Translate this page into:
A rare case of aggressive systemic mastocytosis manifesting with bullous lesions in a neonate
Correspondence Address:
Biju Vasudevan
Department of Dermatology, Base Hospital, Lucknow, Uttar Pradesh
India
| How to cite this article: Sinha A, Vasudevan B, Sharma N, Verma R, Aneesh K P. A rare case of aggressive systemic mastocytosis manifesting with bullous lesions in a neonate. Indian J Dermatol Venereol Leprol 2020;86:706-709 |
Sir,
Mastocytosis refers to a group of disorders characterized by excessive mast cell accumulation in the skin and other tissues.[1] The most recent classification of mastocytosis by the WHO in 2016 features mainly three types: cutaneous, systemic and mast cell sarcoma. Systemic mastocytosis involves extracutaneous organs with or without skin involvement and includes the following forms: indolent systemic mastocytosis, smoldering systemic mastocytosis, mastocytosis with associated clonal hematological non-mast cell disease, aggressive systemic mastocytosis and mast cell leukemia.[2]
Our patient was a male neonate who was the first-born child (by full-term normal vaginal delivery) of a nonconsanguineous marriage to a healthy mother with an uneventful antenatal and perinatal history. At birth, the patient was noticed to have diffuse skin eruptions with bullous lesions all over the body. He was not taking breastfeeds and was placed on orogastric tube feed. The neonate was referred to our center on the 2nd day of birth with clinical differentials of epidermolysis bullosa, bullous mastocytosis and porphyria.
Examination at our center revealed diffuse erythema and thickening of skin over the entire body, along with multiple overlying hemorrhagic bullae, some of which were intact and some had eroded to reveal raw bleeding areas [Figure - 1]. There were patchy areas on the trunk and lower limbs with a diffuse leathery appearance [Figure - 2]. There was clearly evident diffuse thickening and infiltration of facial skin with accentuated skin markings [Figure - 3]. The neonate's face had a wizened old man look. Palms and soles were involved. Darier's sign was positive in the form of bullae developing over areas where any form of even mild friction was present [Figure - 4]. The abdomen was mildly distended.
 |
| Figure 1: Multiple blisters on the back of the neonate |
 |
| Figure 2: Leathery plaques on limbs |
 |
| Figure 3: Accentuated skin markings and folds on face |
 |
| Figure 4: Darier's sign visible as blister at site of tubing |
Skin biopsy revealed subepidermal bullae with prominent monocytic infiltration of the entire dermis by mast cells and metachromatic granules were seen in these cells after staining with toluidine blue, confirming the diagnosis of bullous mastocytosis [Figure - 5], [Figure - 6], [Figure - 7]. There was hepatosplenomegaly evident on ultrasonography and marked anemia. Total leukocyte count was 22,000/mm[3] and platelets were low (96,000/mm[3]). Serum bilirubin was 15mg/dL, aspartate transaminase was 114 U/L and alanine transaminase was 68 U/L on day 2. Serum tryptase was heavily raised, having a value of 200 μg/L (normal range: 2–14 μg/L) and serum histamine was also raised (4.53 μg/L). TORCH screen and screening for other infections were negative. A diagnosis of aggressive systemic mastocytosis was made based on skin biopsy findings, very high tryptase and histamine levels, hepatosplenomegaly and derangement of peripheral blood counts.
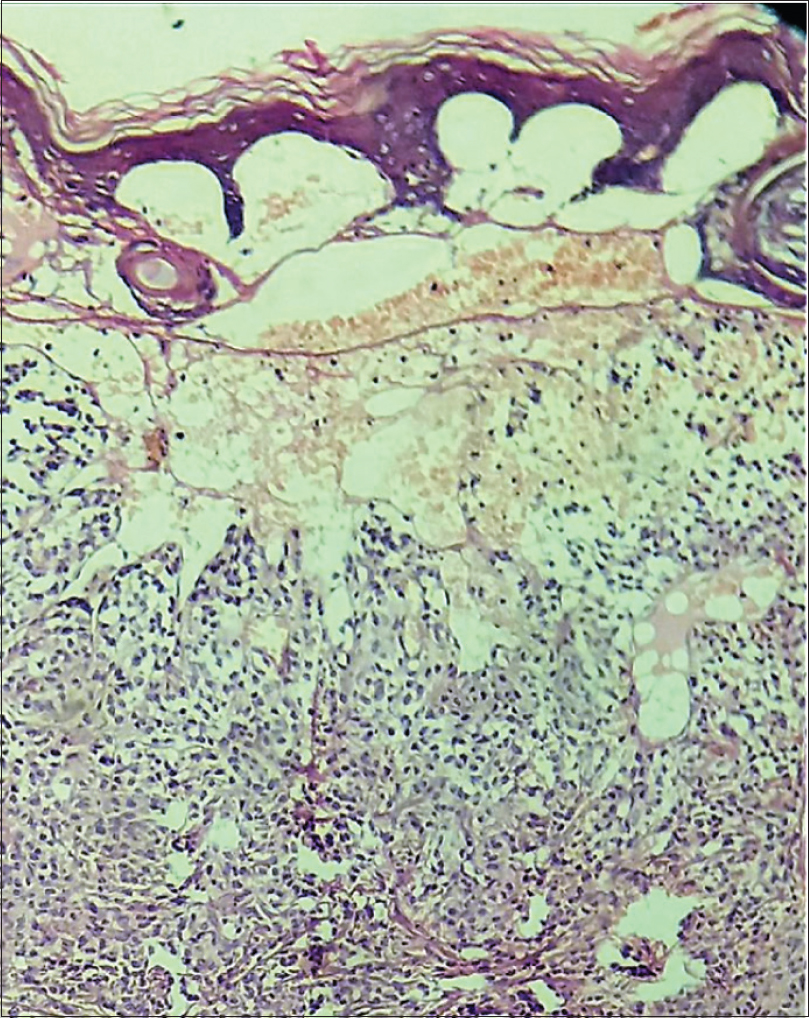 |
| Figure 5: Subepidermal bullae with extensive monomorphic basophilic infiltrate in the entire dermis (H and E, ×100) |
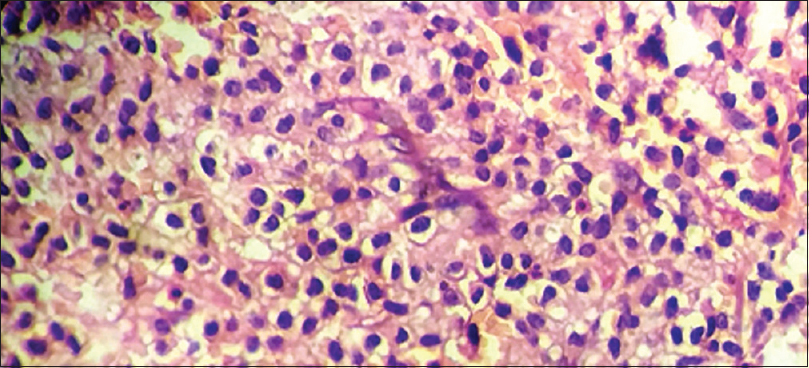 |
| Figure 6: Extensive mast cell infiltrate (H and E, × 400) |
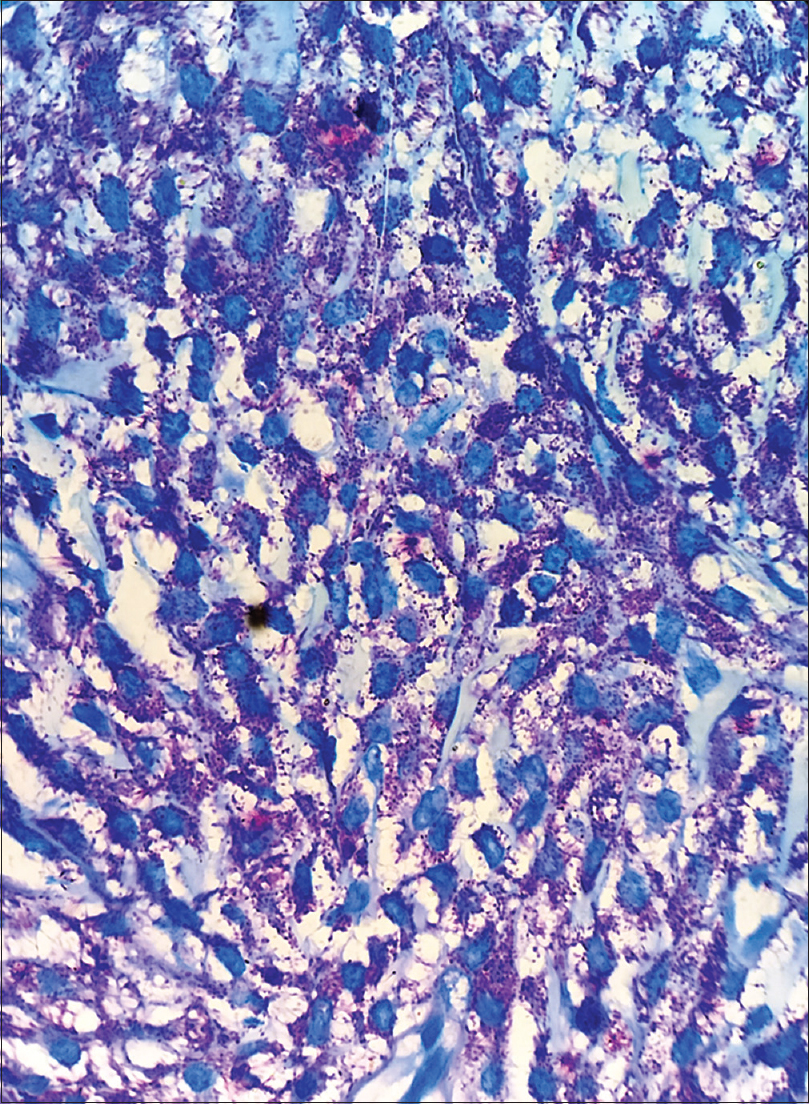 |
| Figure 7: Mast cells with granules (toluidine blue stain, ×400) |
The patient was initially treated with injection pheniramine maleate, injection dexamethasone, injection cefotaxime and injection gentamycin along with adequate hydration. All precautions to prevent mast cell degranulation and ensuring minimal trauma during handling were undertaken. The skin condition seemed to improve over 3 days, with reduction in blistering. However, on the 5th day patient suddenly developed multiple hemorrhagic bullae and extensive crusting all over the body [Figure - 8] and started having profuse watery diarrhea with sudden onset fever, tachycardia, tachypnoea and hypotension. There was worsening anemia (Hb 6g/dL), thrombocytopenia (24,000/μL), with further deterioration of liver function tests (bilirubin-19.7 mg/dL, aspartate transaminase-160 U/L, alanine transaminase-110 U/L) and deranged coagulation parameters with international normalized ratio (INR-) 3.28. The baby was put on ventilator support and aggressively managed with injection noradrenaline, injection dopamine, injection dexamethasone, injection pheniramine along with injections vancomycin and meropenem with a diagnosis of septicemia. However, the child's condition continued to deteriorate and he died on the 7th day after birth.
 |
| Figure 8: Worsening of conditioning of neonate with crusted extensive lesions on body |
Biopsy of the liver, bone marrow and spleen postmortem revealed infiltration with mast cells and the cause of death was attributed to massive mast cell degranulation causing cardiovascular collapse complicated by infection-induced sepsis. C-kit mutation analysis could not be carried out as the parents had decided against doing any further investigations.
Mastocytoses are a heterogenous group of disorders that may be difficult to diagnose and treat. The disease is caused by a gain-of-function mutation in proto-oncogene, KIT (CD117), a receptor tyrosine kinase responsible for mast cell growth, differentiation and survival.[3]
Systemic mastocytosis is rarely seen in children, while aggressive systemic mastocytosis, characterized by heavy mast cell accumulation in various organs like the skeletal system, bone marrow, gastrointestinal tract and spleen, is even rarer. The condition has been reported previously in a very few neonates,[4],[5],[6] with a poor prognosis.
According to consensus criteria, the diagnosis of aggressive systemic mastocytosis requires the fulfilment of systemic mastocytosis criteria: One major criterion: (i) presence of multifocal dense infiltrates of >15 mast cells aggregating in bone marrow or other extracutaneous organs plus one minor criterion, or three minor criteria by themselves including:(i) mast-cell infiltrates in bone marrow or other extracutaneous organs with >25% spindle-shaped cells, (ii) c-KIT D816V mutation, (iii) expression of CD2 and/or CD25 on CD117+ mast cells, (iv) serum tryptase levels >20 ng mL plus one or more “C-findings”(cytopenia, malabsorption, osteolysis, liver impairment and ascites).[7] Our patient had the major criteria, two minor criteria and C findings.
Aggressive systemic mastocytosis is a difficult to treat condition and treatment options include antihistaminics, H2 antagonists, disodium cromoglygate, corticosteroids, psoralen ultraviolet A, interferon alpha-2b and tyrosine kinase inhibitors. There is limited information in the literature to guide treatment of patients such as ours, with multisystem infiltration of mast cells causing multiple organ failure. Tyrosine kinase inhibitors have been shown to cause mast cell apoptosis, but their use in infants or neonates has been rarely reported.[8] Antibiotics are indicated in cases with features of sepsis. This case highlights the rapidly progressing course of aggressive systemic mastocytosis in a neonate and the need to develop aggressive treatment options to improve prognosis in patients, especially of this age group, which is otherwise very poor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Verma R, Vasudevan B, Vijendran P, Mitra D. A rare case of bullous mastocytosis in a child associated with bathing trunk nevus. Int J Dermatol 2014;53:761-3.
[Google Scholar]
|
| 2. |
Arber DA, OraziA, Hasserjian R, Thiele J, Borowitz MJ, LeBeau MM, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 2016;127:2391-405.
[Google Scholar]
|
| 3. |
Jenkinson HA, Lundgren AD, Carter MC, DiazL Z, Levy ML. Management of a neonate with diffuse cutaneous mastocytosis: Case report and literature review. Pediatr Dermatol 2019;36:486-9.
[Google Scholar]
|
| 4. |
Huang A, Fiadorchanka N, Brar K, Balderacchi JL, Glick SA. In utero presentation of aggressive systemic mastocytosis in a neonate. Br J Dermatol 2017;177:1439-41.
[Google Scholar]
|
| 5. |
5. Chaudhary N, Shapiro N, Bhutada A, Rastogi S. c-KIT-positive fatal diffuse cutaneous mastocytosis with systemic manifestations in a neonate. J Pediatr Hematol Oncol 2019;41:e338-40.
[Google Scholar]
|
| 6. |
Walker T, von Komorowski G, Scheurlen W, Dorn-Beineke A, Back W, Bayerl C. Neonatal mastocytosis with pachydermic bullous skin without c-Kit 816 mutation. Dermatology 2006;212:70-2.
[Google Scholar]
|
| 7. |
Valent P, Akin C, Metcalfe DD. Mastocytosis: 2016 updated WHO classification and novel emerging treatment concepts. Blood 2017;129:1420-7.
[Google Scholar]
|
| 8. |
Droogendijk HJ, Kluin-Nelemans JC, van Doormaal JJ. Imatinib mesylate in the treatment of systemic mastocytosis. A phase II trial. Cancer 2006;107:345-51.
[Google Scholar]
|
Fulltext Views
3,413
PDF downloads
1,438





