Translate this page into:
Adverse cutaneous events after laser epilation in patients with photodermatosis
Correspondence Address:
Blanca Ferrer Guillén
Department of Dermatology, University General Hospital of Valencia, Tres Cruces 2, Valencia 46014
Spain
| How to cite this article: Sánchez LC, Guillén BF, Sánchez Carazo JL, Ferriols AP. Adverse cutaneous events after laser epilation in patients with photodermatosis. Indian J Dermatol Venereol Leprol 2018;84:718-720 |
Sir,
We report the first two cases, till now, of primary cutaneous mucinosis and leukocytoclastic vasculitis, following laser epilation in patients with photodermatosis.
Laser epilation is an effective and safe hair removal method, which is not devoid of adverse effects, most of which are mild and transient and may include hypopigmentation or hyperpigmentation, perifollicular edema, erythema or crusting and paradoxical hypertrichosis.[1],[2],[3]
The first patient was a 55-year-old woman with a stinging rash over both legs, which had started one hour after her second session of laser epilation, and lasted more than a week. During the first session, she experienced a similar rash which resolved spontaneously. Laser epilation was performed with alexandrite laser (λ 755 nm) using a cooling gel and moisturizer. The patient had a history of erythematous to violaceous papules on both her legs, which appeared with the first solar exposure during the summer 3 years ago. The lesions lasted for more than a week, suggesting a diagnosis of polymorphous light eruptions. However, she had not been previously diagnosed, as she had never consulted about the condition.
Laboratory tests showed a total serum IgEof 144 KU/L. Patch tests with the standard GEIDAC series (Spanish contact dermatitis and skin allergy research group) and photopatch tests with the European standard series, were both negative. The open test with cooling gel and the moisturizer was also negative. Phototesting on the patient's back showed a minimal erythema dose (MED) of 60 mJ/cm2, (normal according to her phototype IV) and a negative reaction to UVA. Thereafter, we performed another phototeston the right thigh where the rash had appeared. We observed an anomalous response to UVA with 15 J/cm2 and a minimal erythema dose of 45 mJ/cm2, which are nonsignificant variations in the lower limb, within the same individual.
Subsequently, the patient was exposed to alexandrite laser in a small area in the anterior thigh, and after one hour she developed erythematous, edematous plaques limited to the exposed area [Figure - 1]. Given the background, a polymorphous light eruption induced by laser was suspected and a punch biopsy was obtained, revealing a perivascular infiltrate - predominantly lymphocytic and a bluish interstitial and perifollicular deposit that stained with colloidal iron, corresponding to mucin [Figure - 2]. Immunofluorescence was negative. The diagnosis of alexandrite laser-induced localized primary cutaneous mucinosis was made and laser was not performed again. We hypothesize that the reason for the accumulation of mucin is an inflammatory reaction induced by an unknown cutaneous stimulus leading to upregulation of its synthesis.
 |
| Figure 1: Erythematous papules that converge to form erythematousedematous plaques limited to the exposed area to Alexandrite laser |
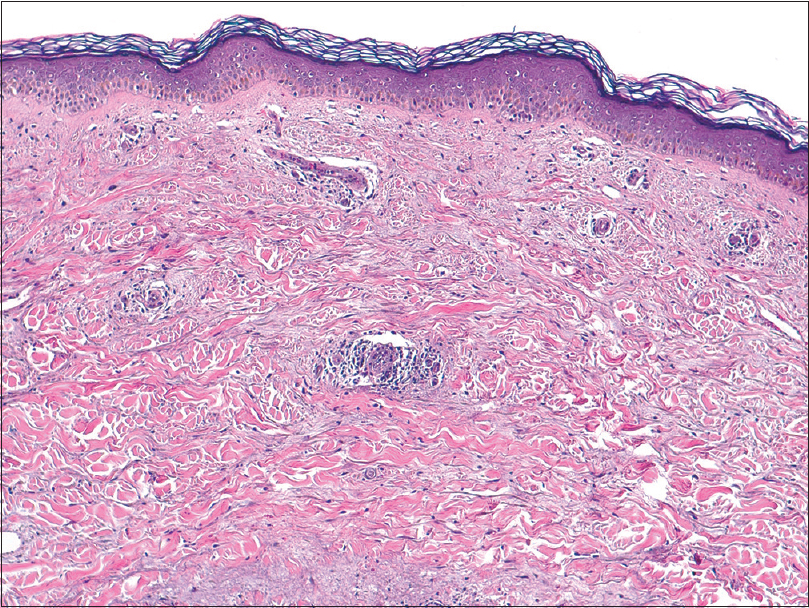 |
| Figure 2: Superficial and deep perivascular infiltrate predominantly lymphocytic and the presence of a bluish interstitial and perifollicular deposit corresponding to mucin (Hematoxylin and eosin, ×40) |
The second patient was a 44-year-old woman presenting with erythematous to purpuric macules in both legs, one hour after her eighth laser epilation session with a diode laser (λ 810 nm). The epilation began on the right leg, and since she felt a burning sensation during the procedure, the intensity was decreased in the contralateral limb [Figure - 3]. She had a previous history of systemic lupus erythematous with proven glomerular involvement.
 |
| Figure 3: Erythematous-purpuric macules in both legs limited to the exposed area to diode laser. Fewer lesions in the left leg due to decrease in intensity |
We performed a punch biopsy, revealing perivascular dermatitis with extravasation of red blood cells, areas of leukocytoclasia and hyalinization of the vessel wall [Figure - 4]. The patient declined photobiological study. The diagnosis of leukocytoclastic vasculitis induced by diode laser was made. The lesions disappeared after one week of treatment with topical methylprednisolone. Subsequently, another laser session was performed in a different area with lower intensity, without lesions.
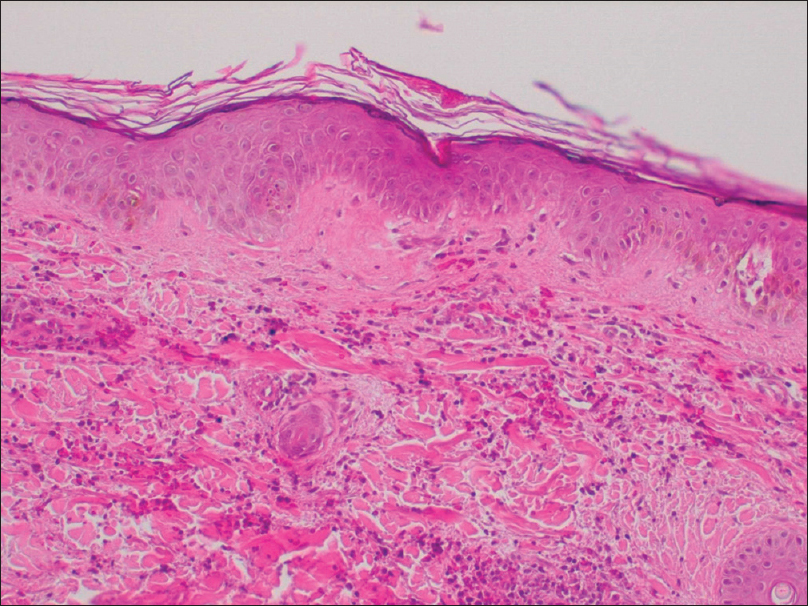 |
| Figure 4: Superficial and deep perivascular dermatitis with extravasation of red blood cells, leukocytoclasia and hyalinization of the vessel walls (Hematoxylin and eosin, ×100) |
One case of urticarial vasculitis induced by diode laser has been reported by Moreno-Arias after the second laser session.[4] Urticariform reactions of immediate onset after laser hair removal are frequent and correspond to dermatographic urticaria. However, urticariform reactions with a delayed onset and longer duration have been reported. Bernstein described four patients with clinical urticaria, three after alexandrite laser and one after Nd: YAG lasering.[5] Landa collected 36 patients with a similar clinical presentation, but of delayed onset, most of whom presented with lesions in the first session itself.[6] Biopsy in three cases was consistent with the diagnosis of urticaria. Landa points out that the etiology may be related to an antigen in the hair shaft or follicle itself, which is supported by the fact that, as the amount of antigen decreases, the lesions decrease.[6] This does not seem to occur in our second patient, who developed vasculitis after eight sessions when the number of follicles in the treated area was lower. In that case, laser intensity was crucial as the decrease in the contralateral leg caused fewer lesions; however, it remains unclear why lesions did not recur on subsequent sessions.
It is, thus, advisable to perform a test before laser epilation in a small area with immediate reading and after 48 hours, as late reactions have been reported in patients undergoing laser hair removal, especially those with a history of photodermatosis.[6]
The wavelength of the devices in laser epilation should not be responsible for the cutaneous reactions in patients with photodermatosis, as the use of photoepilation is widespread and there is limited literature on it.
The limitations of this report are the low frequency of these reactions and the lack of reports in published literature, which are essential to clarify their etiology.
It is important to be aware of these infrequent reactions and be cautious with patients with photodermatoses. More data are needed to elucidate their pathogenesis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Goldberg DJ, editor. Laser Dermatology: Pearls and Problems. 2nd ed. New York; Springer Heidelberg 2013.
[Google Scholar]
|
| 2. |
Lou WW, Quintana AT, Geronemus RG, Grossman MC. Prospective study of hair reduction by diode laser (800 nm) with long-term follow-up. Dermatol Surg2000;26:428-32.
[Google Scholar]
|
| 3. |
Moreno-Arias G, Castelo-Branco C, Ferrando J. Paradoxical effect after IPL photoepilation. Dermatol Surg2002;28:1013-6.
[Google Scholar]
|
| 4. |
Moreno-Arias GA, Tiffon T, Marti T, Camps-Fresneda A. Urticaria vasculitis induced by diode laser photo-epilation. Dermatol Surg2000;26:1082-3.
[Google Scholar]
|
| 5. |
Bernstein EF. Severe urticaria after laser treatment for hair reduction. Dermatol Surg2010;36:147-51.
[Google Scholar]
|
| 6. |
Landa N, Corrons N, Zabalza I, Azpiazu JL. Urticaria induced by laser epilation: A clinical and histopathological study with extended follow-up in 36 patients. Lasers Surg Med 2012;44:384-9.
[Google Scholar]
|
Fulltext Views
9,960
PDF downloads
1,202





