Translate this page into:
A rare case of inverted follicular keratosis in an elderly male: Dermoscopic and histopathological overview with therapeutic response to imiquimod
Corresponding author: Dr. Arunima Ray, Department of DVL, IMS and SUM Hospital, Siksha O Anusundhan University, Bhubaneshwar, Odisha, India. arunima.roma@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ray A, Panda M, Samant S, Mohanty P. A rare case of inverted follicular keratosis in an elderly male: Dermoscopic and histopathological overview with therapeutic response to imiquimod. Indian J Dermatol Venereol Leprol 2021;87:455.
Sir,
Inverted follicular keratosis is a benign tumor of the follicular infundibulum, commonly treated with surgical excision. It usually presents as a solitary lesion over the face and neck. The diagnosis is based on histopathological findings and common clinical differentials are squamous cell carcinoma, basal cell carcinoma, keratoacanthoma and warts.1
Due to its predilection for elderly patients and its site, inverted follicular keratosis clinically masquerades as a malignant growth. This makes it diagnostically noteworthy.
We are reporting this case for its rarity, dermoscopic and histopathologically aided conclusive diagnosis and the satisfactory treatment response with topical imiquimod.
A 63-year-old man presented to the dermatology outpatient department (IMS and SUM Hospital, Bhubaneswar) with a single well-defined, painless, skin-colored plaque (1 cm × 0.5 cm) over the margin of his left upper eyelid. The surface was irregular, verrucous with crusting and without any friability [Figure 1]. The plaque was slowly growing over the last three months. No other lesions were present elsewhere and the patient was not on any medications.

- Single irregular verrucous plaque (1 cm × 0.5 cm) over the upper left eyelid
There were no complaints of ocular morbidity except for local conjunctival congestion in the left eye. On slit-lamp examination, there was very mild conjunctival congestion present locally near the eyelid.
On dermoscopy (using DermLite DL3N with iPhone X), yellow-white structureless amorphous areas with central keratinous plugs, white lines, red dots (blood spots), milky red areas and hairpin vessels surrounded by a whitish halo were seen [Figure 2].
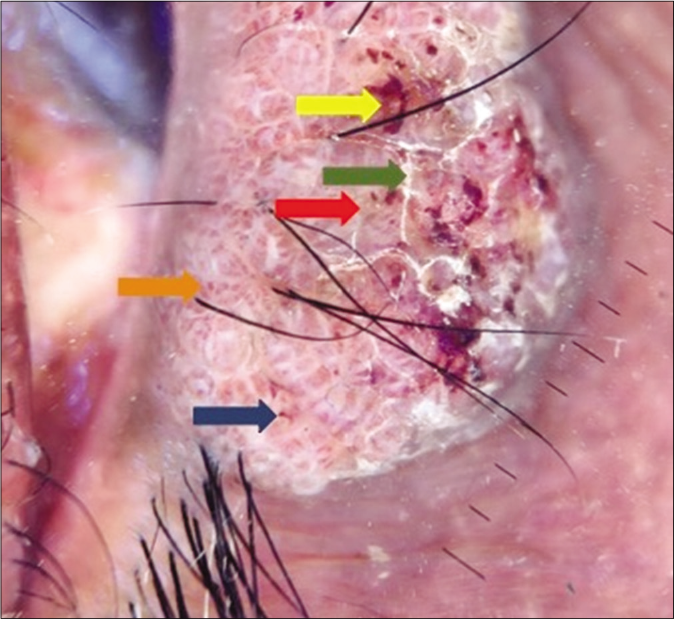
- Dermoscopy (DermLite DL3N with iPhone X attachment at 10×, polarized mode) showed linear vessels with whitish halo (blue arrow), yellow white structureless areas (red arrow), red dots (yellow arrow), white lines (green arrow) and glomerular vessels (orange arrow)
Histopathological examination revealed a stratified, squamous epithelium with hyperkeratosis, parakeratosis, foci of keratin plugging and dense inflammation with inverted papillomatosis, acanthosis and a number of squamous eddies.. There was no cellular atypia, cell nests or abnormal mitotic figures [Figures 3-5].
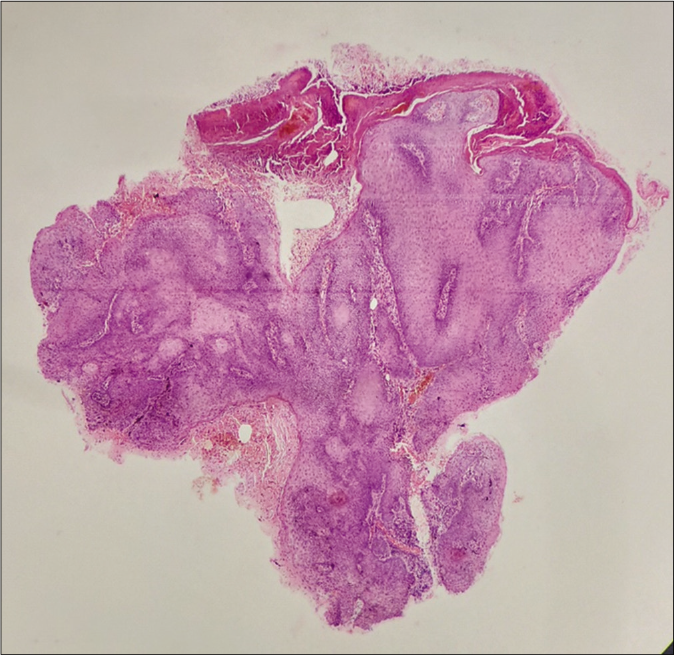
- Scanner view shows an endo-exophytic growth with features of hyperkeratosis, acanthosis and inverted papillomatosis (H and E stain, 4×)
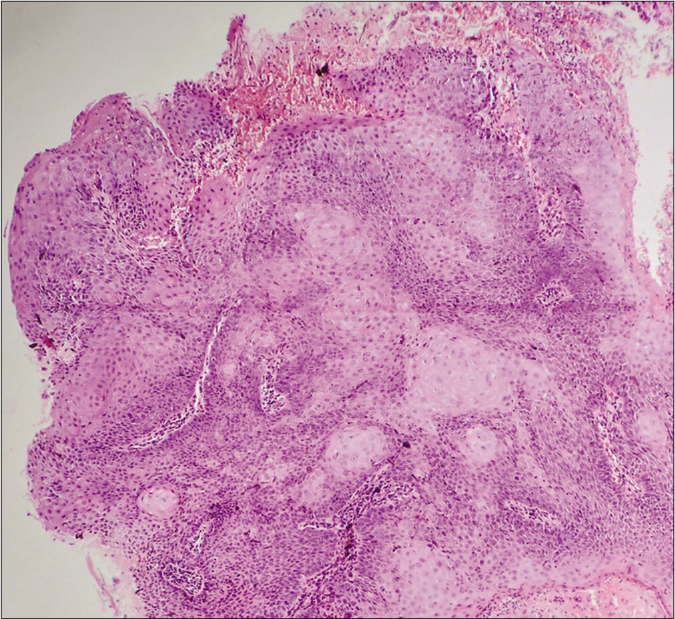
- Numerous squamous eddies are visible (H and E stain 10×)
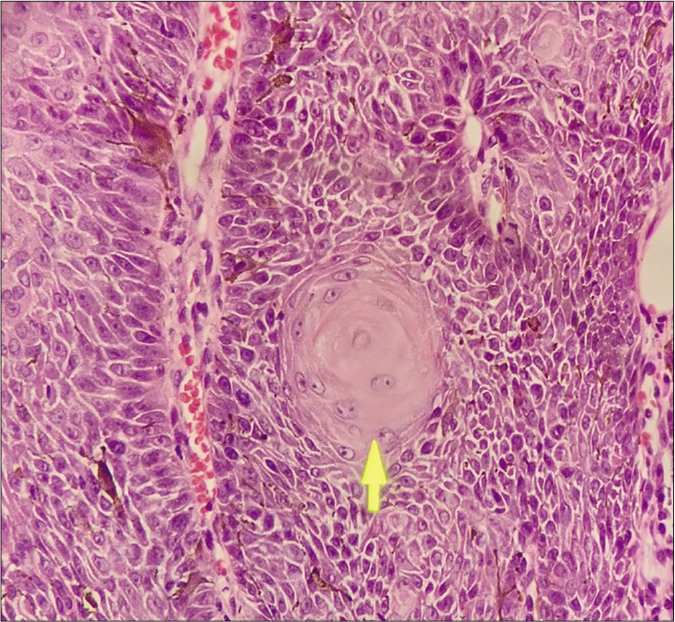
- H and E stain, 40×), a single squamous eddy is visible (yellow arrow)
The patient was advised to apply 5% imiquimod cream for three consecutive days a week for four weeks. To avoid any local irritation, strict instructions were given to apply petrolatum jelly around the plaque to avoid any spillover to the normal skin.
After two weeks of commencement of treatment, he had conjunctival congestion and watering of eyes which was treated with mild steroid (loteprednol) eyedrops in tapering doses and lubricant eye drops. Conjunctival congestion subsided within two weeks without any further complaints.
Patient continued to apply imiquimod over the next two weeks and a significant regression in the size of the plaque (more than 80%) was seen [Figure 6].

- Significant regression in plaque is seen after 4 weeks of topical imiquimod application
Inverted follicular keratosis usually presents as solitary lesion, principally in elderly men. The classical histopathological sign is squamous eddies which are tight whorls of bland appearing squamous cells which are irritated keratinocytes. It shares a pathogenic consanguinity with irritated seborrheic keratosis.
Seborrheic keratosis has a predominantly exophytic component, and inverted follicular keratosis has a downward growing component characterized by endo-exophytic growth.2 Some consider inverted follicular keratosis as a rare variant of seborrheic keratosis while some others consider it as a distinct entity.
Llambrich et al. in one of the largest dermoscopic series on inverted follicular keratosis found that 83.3% of patients showed hairpin vessels, 75% showed white structureless areas and scales, 66.6% showed keratin, and 33.3% had blood spots.3 Hairpin vessels along with white structureless areas, which is the keratoacanthoma like pattern, was seen in 58.3% of their patients. All these findings were seen in our patient also. Other dermoscopic studies on inverted follicular keratosis also show such findings.4
The exact etiopathogenesis of this entity is unknown. Association with human papillomavirus infection, seborrheic keratosis, viral warts and Cowden Syndrome has been seen.5 Surgical excision is the preferred treatment. However, due to the delicate site over the eyelid, imiquimod cream was preferred in this patient. Karadag et al. has reported successful treatment of inverted follicular keratosis with topical 5% imiquimod cream.In our patient, 5% imiquimod cream applied three times per week for four weeks produced significant regression by over 80% [Figure 6].
Imiquimod has both antitumor and antiviral activity, with antiangiogenic properties, which upregulates the endogenous antiangiogenic mediators like tissue inhibitor of matrix metalloproteinase and downregulates proangiogenic molecules like basic fibroblast growth factor and matrix metalloproteinase.
Owing to its site, morphological ambiguity and predilection for elderly, inverted follicular keratosis may be mistaken as a malignant growth. This is a cause for concern in the patient and adequate counselling regarding the benign nature of the lesion must be done with histopathological evidence. Even though rare, inverted follicular keratosis should be considered as a differential among conditions like squamous cell carcinoma, basal cell carcinoma, seborrheic keratosis, keratoacanthoma and verruca [Table 1].
| Differential diagnoses | Inverted follicular keratosis | Viral warts | Seborrheic keratosis | Actinic keratosis | BCC | Squamous cell carcinoma |
|---|---|---|---|---|---|---|
| Clinical feature | Solitary papule with irregular surface and crusting | Firm papules with rough horny surface | Verrucous plaques in stuck-on appearance | Erythematous papules or plaques, adherent dry scales. With varying degrees of hyperkeratosis | Prominent surface telangiectasia. Nodular BCC is pink or red colored. Cystic center gives a translucent appearance | Verrucous or ulcerated plaque with an ill-defined base extending beyond tumor margins |
| Dermoscopic feature | Yellow-white structureless areas, keratin plugs, red dots, hairpin vessels with white halo | Lobular, frog spawn structure, red dots, and loss of dermatoglyphics | Cerebriform pattern, comedo-like openings, milia-like cysts, moth eaten border and hairpin vessels | Erythema in reddish vascular pseudo network, yellow-white scales, thin and wavy vessels, follicular openings with keratotic plugs5 | Arborizing vessels or surface telangiectasia over milky red background (vascular blush). Blue gray nests and spoke wheel pattern also | White structureless area, white perifollicular areas, blood spots, polymorphic vessels3 |
| Histopathological feature | Hyperkeratosis, inverted papillomatosis, acanthosis and squamous eddies with endo exophytic growth | Acanthosis, hyperkeratosis, koilocytosis, papillomatosis | Hyperkeratosis, irregular acanthosis, keratin filled invaginations, marked papillomatosis, squamous eddies in irritated variant with exophytic growth | Hyperkeratosis, parakeratosis, loss of polarity, nuclear crowding, nuclear hyperchromatism, hypogranulosis, nuclear pleomorphism, increased epidermal mitotic activity | Marginal palisading pattern with well-organized stroma. Mitotic figures are seen. Tumor buds appear from the epidermis | Atypical keratinocytes breach epidermal basement membrane, and invade the dermis. Pleomorphic cells are seen |
BCC = basal cell carcinoma
Surgical excision ensuring complete removal can be difficult in delicate areas. Topical 5% imiquimod cream has been used only rarely for this condition so far. Our experience shows that application of topical imiquimod is safe and effective even in such delicate areas if used judiciously.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Inverted follicular keratosis successfully treated with imiquimod. Indian Dermatol Online J. 2016;7:177-9.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of inverted follicular keratosis: Study of 12 cases. Clin Exp Dermatol. 2016;41:468-73.
- [CrossRef] [PubMed] [Google Scholar]
- Inverted follicular keratosis: Dermoscopic and reflectance confocal microscopic features. Dermatology. 2013;227:62-6.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple inverted follicular keratoses as a presenting sign of Cowden's syndrome: Case report with human papillomavirus studies. J Am Acad Dermatol. 2004;51:411-5.
- [CrossRef] [PubMed] [Google Scholar]





