Translate this page into:
Accidental high-dose methotrexate toxicity due to an electronic prescribing error
Correspondence Address:
Ercan �aliskan
Department of Dermatology, Gulhane School of Medicine, Etlik/Kecioren/Ankara - 06018
Turkey
| How to cite this article: �aliskan E, Tunca M, A�ikg�z G, Arca E, Akar A. Accidental high-dose methotrexate toxicity due to an electronic prescribing error. Indian J Dermatol Venereol Leprol 2014;80:268-269 |
Sir,
Methotrexate is widely used in psoriatic patients and methotrexate toxicity is a relatively frequent problem. High-dose methotrexate intoxication, however, is rarely reported. [1] Most cases are patients who have taken several times the usual doses due to misinterpretation of complex weekly oral schedules.
A 45-year-old man was referred to our clinic with oral ulcerations and pustular lesions on his psoriatic plaques. He had been treated variously over 10 years with cyclosporine, acitretin, as well as psoralen ultraviolet A (PUVA), and methotrexate had been prescribed recently. Five days after the 1 st intramuscular injection of what was supposed to be a 25 mg dose (half of a 50 mg vial), he developed mouth sores and his psoriatic plaques flared, becoming reddish, itchy and painful.
On the 7 th day after the injection, his psoriatic lesions were seen to be scaly and surrounded by a vivid erythema; there were also tiny pustules within these lesions [Figure - 1]. Although his vital signs were stable, and complete blood counts as well as routine biochemistry were normal, he was admitted to our hospital for suspected methotrexate toxicity. We could not determine his serum methotrexate levels but his records in the nationwide electronic prescription system revealed that 5 g/50 ml of methotrexate had been prescribed. Sodium bicarbonate was therefore started for alkalization of urine; however, leucovorin rescue therapy was not initiated as the injection had been given more than seven days earlier.
 |
| Figure 1: Pustular eruptions of MTX toxicity. Initial pustular lesions of psoriatic plaques following MTX injection located on the knees and hands |
By the third day of hospitalization, his absolute neutrophil count (ANC) had decreased to 400/mm 3 and he developed a high fever. Granulocyte-colony stimulating factor (G-CSF) therapy and prophylactic imipenem were initiated. The skin and oral lesions subsequently worsened and total parenteral nutrition had to be added. On the sixth day, the pustular lesions began to crust and ulcerate. A unit of platelet suspension was transfused since the platelet count had decreased to 12000/ml and a fecal occult blood test was found positive. Liver enzymes were elevated at this point (ALT: 155 U/L, AST: 72 U/L), while renal function tests remained normal. On day 8, his lesions began to resolve and the hematologic parameters started to improve. On day 10, the ANC had risen to 3270/mm 3 . Granulocyte-colony stimulating factor and antibiotic treatments were stopped, and oral feeding was resumed. By day 12 of his hospital stay, the liver enzymes had regressed to normal values and he was discharged on the 14 th day with almost complete clinical remission.
A computerized prescriber order entry system was recently introduced in our country. The use of computerized prescriptions appears to be a promising strategy to reduce prescription errors. A study in Spain showed that medication errors were minimized after implementation of an e-prescription system, especially dosage related errors. [2] The authors attributed this to the e-system providing the usual doses of drugs by default. The software in our country, however, does not include default dosages. We believe that the unfamiliarity of the prescribing dermatologist with this system coupled with a numerical similarity between the intended dose (50 mg) and volume of the vial (50 ml) [Figure - 2] caused confusion in both the prescribing dermatologist and the nurse injecting the dose, leading to a very high dose being administered inadvertently.
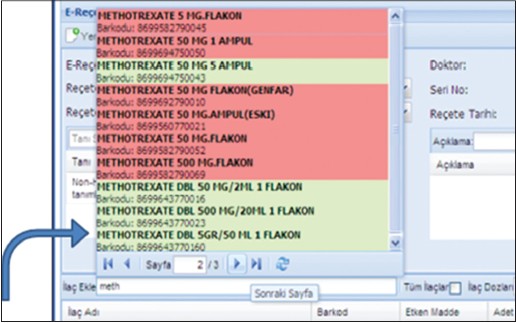 |
| Figure 2: Computer-assisted order entry of methotrexate. The screen shot of the e-recipe showing the drugs with different methotrexate doses |
High-dose methotrexate is used in the treatment of malignant diseases along with appropriate preventive measures such as leucovorin rescue. Accidental high-dose methotrexate intoxication has rarely been reported. In a Pubmed search, we found only one report of toxicity probably due to a high dose of methotrexate, [1] in which a psoriatic patient self-administered an unknown dose and subsequently developed ulcerative lesions which were considered a diagnostic clue.
Pustular and ulcerative lesions are a rare but striking manifestation of methotrexate toxicity; [1],[3],[4],[5] pathogenic mechanisms beyond direct toxicity are yet to be elucidated. Almost all reported cases are patients who were on oral methotrexate. [2],[3],[4],[5] Pearce et al., have also described two patients with erosions of their psoriatic lesions as a sign of methotrexate toxicity. [3] They stated that the clinical features in their patients were similar to those in patients described previously and emphasized that erosions on psoriatic plaques constitute an early sign of methotrexate toxicity. In our case too, the pustular eruptions on psoriatic plaques served as a herald of possible methotrexate toxicity leading us to hospitalize the patient despite the limited number of lesions and initially normal laboratory findings. Clinicians should therefore recognize pustular lesions evolving into ulceration in a psoriatic patient on methotrexate as a warning sign.
| 1. |
Fridlington JL, Tripple JW, Reichenberg JS, Hall CS, Diven DG. Acute methotrexate toxicity seen as plaque psoriasis ulceration and necrosis: A diagnostic clue. Dermatol Online J 2011;17:2.
[Google Scholar]
|
| 2. |
Villamañán E, Larrubia Y, Ruano M, Vélez M, Armada E, Herrero A, et al. Potential medication errors associated with computer prescriber order entry. Int J Clin Pharm 2013;35:577-83.
[Google Scholar]
|
| 3. |
Pearce HP, Wilson BB. Erosion of psoriatic plaques: An early sign of methotrexate toxicity. J Am Acad Dermatol 1996;35:835-8.
[Google Scholar]
|
| 4. |
Hocaoglu N, Atilla R, Onen F, Tuncok Y. Early-onset pancytopenia and skin ulcer following low-dose methotrexate therapy. Hum Exp Toxicol 2008;27:585-9.
[Google Scholar]
|
| 5. |
Agarwal KK, Nath AK, Thappa DM. Methotrexate toxicity presenting as ulceration of psoriatic plaques: A report of two cases. Indian J Dermatol Venereol Leprol 2008;74:481-4.
[Google Scholar]
|
Fulltext Views
4,584
PDF downloads
1,358





