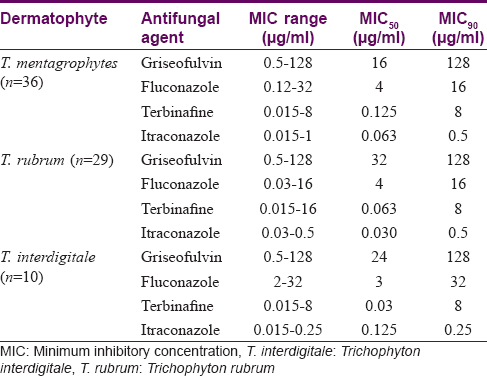
High MIC values were seen in 14 isolates for terbinafine and in 11 isolates each for fluconazole and griseofulvin but none of the isolates had a high MIC for itraconazole. High MICvalues for both griseofulvin and terbinafine were noted in 3 isolates.
Discussion
Dermatophyte infections are widespread and cause significant distress to the patients socially, emotionally and financially. Recurrent dermatophytosis is fast emerging as a challenge for dermatologists in India.[4] Recurrent dermatophytosis constituted 9.3% of all patients with presenting with dermatophytosis in our study mostly afflicting young adult males. Since the conclusion of this study in 2015, we have observed a many fold increase in recurrent dermatophytosis.
We observed frequent sharing of towel and footwear and clothes in our patients. This could contribute to the spread of infection. Objects such as clothing, bedsheets and towel harbor the fungal pathogens and are capable of transmitting the disease among family members. In addition, fungal spores remain viable for months in household dust leading to recurrent episodes of clinical disease.[6],[7] Asymptomatic carriers among family members may also be another cause for recurrence. A third of our patients wore tight clothes such jeans, and woolen undergarments in winters, which were often unwashed for weeks creating a damp environment favorable for proliferation of dermatophytes.
Topical application of corticosteroids was freqeuntly seen in our patients. Corticosteroid-containing topical applications suppress inflammation and improve signs and symptoms of tinea initially. However dermatophytes flourish leading to subsequent flare of the disease.[8] Treatment prescribed by general practitioners and quacks in India for tinea is usually polypharmacy with corticosteroid combinations and subtherapeutic doses of antifungals. With the implementation of the policy of prescribing generic medicines in India, chemists and pharmacists often dispense any brand of antifungal drug regardless of physician prescription. In recent years a large number pharmaceutical houses in India have started manufacturing antifungal drugs such as itraconazole in 200 and 400 mg capsules and powders, the quality, bioavailability and rationale of which are questionable. Irrational use of topical and systemic antifungal medications either alone or in combination with easily available over-the-counter steroid or antibacterial agents are contributing to the emergence of recurrent dermatophytosis. Concentrations of itraconazole peak at 2 weeks in the stratum corneum and effective levels are maintained for up to 8 weeks after the completion of a course.[9] Therefore, rapid clinical recurrences are unlikely to be due to reinfection but rather due to incomplete mycological response to antifungal drugs administered owing to emerging virulent strains of dermatophytes.
Direct microscopy of samples was positive in 148 (98.7%) cases which is much higher than the reported positivity rates (64–79%) in other studies.[10],[11] This could be due to the use of calcofluor white with fluorescent microscopy which is more sensitive than direct microscopy with potassium hydroxide alone. A higher fungal load in these recurrent cases may also be responsible for the higher positivity. The higher culture positivity rate of 60% in our study as compared to 37.5% to 55.1% reported in other studies from the same geographical region[10],[11],[12] may also be due to the higher fungal load in recurrent cases as well as due to better collection, transportation and processing of samples.
T. mentagrophytes was the most commonly isolated organism. This has been the most frequently isolated organism in other reports from India,[6],[7],[8],[9],[10],[11],[12],[13],[14],[15] although in some studies of tinea corporis and cruris, T. rubrum h as been more frequently isolated.[16] The taxonomy of dermatophytes is evolving with increased use of molecular techniques and T. mentagrophytes and T. rubrum are now considered as a species complex with many species defined within each species.[17]
Itraconazole was the most effective antifungal agent against T. mentagrophytes (MIC-90 of 0.5 μg/ml), T. rubrum (MIC-90 of 0.03 μg/ml) and T. interdigitale (MIC-90 of 0.125 μg/ml). High MIC for terbinafine has been reported by Lakshmanan et al. from Iran,[16] and primary resistance to terbinafine due to mutation in the squalene epoxidase gene has been reported in T. rubrum.[18] We noted high MIC (>2 μg/ml) for terbinafine in one T. interdigitale, four T. mentagrophytes, three T. rubrum and isolates.
Fluconazole was moderately effective according to the in-vitro susceptibility results and griesofulvin was the least active agent among all the species tested with MIC-50 of 16, 32 and 32 μg/ml for T. mentagrophytes, T. rubrum and T. interdigitale, respectively. Similar findings have been reported in earlier studies.[19],[20],[21],[22] The MIC ranges for various antifungal drugs were much lower in our study as compared to those in a recent study by Mahajan et al. from Varanasi.[15]
Neither MIC-50 nor MIC-90 can categorize the isolates as resistant or sensitive as they only indicate the MIC of 50% or 90% of the tested isolates. This information is used to map the susceptibility pattern of the circulating strains in a given setting (Institute, region, or country etc.). For an isolate to be labeled as resistant to terbinafine, itraconazole or griseofulvin a MIC of 4 mg/L or more, whereas for fluconazole more than 32 mg/L is considered resistant.
Our results indicate that increase in MIC is not the only factor responsible for recurrence. Relapse after adequate treatment of onychomycosis is common,[23] but not well recognized in other forms of dermatophytosis. Most of the strains are not drug resistant. Although recurrences may also be due to reinfection from family members or the environment, it is more likely that the duration of antifungal therapy given may be inadequate. Most of our patients had stopped topical treatment as soon as they got partial relief. In view of the expected high fungal load, extending the therapy for 2–3 weeks after the clinical cure may be necessary.
The main limitation of the present study is the lack of a patient group who had only first episode of typical dermatophytosis for compare pathogens isolated and antifungal drug susceptibility. Also there was no follow-up of the recruited patients to correlate the results of antifungal susceptibility and clinical outcome. We also did not study the immunological profile of these patients which could provide further information regarding this problem.
Conclusion
In our study of recurrent dermatophytosis, we observed that a high incidence of intrafamilial tinea infections, misuse of corticosteroids-containing topical antifungal preparations, poor compliance to treatment and poor personal hygeine were associated with recurrences and poor responses to treatment. A high MIC of antifungal drugs alone could not explain the frequently noted recurrence phenomenon in dermatophytes infection. It is likely that dermatophyte organisms are becoming more virulent with a gradual increase in the minimum inhibitory concentration of commonly used antifungal drugs as a result of various host, environmental and treatment factors posing a great emerging health hazard to the community.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Degreef H. Clinical forms of dermatophytosis (ringworm infection). Mycopathologia 2008;166:257-65.
[Google Scholar]
|
| 2. |
Weitzman I, Summerbell RC. The dermatophytes. Clin Microbiol Rev 1995;8:240-59.
[Google Scholar]
|
| 3. |
Sentamilselvi G, Kamalam A, Ajithadas K, Janaki C, Thambiah AS. Scenario of chronic dermatophytosis: An Indian study. Mycopathologia 1997;140:129-35.
[Google Scholar]
|
| 4. |
Dogra S, Uprety S. The menace of chronic and recurrent dermatophytosis in India: Is the problem deeper than we perceive? Indian Dermatol Online J 2016;7:73-6.
[Google Scholar]
|
| 5. |
Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J 2016;7:77-86.
[Google Scholar]
|
| 6. |
Bhatia VK, Sharma PC. Epidemiological studies on dermatophytosis in human patients in Himachal Pradesh, India. Springerplus 2014;3:134.
[Google Scholar]
|
| 7. |
Havlickova B, Czaika VA, Friedrich M. Epidemiological trends in skin mycoses worldwide. Mycoses 2008;51 Suppl 4:2-15.
[Google Scholar]
|
| 8. |
de Freitas RS, Neves PS, Charbel CE, Criado PR, Nunes RS, Santos-Filho AM, et al. Investigation of superficial mycosis in cutaneous allergy patients using topical or systemic corticosteroids. Int J Dermatol 2017;56:e194-8.
[Google Scholar]
|
| 9. |
Morimoto K, Tanuma H, Kikuchi I, Kusunoki T, Kawana S. Pharmacokinetic investigation of oral itraconazole in stratum corneum level of tinea pedis. Mycoses 2004;47:104-14.
[Google Scholar]
|
| 10. |
Hanumanthappa H, Sarojini K, Shilpashree P, Muddapur SB. Clinicomycological study of 150 cases of dermatophytosis in a tertiary care hospital in South India. Indian J Dermatol 2012;57:322-3.
[Google Scholar]
|
| 11. |
Bindu V, Pavithran K. Clinico-mycological study of dermatophytosis in Calicut. Indian J Dermatol Venereol Leprol 2002;68:259-61.
[Google Scholar]
|
| 12. |
Vyas A, Pathan N, Sharma R, Vyas L. A clinicomycological study of cutaneous mycoses in Sawai man singh hospital of Jaipur, North India. Ann Med Health Sci Res 2013;3:593-7.
[Google Scholar]
|
| 13. |
Bhatia VK, Sharma PC. Determination of minimum inhibitory concentrations of itraconazole, terbinafine and ketoconazole against dermatophyte species by broth microdilution method. Indian J Med Microbiol 2015;33:533-7.
[Google Scholar]
|
| 14. |
Adimi P, Hashemi SJ, Mahmoudi M, Mirhendi H, Shidfar MR, Emmami M, et al. In vitro activity of 10 antifungal agents against 320 dermatophyte strains using microdilution method in Tehran. Iran J Pharm Res 2013;12:537-45.
[Google Scholar]
|
| 15. |
Mahajan S, Tilak R, Kaushal SK, Mishra RN, Pandey SS. Clinico-mycological study of dermatophytic infections and their sensitivity to antifungal drugs in a tertiary care center. Indian J Dermatol Venereol Leprol 2017;83:436-40.
[Google Scholar]
|
| 16. |
Lakshmanan A, Ganeshkumar P, Mohan SR, Hemamalini M, Madhavan R. Epidemiological and clinical pattern of dermatomycoses in rural India. Indian J Med Microbiol 2015;33 Suppl: 134-6.
[Google Scholar]
|
| 17. |
Jensen RH, Arendrup MC. Molecular diagnosis of dermatophyte infections. Curr Opin Infect Dis 2012;25:126-34.
[Google Scholar]
|
| 18. |
Osborne CS, Leitner I, Favre B, Ryder NS. Amino acid substitution in Trichophyton rubrum squalene epoxidase associated with resistance to terbinafine. Antimicrob Agents Chemother 2005;49:2840-4.
[Google Scholar]
|
| 19. |
Yenişehirli G, Tunçoğlu E, Yenişehirli A, Bulut Y.In vitro activities of antifungal drugs against dermatophytes isolated in Tokat, Turkey. Int J Dermatol 2013;52:1557-60.
[Google Scholar]
|
| 20. |
Gupta AK, Kohli Y.In vitro susceptibility testing of ciclopirox, terbinafine, ketoconazole and itraconazole against dermatophytes and nondermatophytes, and in vitro evaluation of combination antifungal activity. Br J Dermatol 2003;149:296-305.
[Google Scholar]
|
| 21. |
Afshari MA, Shams-Ghahfarokhi M, Razzaghi-Abyaneh M. Antifungal susceptibility and virulence factors of clinically isolated dermatophytes in Tehran, Iran. Iran J Microbiol 2016;8:36-46.
[Google Scholar]
|
| 22. |
Silva LB, de Oliveira DB, da Silva BV, de Souza RA, da Silva PR, Ferreira-Paim K, et al. Identification and antifungal susceptibility of fungi isolated from dermatomycoses. J Eur Acad Dermatol Venereol 2014;28:633-40.
[Google Scholar]
|
| 23. |
Gupta AK, Elewski BE, Rosen T, Caldwell B, Pariser DM, Kircik LH, et al. Onychomycosis: Strategies to minimize recurrence. J Drugs Dermatol 2016;15:279-82.
[Google Scholar]
|
Fulltext Views
10,202
PDF downloads
3,190





