Translate this page into:
Acute generalised exanthematous pustulosis secondary to spider bite
Corresponding author: Dr. Ranjana Beniwal, Department of Dermatology, Dr. Sampurnanand Medical College and Associated Group of Hospitals, Jodhpur, India. ranjanabeniwal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Beniwal R, Agrawal A, Joshi YR, Singhvi A. Acute generalised exanthematous pustulosis secondary to spider bite. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_249_2024
Dear Editor,
A 22-year-old woman presented to the dermatology outpatients with numerous pus-filled lesions on her body associated with a fever (38.6°C) since 12 hours. She gave a history of being bitten by a spider the night before the onset of lesions. There was no history of any other drug intake prior to the onset of lesions, comorbidity, or any other systemic complaints. Examination revealed multiple discrete to confluent non-follicular pustules over a background of erythema and oedema on the trunk, predominantly involving flexures, including axillae and groin with some desquamation in the groin [Figure 1a and 1b]. A 2×4 cm necrotic eschar with peripheral erythema was present at the site of a spider bite on the lateral aspect of the trunk below the left axilla [Figure 1c]. Mucosae were uninvolved. Gram staining and KOH (potassium hydroxide) staining from the pustule was non-contributory. A complete haemogram showed leucocytosis (14×109/L) with neutrophilia (80%) and mild eosinophilia (7%). Liver and kidney function tests, urine microscopy, and random blood glucose were within normal limits. Histopathology showed subcorneal and intraepidermal spongiform pustules, and oedema of the papillary dermis with diffuse perivascular infiltration of neutrophils and a few eosinophils [Figure 2]. The patient was diagnosed as a case of AGEP secondary to a spider bite in accordance with the EUROSCAR (European study of severe cutaneous adverse reactions) criteria. Following a short course of oral prednisolone in tapering doses starting at 40 mg/day and stopped in 12 days. and supportive therapy (topical betamethasone dipropionate lotion, emollients and anti-histamines), there was complete recovery in seven to ten days.
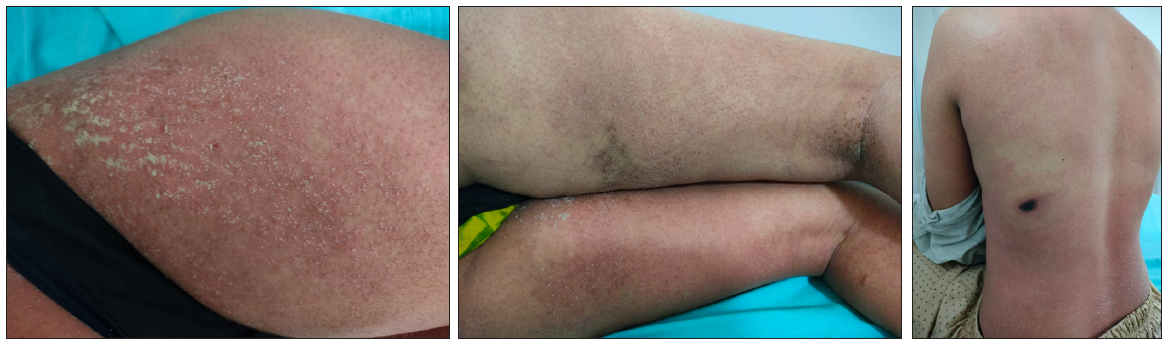
- Multiple non-follicular sterile pustules with background erythema; (a) in the groin and, (b) over thighs and popliteal fossa (c) over lower back along with necrotic eschar of spider bite on the lateral aspect of trunk.
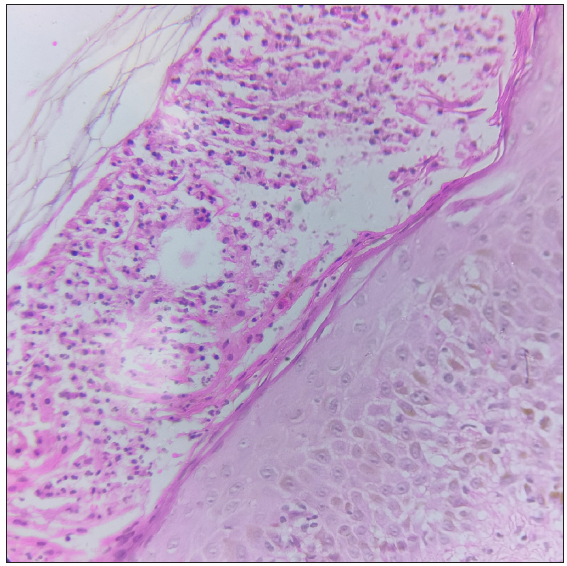
- Histopathology showing dermal edema with perivascular mixed inflammatory infiltrate and subcorneal pustule with neutrophils (Haematoxylin and eosin, 400x)
AGEP is a rare type of SCAR in which tiny non-follicular sterile pustules with underlying erythema develop and spread rapidly.1 Mucosal involvement is mild and occurs in approximately 20% of cases. Unusual manifestations have also been reported, which include erythema multiforme-type lesions, edema of face and hands, purpura, vesicles, and blisters. Histopathology typically shows spongiform subcorneal and/or intraepidermal pustules, marked papillary dermal edema, and eventually vasculitis, eosinophils, and/or focal necrosis of keratinocytes.2
Most cases of AGEP occur secondary to drugs, especially antibiotics, but cases have also been documented following infections, vaccinations, dietary triggers, or physical contact.1 Patch testing and in vitro assays have suggested that AGEP is a T-cell-mediated, delayed-type hypersensitivity reaction to a specific drug or other triggers.3
Recently, spider bite has been linked as a trigger of AGEP. Possible pathogenetic mechanism includes the stimulation of cytokines, including IL-8 (interleukin-8) and GM-CSF (granulocyte-macrophage colony-stimulating factor). IL-8 and GM-CSF are implicated in the recruitment of polymorphononuclear cells into the epidermis, contributing to neutrophilic infiltration and survival. This stimulation is proposed to be due to sphingomyelinase, an enzyme which is present in the venom of the spider.3,4
AGEP is usually self-limiting with clinical resolution within two weeks in most cases.2 It has been reported that the latent period is shorter in the cases of AGEP due to a spider bite varying from one to three days as compared to drug-induced AGEP (less than four days).5
Although drugs still remain the most common cause of AGEP, spider bite has emerged as a rare cause of AGEP that clinicians need to be aware of, especially in cases where there is no relevant drug history. We report this case to emphasise this rarity.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Acute Generalized Exanthematous Pustulosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
- [Google Scholar]
- Acute generalized exanthematous pustulosis (AGEP)—A clinical reaction pattern. J Cutan Pathol. 2001;28:113-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acute generalized exanthematous pustulosis (AGEP) triggered by a spider bite. Allergol Int. 2009;58:301-3.
- [CrossRef] [PubMed] [Google Scholar]
- Acute generalized exanthematous pustulosis following a spider bite: Report of 3 cases. J Am Acad Dermatol. 2006;55:525-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acute generalized exanthematous pustulosis caused by a probable spider bite: A case report and review of the literature. Turkderm-Turk Arch Dermatol Venereol. 2020;54:152-5.
- [CrossRef] [Google Scholar]





