Translate this page into:
Adult onset, hypopigmented solitary mastocytoma: Report of two cases
2 Department of Pathology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi - 110 095, India
Correspondence Address:
A Singal
B-14, Law Apartments, Karkardooma, Delhi - 110 092
India
| How to cite this article: Pandhi D, Singal A, Aggarwal S. Adult onset, hypopigmented solitary mastocytoma: Report of two cases. Indian J Dermatol Venereol Leprol 2008;74:41-43 |
Abstract
Solitary mastocytoma is known to occur predominantly in children below 2 years of age and onset in adulthood is rare. Lesions are hyperpigmented in the majority of cases owing to the stimulation of melanin synthesis by mast cell growth factor. We hereby report two patients with adult onset solitary mastocytoma presenting as hypopigmented plaque. The first case was a 24-year-old man who presented with a plaque on the back of the neck of 5 years duration. The second case was a 30-year-old man who had a well-defined solitary, oval 3 x 2.5 cm plaque on the nape of the neck. Stroking of lesion resulted in a wheal with flare (Darier's sign) in both cases. Systemic examination was within normal limits in both cases. Histopathology revealed a dense toluidine blue-positive infiltrate of mast cells in the upper dermis in both cases. |
| Figure 4: Oval, hypopigmented plaque with positive Darier�s sign in Case 2 |
 |
| Figure 4: Oval, hypopigmented plaque with positive Darier�s sign in Case 2 |
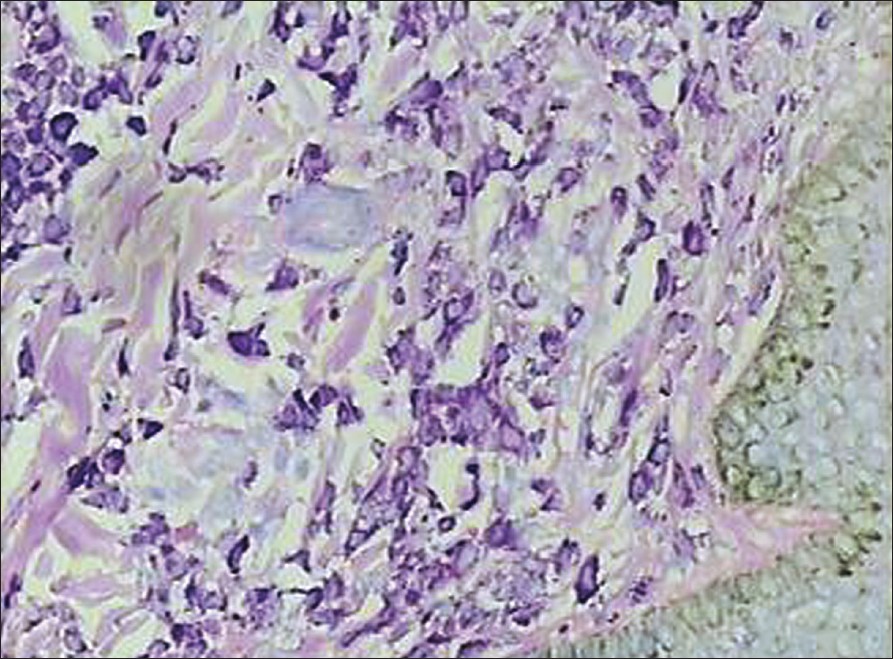 |
| Figure 3: Toluidine blue positive mast cells in the dermis (X400) |
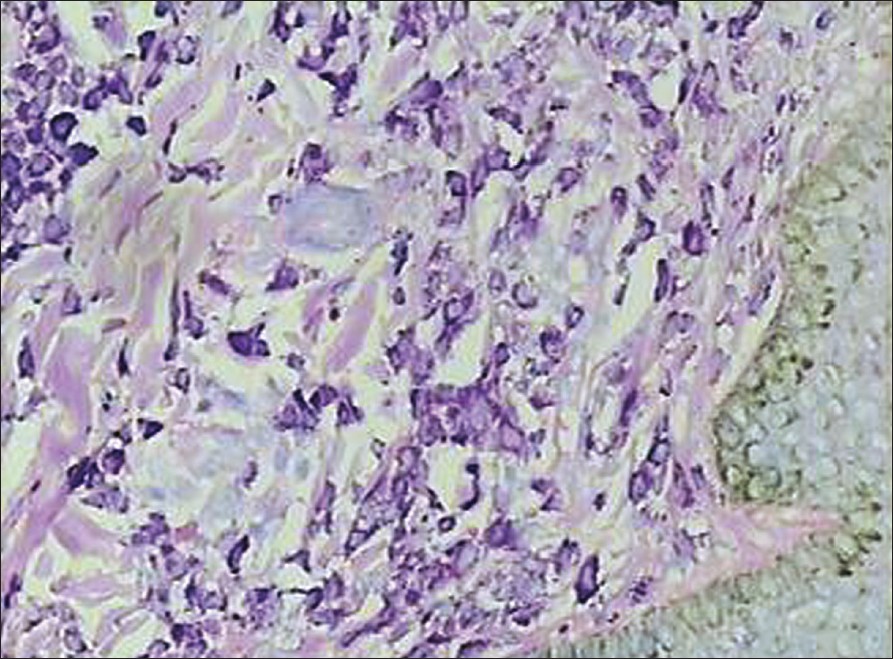 |
| Figure 3: Toluidine blue positive mast cells in the dermis (X400) |
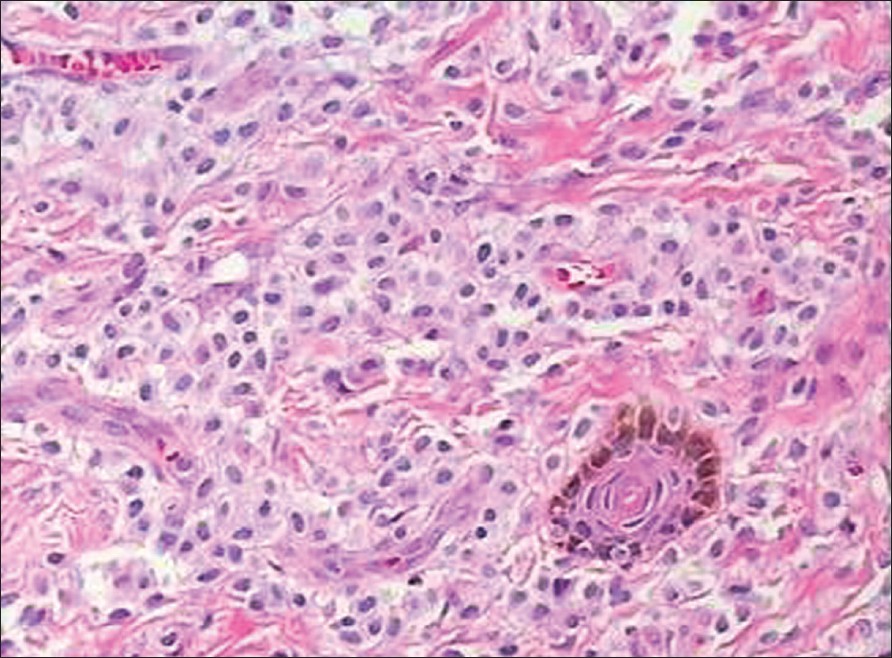 |
| Figure 2: Dense infiltrate of mast cells in the upper dermis (H and E, X400) |
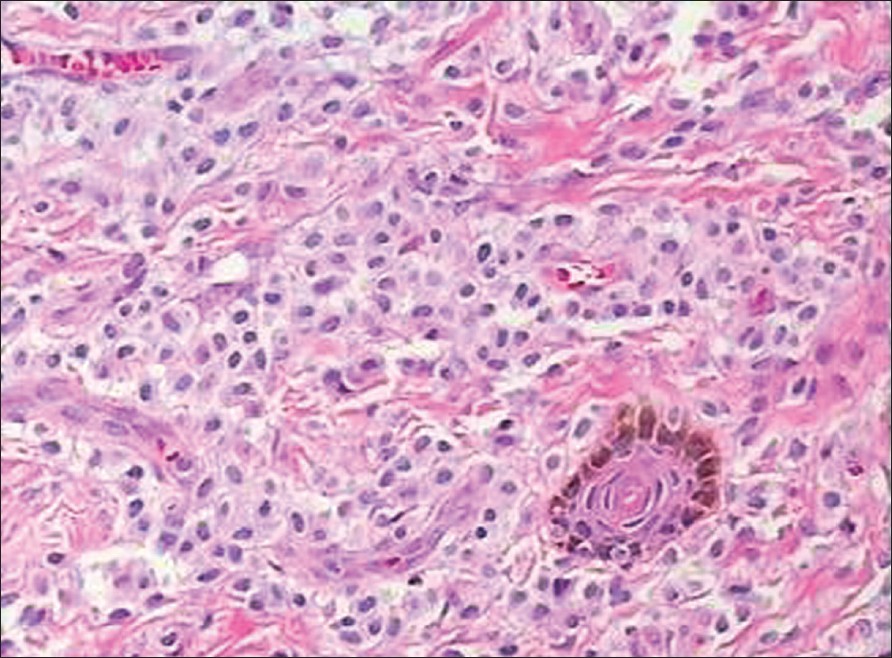 |
| Figure 2: Dense infiltrate of mast cells in the upper dermis (H and E, X400) |
 |
| Figure 1: Hypopigmented, round plaque with positive Darier�s sign on the nape of the neck in Case 1 |
 |
| Figure 1: Hypopigmented, round plaque with positive Darier�s sign on the nape of the neck in Case 1 |
Introduction
Mastocytosis is a disease characterized by the proliferation of mast cells in the skin, bone marrow, liver, spleen, lymph nodes or gastrointestinal tract. Cutaneous mastocytosis can present as urticaria pigmentosa, solitary mastocytoma (SM), diffuse mastocytosis and telangiectasia macularis eruptiva perstans. [1] Based on the clinical picture and course, mastocytosis may be divided into childhood onset (≤15 years) and adult onset (>16 years). Solitary mastocytoma occurs almost exclusively in the first 2 years of life as red, yellow, skin-colored or hyperpigmented solitary or multiple macules, plaques or nodules. [2],[3],[4] Herein we describe two patients with adult onset mastocytoma presenting as a solitary, hypopigmented plaque over the neck.
Case Reports
Case 1
A 24-year-old man presented with a plaque on the back of the neck of 5 years duration. He had intense itching and burning sensation after rubbing the lesion. There was history of allergic rhinitis since childhood. He had no episodes of flushing, headache, tachycardia, diarrhea or bone pain. On cutaneous examination, a single, hypopigmented, well-circumscribed, round plaque measuring 2.5 x 2.5 cm was observed on the nape of the neck. Stroking of lesion resulted in a wheal with flare (Darier′s sign) [Figure - 1]. There was no evidence of lymphadenopathy or hepatosplenomegaly. Histopathologic examination of a punch biopsy specimen revealed a dense mast cell infiltrate with scattered eosinophils involving the upper dermis and extending deeper in the peri-appendageal area [Figure - 2]. Toluidine blue stain demonstrated metachromatic purple granules in the cytoplasm [Figure - 3]. A diagnosis of solitary mastocytoma was made and after informed consent, the lesion was excised. There was no recurrence during one-year follow-up.
Case 2
A 30-year-old man came with a 10-year history of a plaque on the back of the neck. He reported itching in the lesion following scratching. He denied history of allergic rhinitis, bronchial asthma, flushing, headache, tachycardia, diarrhea or bone pain. Examination revealed a single, oval, 3 x 2.5 cm well-defined plaque with positive Darier′s sign on the nape of the neck [Figure - 4]. Systemic examination was within normal limits. Histopathologically, a dense, toluidine blue positive, mast cell infiltrate was observed in the upper dermis. The patient refused excision of the solitary mastocytoma. He was treated with two injections of intralesional triamcinolone acetonide (20 mg/ml) administered at the interval of three weeks. There was reduction in the pruritus with no change in the size of the lesion and Darier′s sign remained positive. Subsequently, he was lost to follow up.
Discussion
The cutaneous form of solitary mastocytoma (SM) was first described by Nettleship in 1889. Since then, recognition of SM and mastocytosis has increased due to significant increase in the knowledge of these entities. [5] Solitary mastocytoma is defined by the presence of one to several lesions (commonly five separate lesions). [2] Stroking of lesional skin usually provokes a whealing response (Darier′s sign) or blistering reaction (usually in children less than 3 years old). [3] Solitary mastocytoma is rarely found in adults. In one large series of 112 patients, SM developed mostly within the first month of life. [6] In a recent series of 101 patients documented by Middelkamp Hup et al., over an 18-year period, only one patient with adult onset SM was documented [2] . The symptoms are due to local and systemic release of histamine and other mast cell mediators like leukotrienes, prostaglandins and platelet activating factor. [5] These include pruritus (of varying intensity and severity), flushing, gastrointestinal complaints (nausea, colicky pain, diarrhea) and headaches. Rarely, gastrointestinal bleed, asthma and hypotension may occur. Malignant change has been reported with urticaria pigmentosa but not with SM. [3]
Mastocytosis can occur in sporadic and familial forms. [5] The exact etiology for proliferation of mast cells is unknown. Various postulates include C-kit receptor mutation, excessive production of C-kit ligand or increased production of soluble form of mast cell growth factor (MGF). [7] There are indications that mutation in C-kit receptor of which MGF is a ligand may be responsible for chronic course in adults. [8] The lesions of mastocytosis are often hyperpigmented due to overproduction of melanin. It has been proposed that this is due to MGF-induced stimulation of both mast cells and melanocytes. It is pertinent to note that both our patients had hypopigmented plaques, which is an atypical presentation. The usual differential diagnoses of SM include melanocytic nevi, xanthoma and xanthogranuloma. [9] In adults, leukemia cutis may also be considered. [10] Further, Pascual et al. reported a patient with a longstanding solitary plaque of telangiectasia macularis eruptiva perstans associated with renal carcinoma. This minimally raised lesion had significant overlying telangiectasias. [11] In our patient with hypopigmented SM, additionally leprosy and hypopigmented sarcoid were also ruled out.
It is possible that there is a relationship between SM and asthma. A higher personal or family incidence of allergic rhinitis or asthma was noted in children with SM. [6] Precipitation of acute asthmatic attack has been documented following mechanical stimulation of SM lesion. Degranulation of mast cells and release of mediators may play a role in its causation. [12] Case 1 had longstanding history of allergic rhinitis.
As children typically have complete involution of lesions by adulthood, treatment of SM has mostly been palliative in the form of H 1 and H 2 antihistaminics, cromolyn sodium, avoidance of triggering factors such as friction, ingestion of alcohol, NSAIDs or temperature changes. [4],[12],[13] Other modalities tried include topical and intralesional corticosteroids and hydrocolloid dressings. [3],[4] Surgical excision of SM as was done in Case 1 remains a rapid, simple and effective treatment. [12] Although Case 2 had symptomatic relief, no improvement in the lesion was noted with two injections of triamcinolone acetonide. This is in variance with the infant reported by Kang et al, who developed negative Darier′s sign, flattening of lesion following three injections of triamcinolone acetonide, given at monthly intervals. [4]
In the literature adult onset SM has been documented to have a less favorable resolution rate as compared to childhood onset. In addition, resolution is usually expected in up to 10 years, which would be unacceptable to symptomatic patients. [2] Thus, in case of single or a few, symptomatic lesions, surgical excision can be tried as first-line therapy.
| 1. |
Poulton JK, Kauffman CL, Lutz LL, Sina B. Solitary mastocytoma arising at a hepatitis B vaccination site. Cutis 1999;63:37-40.
[Google Scholar]
|
| 2. |
Middelkamp Hup MA, Heide R, Tank B, Mulder PG oranje AP. Comparison of mastocytosis with onset in children and adults. J Eur Acad Dermatol Venereol 2002;16:115-20.
[Google Scholar]
|
| 3. |
Yung A. Flushing due to solitary cutaneous mastocytoma can be prevented by hydrocolloid dressings. Pediatr Dermatol 2004;21:262-4.
[Google Scholar]
|
| 4. |
Kang NG, Kim TH. Solitary mastocytoma improved by intralesional injections of steroid. J Dermatol 2002;29:536-8.
[Google Scholar]
|
| 5. |
Kacker A, Huo J, Huang R, Hoda RS. Solitary mastocytoma in an infant: Case report with review of literature. Int J Pediatr Otorhinolaryngol 2000;52:93-5.
[Google Scholar]
|
| 6. |
Caplan RM. The natural course of urticaria pigmentosa: Analysis and follow-up of 112 cases. Arch Dermatol 1963;87:146-57.
[Google Scholar]
|
| 7. |
Kitamura Y, Tsujimura T, Jippo T, Kasugai T, Kanakura Y. Regulation of development, survival and neoplastic growth of mast cells through the c-kit receptor. Int Arch Allergy Immunol 1995;107:54-6.
[Google Scholar]
|
| 8. |
Longley J. Is mastocytosis a mast cell neoplasia or a reactive hyperplasia? Clues from the study of mast cell growth factor. Ann Med 1994;26:115-6.
[Google Scholar]
|
| 9. |
Thappa DM, Jeevankumar B. Solitary mastocytoma. Indian Pediatr 2005;42:390.
[Google Scholar]
|
| 10. |
Ashinoff R, Soter NA, Freedberg IM. Solitary mastocytoma in an adult: Treatment by excision. J Dermatol Surg Oncol 1993;19:487-8.
[Google Scholar]
|
| 11. |
Pascual JC, Banuls J, Albares MP, Vergara G, Belinchon I, Silvestre JF, et al. Presentation of telangiectasia macularis eruptiva perstans as a long-standing solitary plaque associated with renal carcinoma. J Cutan Med Surg 2003;7:399-402.
[Google Scholar]
|
| 12. |
Chang IJ, Yang CY, Sung FY, Ng KY. A red-brown plaque on the nape: Solitary mastocytoma. Arch Dermatol 2004;140:1275-80.
[Google Scholar]
|
| 13. |
Marone G, Genovese A. Biology, diagnosis and therapy of mastocytosis. In : Marone G, editor. Human Basophils and Mast cells: Clinical Aspects, vol. 62. Basel: Karger; 1995. p. 1-21.
[Google Scholar]
|
Fulltext Views
3,698
PDF downloads
1,939





