Translate this page into:
Acrosyringeal lichen planus of palm
Correspondence Address:
Rameshwar M Gutte
Department of Dermatology, OPD No. 128, 1st floor, Dr. L. H. Hiranandani Hospital, Powai, Mumbai - 400076
India
| How to cite this article: Gutte RM. Acrosyringeal lichen planus of palm. Indian J Dermatol Venereol Leprol 2012;78:521 |
Sir,
Lichen planus (LP) is a pruritic, benign, papulosquamous, inflammatory dermatosis of unknown etiology that affects either or all of the skin, mucus membrane, hair and nail. In its classic form, it presents with violaceous, scaly, flat-topped, polygonal papules.
Commonly it affects extremities and mucus membranes. [1],[2]
A 23-year-old unmarried male presented with asymptomatic hyperpigmented keratotic plaques with punctate keratoses and pits over bilateral palms since two months. These lesions were gradual in onset and progressive in nature. They started with keratotic papules and later coalesced to form plaques. There was no history of vesiculation or oozing or of similar lesions elsewhere on the body. Examination revealed four hyperpigmented, hyperkeratotic plaques with punctate keratoses and pits over them at places [Figure - 1] and [Figure - 2]. No other skin lesions were seen on the body. Nails and oral mucosa were normal.
 |
| Figure 1: Hyperkeratotic, hyperpigmented plaque with punctate keratoses over inner arch and middle finger of right palm |
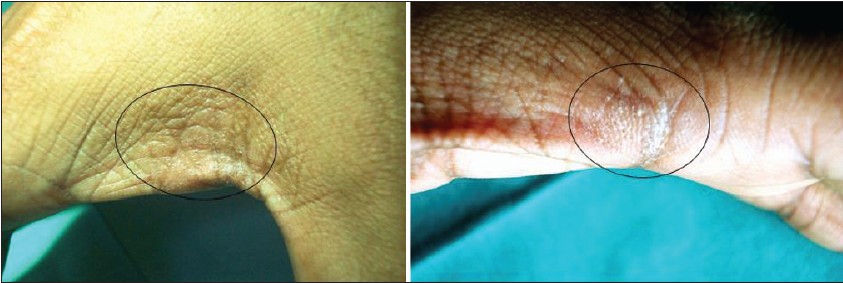 |
| Figure 2: Symmetric, hyperkeratotic, slightly hyperpigmented plaque with multiple pits over them on first web space |
A diagnosis of palmar lichen nitidus and LP was thought and a skin biopsy from a plaque was obtained.
Histopathological examination of biopsy showed compact orthokeratosis, hypergranulosis, irregular slightly saw-tooth acanthosis with focal vacuolar alteration of basal layer with degeneration of basement membrane and scattered necrotic keratinocytes. In papillary dermis, band-like dense lymphocytic infiltrate with congested capillaries and occasional melanophages was seen [Figure - 3]. A dermal lymphocytic infiltrate mainly in juxtaposition to the acrosyringium and liquefaction degeneration of the acrosyringeal basal cell layer were seen as prominent findings [Figure - 4]a. Also dilated acrosyringium with orthokeratotic plug was seen corresponding to punctate keratoses seen clinically [Figure - 4]b. However, epidermal perforation could not be found even on multiple step sections and thus cause of pits seen clinically remained unknown. On clinicopathological correlation, a diagnosis of acrosyringeal LP of palm was made. Patient is advised to apply topical clobetasol and 3% salicylic acid cream twice daily along with moisturizers and is under follow-up.
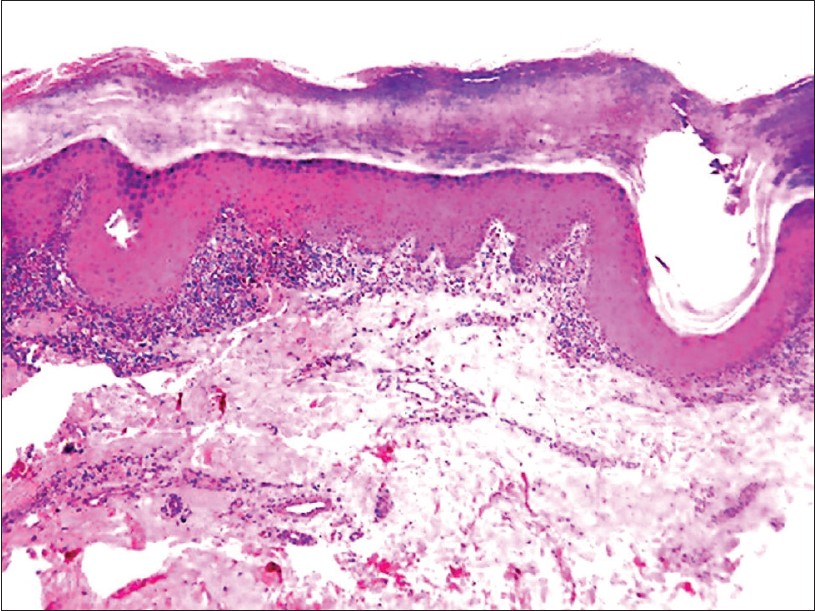 |
| Figure 3: Hyperkeratosis, hypergranulosis, irregular acanthosis and band-like lymphocytic infiltrate in dermis with interface change. (H and E, 40×) |
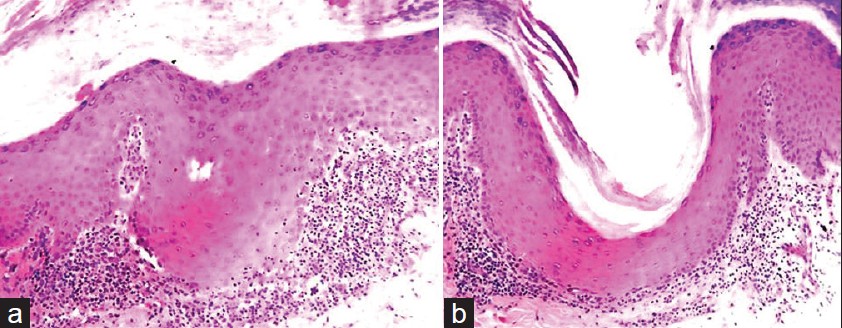 |
| Figure 4: (a) Vacuolar alteration of basal layer with squamatization involving mainly acrosyringium. (H and E, ×100) (b) Dilated acrosyringium with orthokeratotic plug with liquefactive degeneration of the acrosyringeal basal cell layer (H and E, ×100) |
Involvement of palms and soles is rare in LP. In a clinico-etiological study of 375 LP patients, involvement of the palms was seen in only 3.5% and of soles in 4.3% of the cases. [2],[3] Palmoplantar LP usually presents with yellowish hyperkeratotic plaques with or without itching. [1] However, there is wide variation in lesions of palmoplantar LP.
Various morphological patterns of palmoplantar LP have been described, including erythematous scaly plaques, yellowish hyperkeratotic papules, diffuse keratoderma, ulcerated lesions, vesicle-like papules, diffuse palmar hyperpigmentation, umbilicated papules [3],[4],[5],[6],[7] hyperkeratotic pitted plaques with perforation of epidermis (perforating LP) [7] and punctate keratotic plaques (as in present case).
Due to this varied clinical presentation, histopathology is usually needed to confirm diagnosis in such cases.
Keratotic plaques with punctate keratoses or pitting over palms are always a diagnostic dilemma. The conditions to be considered for such presentation as in our case are punctate porokeratosis, lichen nitidus, punctate palmoplantar keratoderma, arsenical keratoses and porokeratotic eccrine ostial and dermal duct nevus. Isolated pitting of palms is also seen in pitted keratolysis, Darrier White disease, Gorlin syndrome, dyskeratosis congenita, Cowden′s syndrome, basaloid follicular hamartomas and aquagenic keratoderma. [3],[7] Khandpur et al. reported four cases of hyperkeratotic pitted plaques on palms and soles and suggested that hyperkeratotic plaques with pits on the palm and soles are highly suggestive of lichenoid pathology and should prompt search for LP or lichen nitidus at other sites. Presence of plugs within the pits is suggestive of LN and violaceous rim indicates LP. [3] Histologically lichen nitidus will show granulomatous pathology with classic "claw clutching a ball" appearance.
One of the characteristic finding seen in our case was acrosyringeal accentuation of dermal infiltrate. Enhamre et al. have described cases of LP with dermal lymphocytic infiltrate in juxtaposition to acrosyringium with liquefactive degeneration of acrosyringeal basal cell layer as a prominent histological finding and coined the term acrosyringeal LP. [8] Mugoni et al. described five cases of LP on palms with acrosyringeal LP in one of them. [6] Drugs such as β-blockers that are excreted through sweat ducts may influence its physiology by involving β-adrenergic receptors to produce predominant acrosyringeal changes. However, our patient did not have any history of drug intake. Mugoni et al. stated that acrosyringium constitutively expresses class 2 major histocompatibility antigens (HLA-DR, HLA-DP, HLA- DQ) on surface, and this expression of antigens in association with cell-mediated immune mechanisms in certain circumstances, could allow antigen presentation to T cells giving rise to immune response involving predominantly acrosyringium. [6]
Various treatment modalities for palmoplantar LP include topical steroid with emollients, keratolytic agents like salicylic acid, topical tazarotene and systemic steroid, acitretin, subcutaneous enoxaparin and oral immunosuppressants like cyclosporine have been used successfully. Psoralen plus ultraviolet A (PUVA) and PUVA bathing, showed good response in resistant cases. Surgical treatment with excision and grafting can be used in painful erosive cases resistant to other modalities. [2],[3],[4]
| 1. |
Inamdar AC, Palit A. On lichen planus and lichenoid disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology, 3 rd ed. Mumbai, India: Bhalani Publishers; 2008. p. 1070-86.
[Google Scholar]
|
| 2. |
Sanchez-Perez J, Buceta LR, Fraga J, Garcia-Diez A. Lichen planus with lesions on the palms and/or soles: Prevalence and clinicopathological study of 36 patients. Br J Dermatol 2000;142:310-4.
[Google Scholar]
|
| 3. |
Khandpur S, Kathuria SD, Gupta R, Singh MK, Sharma VK. Hyperkeratotic pitted plaques on palms and soles. Indian J Dermatol Venereol Leprol 2010;76:52-5.
[Google Scholar]
|
| 4. |
Gündüz K, Inanir I, Türkdogan P, Sacar H. Palmoplantar lichen planus presenting with vesicle-like papules. J Dermatol 2003;30:337-40.
[Google Scholar]
|
| 5. |
Vijay Kumar M, Thappa DM, Gupta S. Diffuse palmar hyperpigmentation in lichen planus. Indian J Dermatol 2000;45:182-4.
[Google Scholar]
|
| 6. |
Mugoni MG, Montesu MA, Cottoni F. Lichen planus on palms and soles. J Eur Acad Dermatol Ven Wereol 1994;3:535-40.
[Google Scholar]
|
| 7. |
Gutte R, Khopkar U. Perforating lichen planus. Indian J Dermatol Venereol Leprol 2011;77:515-7.
[Google Scholar]
|
| 8. |
Enhamre A, Lagerholm B. Acrosyringeal lichen planus. Acta Derm Venereol 1987;67:346-50.
[Google Scholar]
|
Fulltext Views
5,160
PDF downloads
1,903





