Translate this page into:
Adalimumab as a successful treatment for acne fulminans and bilateral acute sacroiliitis with hip synovitis complicating isotretinoin therapy
2 Department of Physical Medicine and Rheumatology, Benha University, Banha, Egypt; Department of Rheumatology, Alhada Armed Forces Hospital, Taif, Saudi Arabia,
3 Department of Radiology, Benha University, Banha, Egypt; Department of Radiology, Alhada Armed Forces Hospital, Taif, Saudi Arabia,
4 Department of Dermatology, Zagazig University, Zagazig, Egypt
Correspondence Address:
Noha Mohammed Dawoud
Department of Dermatology, Andrology and S.T.Ds, Faculty of Medicine, Menoufia University, Shebin El kom 32817, Menoufia, Egypt
| How to cite this article: Dawoud NM, Elnady BM, Elkhouly T, Yosef A. Adalimumab as a successful treatment for acne fulminans and bilateral acute sacroiliitis with hip synovitis complicating isotretinoin therapy. Indian J Dermatol Venereol Leprol 2018;84:104-107 |
Sir,
We report a case of an adolescent male patient who was treated by isotretinoin for moderate acne vulgaris with sudden development of acne fulminans and incapacitating acute sacroiliitis with bilateral hip arthritis presenting new challenges for therapy.
A 16-year-old male patient presented to the emergency unit of Al-Hada armed forces hospital, Taif, KSA complaining of severe progressive back pain of sudden onset with inability to ambulate. Over the last 6 months, he had received oral isotretinoin for the treatment of moderate acne vulgaris starting at 0.6 mg/kg (30 mg/d) with gradually increasing dosage till 1.5 mg/kg (80 mg/d) in the last month with no response and even worsening of lesions.
Examination revealed low-grade fever of 37.8°C and ulcerated crusted erythematous lesions with scattered pustules, nodules, and open comedones all over the face. Fistuolous tract was also detected [Figure - 1]a and [Figure - 2]a.
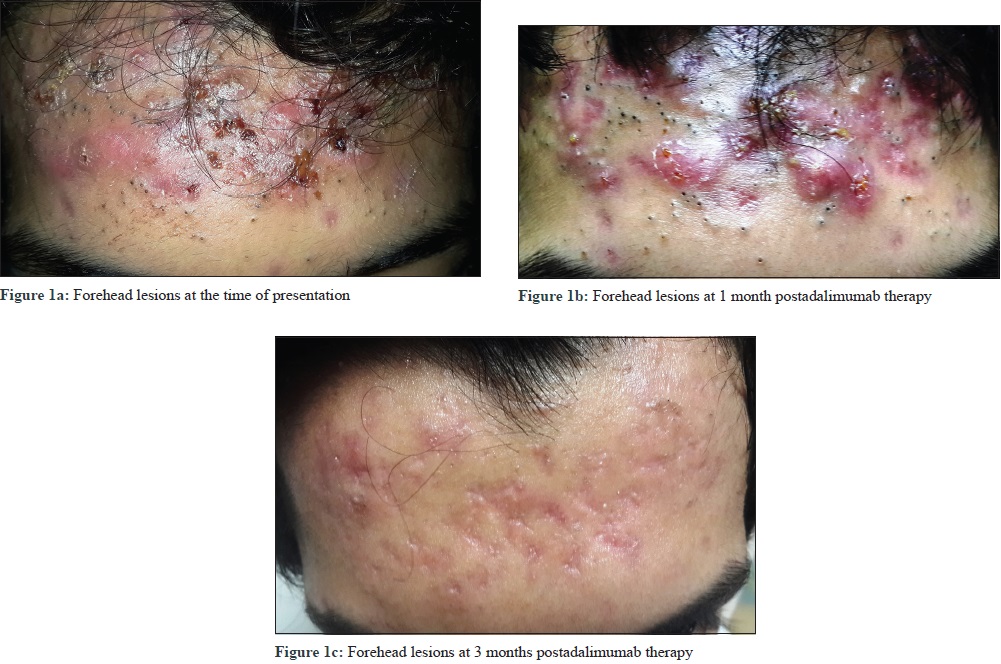 |
| Figure 1: |
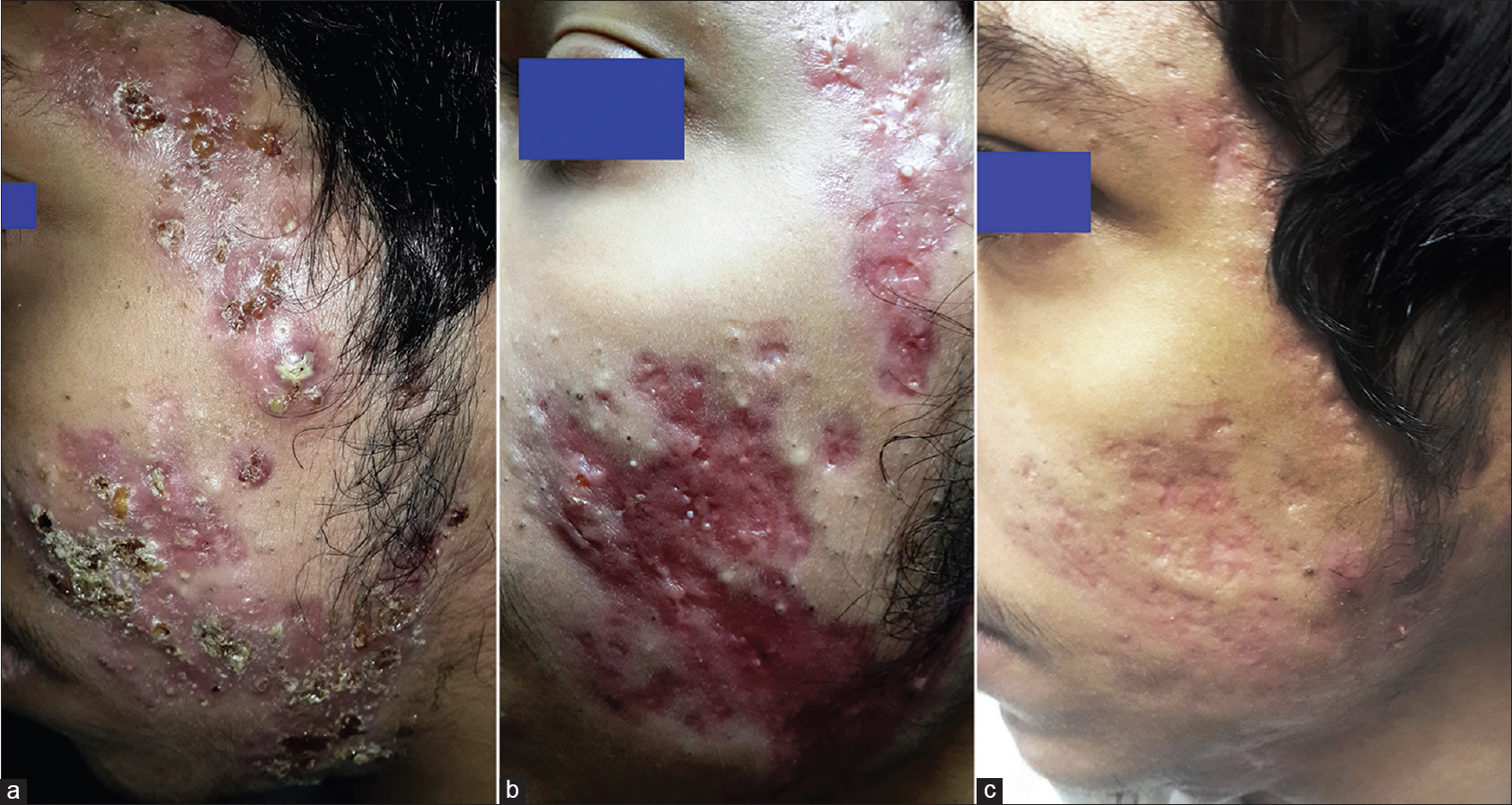 |
| Figure 2: a-c: (a)Left side of the face at the time of presentation (b) Left side of the face at 1 month postadalimumab therapy (c) Left side of the face at 3 months postadalimumab therapy |
Rheumatologic consultation reported limitation of back movement in all planes and no joint arthritis or enthesopathy. The patient was admitted for 3 days; all routine investigations were normal, except for leucocytosis. HLA B27 antigen was negative.
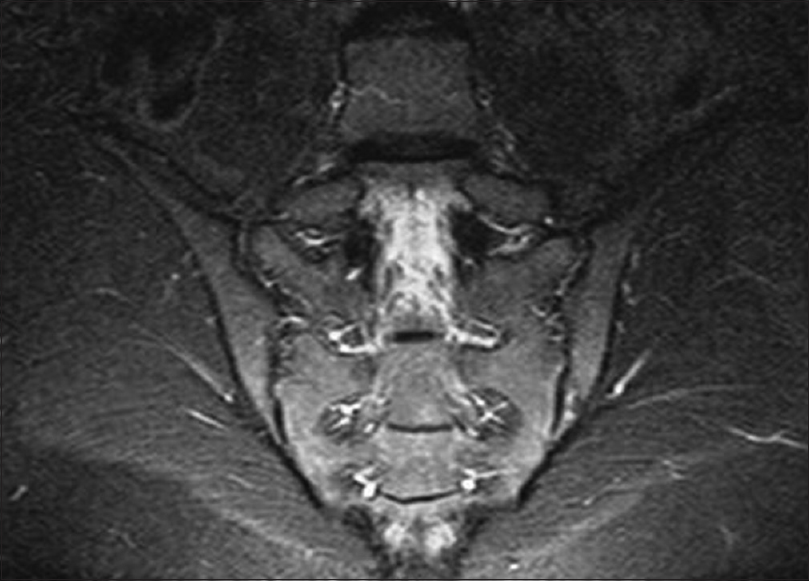
Magnetic resonance imaging (MRI) showed evidence of bilateral sacroiliitis and hip synovitis with minimal effusion[Figure 3a] and [Figure 3b]. Lumber and sacral spines were free from spondylodiscitis with no radiologic evidence of periostitis or hyperostosis.
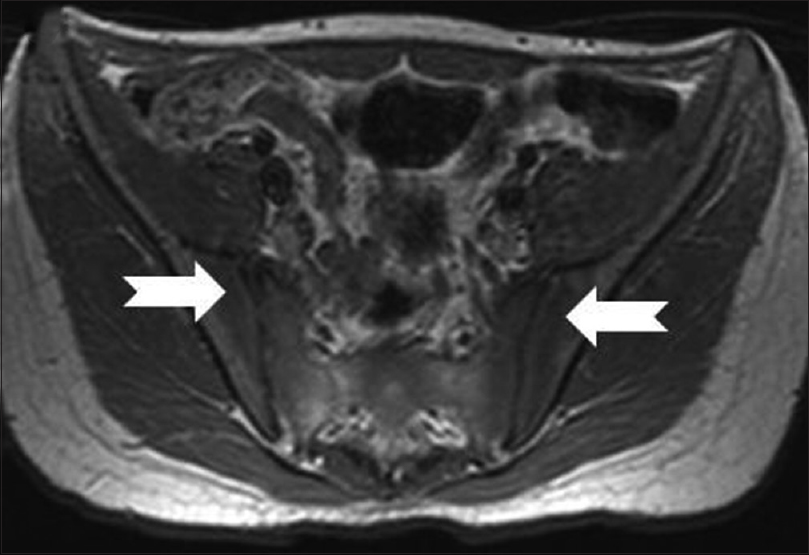 |
| Figure 3a: Magnetic resonance imaging axial T1-weighted image showing early bilateral acute sacroiliitis (dark edema signal) of both sacral and iliac sides, No gross erosions or destructive changes |
 |
| Figure 3b: Magnetic resonance imaging axial short T1 inversion recovery showing early bilateral acute sacroiliitis (bright edema signal) of both sacral and iliac sides |
Patient was diagnosed with acne fulminans and bilateral acute sacroiliitis along with hip synovitis complicating isotretinoin therapy. SAPHO syndrome was excluded because facial lesions were mainly ulcerated with few nodulocystic lesions, no radiologic evidence of hyperostosis or ostitis together with presence of systemic symptoms and inducing factor (isotretinoin). Oral isotretinoin was stopped. Prednisolone (0.6 mg/kg/d) and amoxicillin clavulanate 1 g/12 h with topical potassium permanganate 1/8000, fusidic acid cream, and benzoyl peroxide 2.5% gel were prescribed for 1 week, which resulted in mild improvement of facial lesions. Regarding musculoskeletal symptoms, two alternative full therapeutic doses of non steroidal anti inflammatory drugs were prescribed for 4 weeks without improvement. The use of systemic steroids in the management of axial spondyloarthropathy is not supported by evidence and their efficacy is controversial.[1]
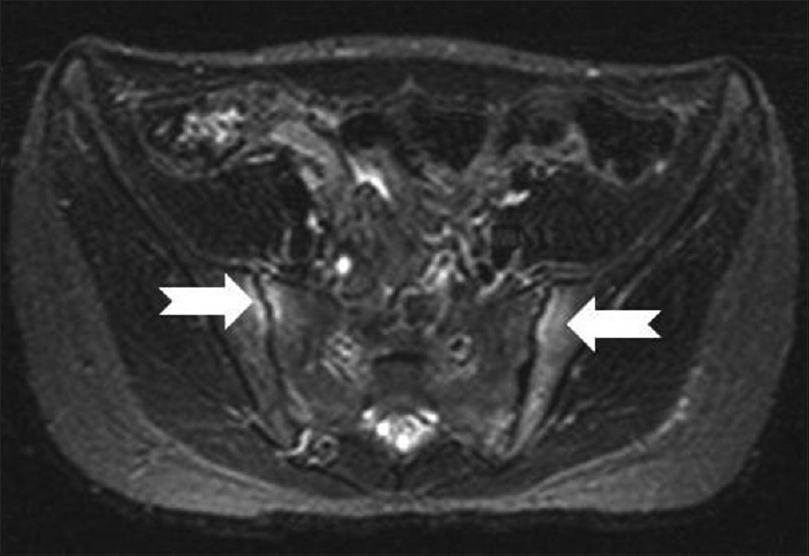
Based on previous reports of successful treatment of acne conglobata, sacroiliitis, seronegative spondyloarthropathy, and SAPHO syndrome by tumor necrosis factor-α (TNF-α) antagonists, we prescribed adalimumab (humira) 40 mg subcutaneously every other week with no loading dose on the basis of the dose used in spondyloarthropathy treatment[2],[3]. Patient's ability to move was restored after 1 week of the first injection and continued improving with subsequent injections. Acne lesions showed gradual improvement during the first month of therapy [Figure - 1]b and [Figure - 2]b, and interestingly comedones disappeared almost completely after 3 months of therapy [Figure - 1]c and [Figure - 2]c. The patient was maintained on adalimumab (humira) for 12 months without any adverse effects, which was later stopped with follow-up period of 3 months, with no relapse and complete resolution of the lesion on MRI [Figure 3c] and [Figure 3d].
 |
| Figure 3c: Follow-up magnetic resonance imaging (coronal short T1 inversion recovery) after adalimumab revealing complete resolution of the previously reported bilateral sacroiliitis with no significant marrow signal alteration |
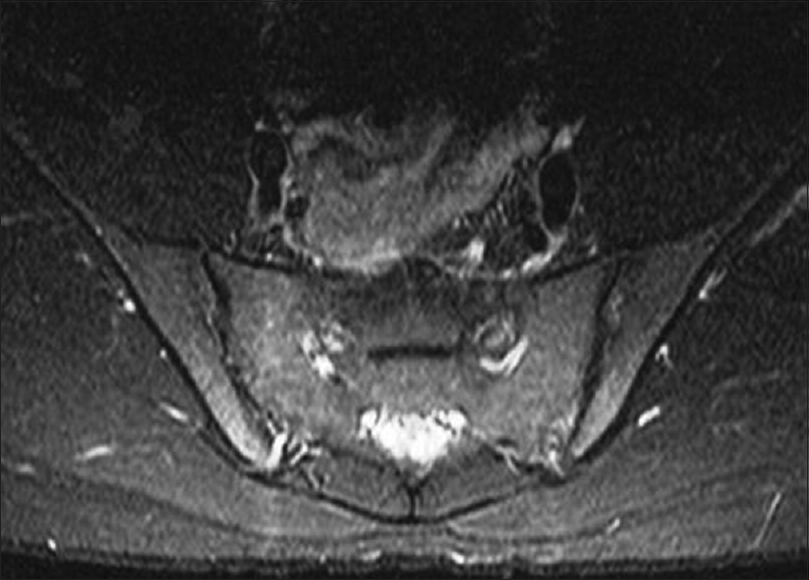 |
| Figure 3d: Follow-up magnetic resonance imaging (axial short T1 inversion recovery) after adalimumab revealing complete resolution of sacroiliitis with no significant marrow signal alteration. |
In the present case, we considered therapy with isotretinoin to be the triggering factor of acne fulminans. This could be explained by the exaggerated hypersensitivity reactions of type III and IV after massive contact with Propionibacterium acnes antigens favored by the fragility of the pilosebaceous epithelium induced by the drug.[4]
Involvement of the sacroiliac joints occurs in 21% of acne fulminans cases. Prevalence of sacroiliitis is not accurately identified in patients using isotretinoin; however, a prospective study in 2015 reported 23.1% prevalence of spondyloarthropathy in patients using isotretinoin.[5] In our case, acute sacroiliitis could be an adverse effect of isotretinoin which was prescribed in high dosage without concomitant systemic corticosteroid or as a sequelae of acne fulminans that developed as a complication to isotretinoin.
It was suggested that isotretinoin could induce solubilization of the liposomal membrane and consequently cytopathic destruction of the synovium, causing arthritis.[6] Ekisioglu and others suggested that the positivity of antigen HLA-B27 renders the patient susceptible to sacroiliitis; however, other cases described in the literature and our reported case do not prove this statement.[7],[8]
Upon failure of conventional therapies, we prescribed adalimumab. The off-label use of TNF-α antagonist was reported to successfully treat acne conglobata and sacroiliitis separately or as a component of SAPHO syndrome. Experiences with biological TNF-α blocking agents in SAPHO syndrome are few and follows the use of these drugs in spondyloarthropathy.[9] Infliximab and adalimumab each was reported to be successful in few cases.[2],[3]
Thus, our case is the first case of isotretinoin-induced acne fulminans and acute seronegative sacroiliitis that was treated successfully with adalimumab.
An in-vivo research observed a marked increase of TNF gene transcripts in acne lesions. TNF is one of the main pro-inflammatory cytokines.[10] These cytokines are responsible for further follicular hyperkeratinization and inflammatory acne lesions.
Our case provides clinical evidence for the role of TNF-α in acne vulgaris pathogenesis. The significant disappearance of comedones after 2 months of therapy underscores the effect of TNF-α not only on inflammatory lesions but also on comedogenesis. This could be explained by the effect of TNF-α on follicular hyperkeratinizaton and induction of lipogenesis.[11]
However, in SAPHO syndrome, Massara et al., denoted that anti-TNF-α therapy (infliximab) may induce persistent amelioration of osteoarticular complaints, but may exacerbate cutaneous manifestations.[9] This observation may indicate different pathomechanisms of acne and pustulosis in SAPHO syndrome or different responses to the different types of anti TNF-α therapy.
In conclusion, although acute sacroiliitis and large joint synovitis are rare complications of isotretinoin therapy, they may be so severe, incapacitating, and resistant to conventional therapy. Adalimumab could be used as a successful treatment for acute sacroiliitis and acne fulminans complicating isotretinoin therapy. Moreover, it could be a promising treatment for acne vulgaris resistant to isotretinoin therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for her images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published and due efforts will be made to conceal his entity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Braun J, van den Berg R, Baraliakos X, Boehm H, Burgos-Vargas R, Collantes-Estevez E, et al. 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis 2011;70:896-904.
[Google Scholar]
|
| 2. |
Yiu ZZ, Madan V, Griffiths CE. Acne conglobata and adalimumab: Use of tumour necrosis factor-a antagonists in treatment-resistant acne conglobata, and review of the literature. Clin Exp Dermatol 2015;40:383-6.
[Google Scholar]
|
| 3. |
Iqbal M, Kolodney MS. Acne fulminans with synovitis-acne-pustulosis-hyperostosis-osteitis (SAPHO) syndrome treated with infliximab. J Am Acad Dermatol 2005;52 5 Suppl 1:S118-20.
[Google Scholar]
|
| 4. |
Zaba R, Schwartz R, Jarmuda S, Czarnecka-Operacz M, Silny W. Acne fulminans: Explosive systemic form of acne. J Eur Acad Dermatol Venereol 2011;25:501-7.
[Google Scholar]
|
| 5. |
Alkan S, Kayiran N, Zengin O, Kalem A, Kimyon G, Kilinc EO, et al. Isotretinoin-induced Spondyloarthropathy-related Symptoms: A Prospective Study. J Rheumatol 2015;42:2106-9.
[Google Scholar]
|
| 6. |
De Francesco V, Stinco G, Campanella M. Acute arthritis during isotretinoin treatment for acne conglobata. Dermatology 1997;194:195.
[Google Scholar]
|
| 7. |
Eksioglu E, Oztekin F, Unlu E, Cakci A, Keyik B, Karadavut IK. Sacroiliitis and polyneuropathy during isotretinoin treatment. Clin Exp Dermatol 2008;33:122-4.
[Google Scholar]
|
| 8. |
Barbareschi M, Paresce E, Chiaratti A, Ferla Lodigiani A, Clerici G, Greppi F. Unilateral sacroiliitis associated with systemic isotretinoin treatment. Int J Dermatol 2010;49:331-3.
[Google Scholar]
|
| 9. |
Massara A, Cavazzini PL, Trotta F. In SAPHO syndrome anti-TNF-alpha therapy may induce persistent amelioration of osteoarticular complaints, but may exacerbate cutaneous manifestations. Rheumatology (Oxford) 2006;45:730-3.
[Google Scholar]
|
| 10. |
Yang JK, Wu WJ, Qi J, He L, Zhang YP. TNF-308 G/A polymorphism and risk of acne vulgaris: A meta-analysis. PLoS One 2014;9:e87806.
[Google Scholar]
|
| 11. |
Choi JJ, Park MY, Lee HJ, Yoon DY, Lim Y, Hyun JW, et al. TNF-a increases lipogenesis via JNK and PI3K/Akt pathways in SZ95 human sebocytes. J Dermatol Sci 2012;65:179-88.
[Google Scholar]
|
Fulltext Views
6,298
PDF downloads
2,356





