Translate this page into:
Acquired cutis laxa of face with multiple myeloma
Correspondence Address:
Tulika A Yadav
Department of Dermatology, King Edward Memorial Hospital, Parel, Mumbai, Maharashtra
India
| How to cite this article: Yadav TA, Dongre AM, Khopkar US. Acquired cutis laxa of face with multiple myeloma. Indian J Dermatol Venereol Leprol 2014;80:454-456 |
Sir,
Cutis laxa is a rare dermatosis characterized by diffuse laxity of skin resulting in a prematurely aged appearance. It is most commonly an inherited condition. The acquired form is rare and has been associated with various conditions, including multiple myeloma, monoclonal gammopathy of undetermined significance, and heavy chain deposition disease. Cutis laxa usually follows a progressive course and there is no definitive treatment available. [1] We describe a 44-year-old female with multiple myeloma and cutis laxa localized to the face. She developed anasarca, which subsided following treatment for multiple myeloma leaving lax and wrinkled skin all over the body. Lax skin improved spontaneously elsewhere but persisted on the face.
A 44-year-old female presented to us with a two-year history of loosening of skin over the face. Two years back, she had developed severe anaemia with associated anasarca and exertional dyspnea. She also had heavy proteinuria, hypoproteinemia and progressive renal failure. A kidney biopsy was performed which revealed mesangial cell proliferation and lobular accentuation of glomerular tufts with marked mesangial matrix deposition and eosinophilic periodic acid Schiff (PAS) positive nodules. Immunofixation electrophoresis on a 24-hour urine sample was positive for kappa light chains. Serum immunofixation electrophoresis (IFE) revealed a stable monoclonal IgG-λ M-spike (0.5 g/dL). Serum β2 -microglobulin was increased. Bone marrow examination revealed 14% plasma cells. Based on these findings, a diagnosis of early multiple myeloma with nephrotic syndrome was made. She was started on a chemotherapy regimen consisting of thalidomide (100 mg/day), oral cyclophosphamide (150 mg/day) both for the first five days in every month with weekly intravenous dexamethasone (40 mg/week) along with loop diuretics. In addition, the patient was prescribed bortezomib which was discontinued by the patient after two months. Following one year of treatment, the anasarca subsided leaving behind loose wrinkled skin all over the body. Over the next one year, the skin over the extremities and the abdomen reverted back to normal; however, loosening of skin persisted over the face.
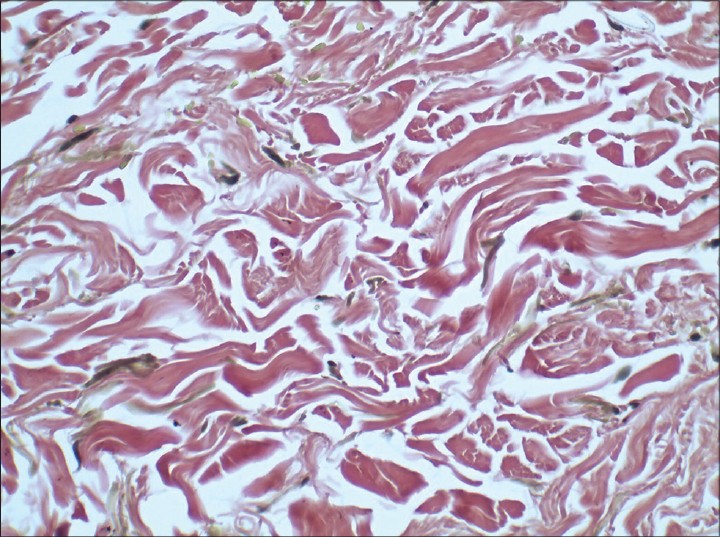
Examination revealed a healthy-appearing woman, who appeared older than her stated age [Figure - 1]. She had loose, sagging skin on the face and neck giving her a hound-dog facies [Figure - 2]. Skin over the ear lobules was lax. On stretching of the skin over face, no elastic recoil was seen. Her systemic examination was also normal. Hematoxylin and eosin (H and E) stained sections from a skin biopsy from the face showed a mixed cell infiltrate of lymphocytes and occasional neutrophils [Figure - 3]. A special stain to demonstrate elastic tissue (Verhoff van Gieson) showed fragmented and clumped elastic fibers [Figure - 4].
 |
| Figure 1: Loose sagging folds of skin over the face |
 |
| Figure 2: Loose folds of skin over the neck |
 |
| Figure 3: A sparse infiltrate of lymphocytes and few histiocytes are seen in the dermis seen on H and E, (×100) |
 |
| Figure 4: VVG stained sections showing clumped and fragmented elastic fibers (×400) |
Based on her clinical features, a diagnosis of acquired cutis laxa localized to the face following multiple myeloma was made and she was referred to a plastic surgeon for surgical correction of redundant folds.
Cutis laxa is a rare condition characterized clinically by lax, pendulous skin and histologically by loss of elastic tissue in the dermis. It is a heterogeneous condition, which may be inherited as a dominant, recessive or X-linked recessive disease, or it may be acquired. The face and neck are often affected, which produces a ′bloodhound′ appearance of premature aging. Mild trauma can lead to purpura due to skin fragility and this may lead to formation of fibrotic nodules over the bony prominences. There may be widespread, massive folds of lax skin, or the changes may be mild and confined to a limited area. Such cases may be confused as having anetoderma. The acquired cephalic form of localized cutis laxa presents characteristically as large, hanging loose ear lobes, blepharochalasis and lax nasolabial folds. Organs other than the skin may also be involved. Internal organ abnormalities like emphysema, gastric fibromas and tracheobronchomegaly have been reported. [2]
Histologically, the skin is of normal thickness, but the elastic fibers are sparse, short, fragmented and clumped, particularly in the upper dermis, and they show granular degeneration. [3] The elastic fibers are found to be deficient in elastin, though their microfibrils appear normal. Similar changes in elastic fibers may occur in the lungs and aorta. [4],[5] There are occasional case reports of multiple myeloma and other plasma cell dyscrasias associated with cutis laxa. [6]
It is likely that paraproteinemia resulting in the deposition of immune complexes possibly leads to the release of inflammatory cytokines and subsequent destruction of elastic fibers. Surgical repair seems to be the only therapeutic choice, but the results are variable and temporary.
| 1. |
Ferrándiz-Pulido C, Serra M, Bel S, Ferrer B, Repiso T, Garcia-Patos V. Multiple myeloma-associated amyloidosis presenting with acrolocalized acquired cutis laxa. Arch Dermatol 2010;146:1433-4.
[Google Scholar]
|
| 2. |
Wanderer AA, Ellis EF, Goltz RW, Cotton EK. Tracheobronchomegaly and acquired cutis laxa in a child. Physiologic and immunologic studies. Pediatrics 1969;44:709-15.
[Google Scholar]
|
| 3. |
Hashimoto K, Kanzaki T. Cutis laxa. Ultrastructural and biochemical studies. Arch Dermatol 1975;111:861-73.
[Google Scholar]
|
| 4. |
Marchase P, Holbrook K, Pinnell SR. A familial cutis laxa syndrome with ultrastructural abnormalities of collagen and elastin. J Invest Dermatol 1980;75:399-403.
[Google Scholar]
|
| 5. |
Sephel GC, Byers PH, Holbrook KA, Davidson JM. Heterogeneity of elastin expression in cutis laxa fibroblast strains. J Invest Dermatol 1989;93:147-53.
[Google Scholar]
|
| 6. |
New HD, Callen JP. Generalized acquired cutis laxa associated with multiple myeloma with biphenotypic IgG- λ and IgA-κ gammopathy following treatment of a nodal plasmacytoma. Arch Dermatol 2011;147:323-8.
[Google Scholar]
|
Fulltext Views
3,686
PDF downloads
1,454





