Translate this page into:
Aleukemic leukemia cutis
Correspondence Address:
Vishwanath Vishalakshi
102, Eden-2, Hiranandani Estate, Patlipada, Off Ghodbandar Road, Thane (W) - 400 607
India
| How to cite this article: Vishalakshi V, Torsekar R G, Shinde S. Aleukemic leukemia cutis. Indian J Dermatol Venereol Leprol 2007;73:109-111 |
Abstract
Aleukemic leukemia cutis has always been a dermatological curiosity. It is a rare condition characterized by the infiltration of skin by leukemic cells before their appearance in the peripheral blood or bone marrow. A 20 year old man had presented with nodular swelling on the scalp of 6 months duration along with cervical lymphadenopathy. Biopsy and immunohistochemistry revealed myeloid sarcoma. The initial presentation was aleukemic and repeated peripheral blood counts and marrow examinations were normal. However, the outcome was fatal within 3 months of diagnosis of cutaneous lesions.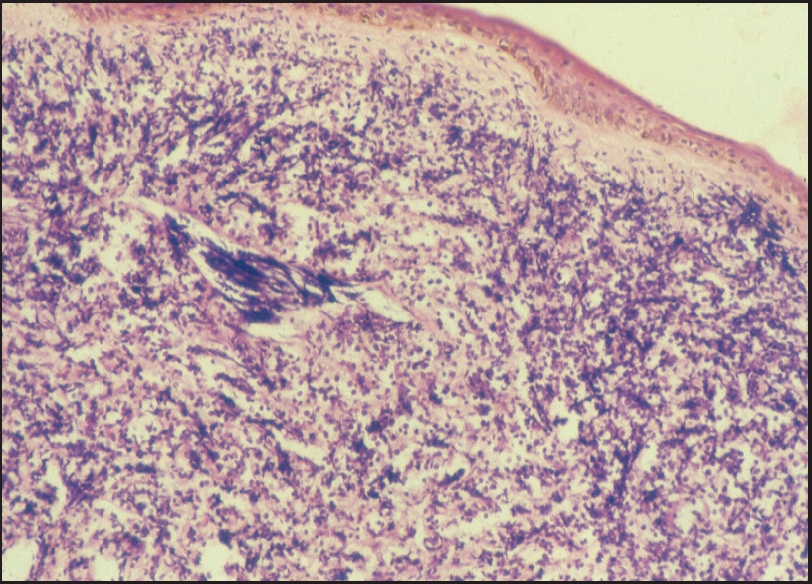 |
| Atrophic epidermis, grenz zone and diffuse infi ltrate of small round cells (H and E, x100) |
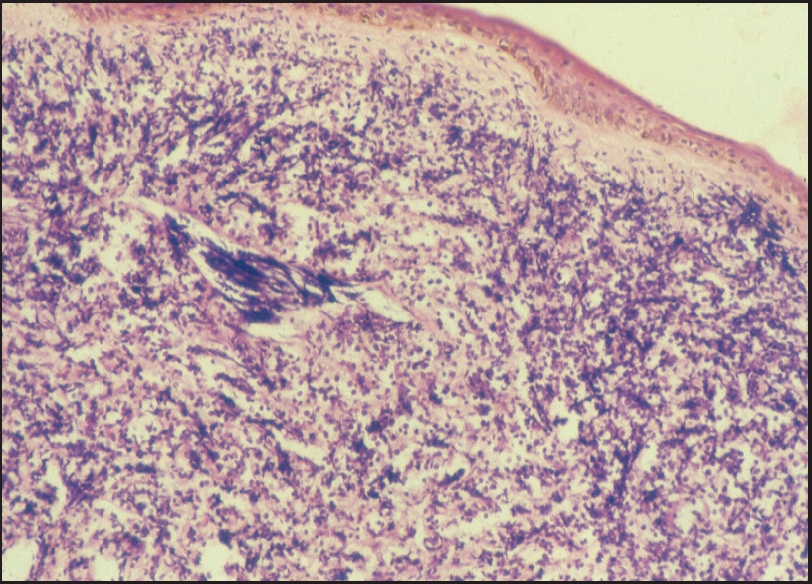 |
| Atrophic epidermis, grenz zone and diffuse infi ltrate of small round cells (H and E, x100) |
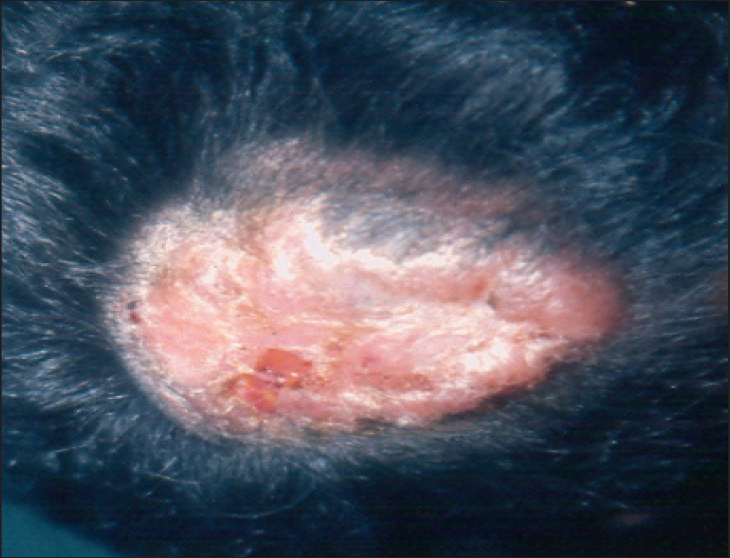 |
| Nodular swelling on scalp |
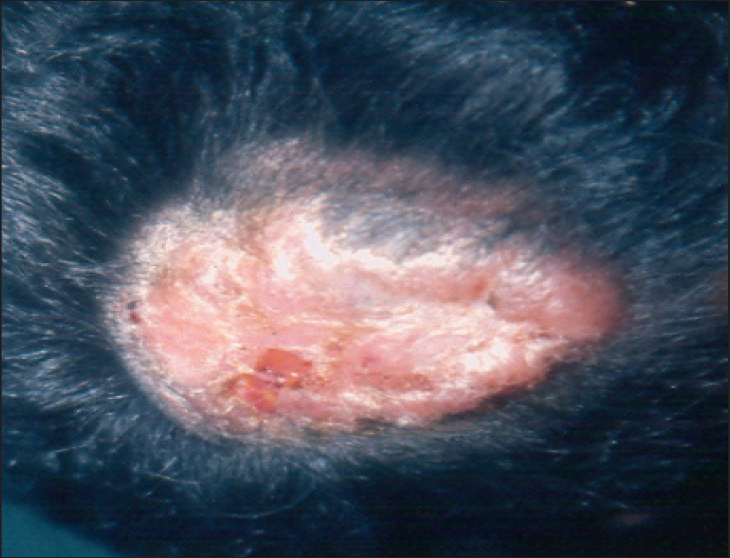 |
| Nodular swelling on scalp |
Introduction
Cutaneous lesions of leukemia can be classified into two groups, leukemids or non-specific lesions and true leukemic infiltrations or specific lesions (leukemia cutis). Leukemia cutis (LC) is frequently seen in acute myelogenous leukemia (AML) and its appearance with respect to bone marrow involvement is variable. Aleukemic presentations have been reported where the first manifestation of leukemia was in skin with a normal peripheral blood count. [1],[2] We report a case of localized myeloid sarcoma with an initial aleukemic presentation in a young adult male.
Case report
A 22 year old male presented with asymptomatic swelling on the scalp of 6 months duration. There was no history of trauma, weight loss, bleeding or any systemic illness in the past. Local examination revealed a hard nodular swelling 10 x 8 x 2 cm on the vertex [Figure - 1] along with cervical lymphadenopathy. The rest of the systemic examination was normal. A clinical differential diagnosis of cylindroma, lymphoma and cutaneous metastasis was considered.
His hemoglobin was 11.5 g%; total and differential white blood counts were normal (TC-8500, N-61, L-39). Erythrocyte sedimentation rate (ESR) was 35 mm at the end of 1 hour. Liver and renal function tests, X-ray chest / skull and abdominal sonography did not reveal any abnormality. Enzyme-linked immunosrbent assay (ELISA) for human immunodeficiency virus (HIV) was negative. Skin biopsy showed an atrophic epidermis, Grenz zone and a diffuse infiltrate of small round cells in the dermis [Figure - 2]. These cells were uniformly stained with a slight rim of cytoplasm, large nucleus, fine chromatin and one to two nucleoli. A differential diagnosis of myeloid sarcoma or malignant lymphoma was considered. However, a bone marrow biopsy done to rule out an underlying hemopoietic malignancy was normal. The patient was referred to Tata Memorial Hospital for further management. A diagnosis of myeloid sarcoma was favored as against lymphoma due to absence of cleaved nuclei and follicular pattern in the infiltrate. Immunohistochemistry was done to look for myeloid infiltration in the deposits and it showed strong CD43 and focal CD68 positivity. Similar findings were obtained from lymph node biopsy suggesting the presence of acute myelomonocytic leukemia. However, repeated peripheral blood counts and bone marrow examinations were normal. It was thus an aleukemic presentation of leukemia cutis. Excision and radiotherapy were planned. However, the patient had a sudden bleeding episode with a fatal outcome that occurred within 3 months of the diagnosis of cutaneous lesions.
Discussion
LC is a rare condition of poor prognostic significance. It can manifest in a variety of leukemia subtypes, hence the exact overall incidence is unclear. In most cases of LC, systemic disease precedes it; only 7% of cases are aleukemic and 13% of LC cases are seen in AML. [3] In a retrospective study, Baer et al . reviewed 18 cases of AML with LC, wherein the skin manifestations were seen either at diagnosis or during relapse. [4] Only 2 patients had LC antedating bone-marrow involvement.
Aleukemic LC has been termed as primary extramedullary leukemia. [3] Detection of extramedullary sites is important for adequate treatment and prevention of relapses in leukemias. Compared to other occult extramedullary sites, LC can be easily documented by biopsy. With the advent of immunologic, cytogenetic and molecular biologic techniques, it is easier to identify and confirm the cell lineage. Hence skin biopsy may be helpful in detecting the leukemia and facilitate further workup especially in cases of aleukemic leukemia, as was seen in our case. The clinical features of LC include macules, papules, plaques, nodules, bullae, purpura, ulcers and exanthematous eruptions. A specific cutaneous manifestation is the appearance of single or multiple nodular tumor masses called granulocytic sarcoma which was seen in our patient. [5]
Granulocytic sarcoma is an uncommon localized tumor composed of immature cells of granulocytic series. It was initially described in 1823 and its association with leukemia was recognized in 1893. It was earlier termed chloroma due to the green appearance resulting from the presence of myeloperoxidase in the immature myeloid cells. The term granulocytic sarcoma was coined in 1966 by Rappaport following the description of lesions which were not green (exposure to air or fixation in formalin causing loss of color). The recent terminology is myeloid sarcoma since not all myeloid leukemias are derived from granulocytes. [6] Other names include extramedullary myeloid tumor, myeloblastoma or specific myelogenous infiltrations. It occurs in different clinical settings-as a harbinger of AML in nonleukemic patients; in association with myelodysplastic / myeloproliferative disorders with impending blast crisis; in association with AML. Myeloid sarcoma is frequently associated with the 8; 21 translocation in AML and has a less favorable prognosis. [7] The common sites of predilection are bone, periosteum, soft tissues of head and neck orbit, lymph nodes and skin. Bilateral presentation in the breast has also been documented and is due to the tropism of circulating tumor cells for breast tissue. [8] Myeloid sarcoma of prostate causing urinary obstruction in an eight year old child has been reported as an unusual presentation of AML. [6] Clinically, myeloid sarcoma involving skin presents as firm nodular masses of variable sizes which do not ulcerate. Microscopically, it is classified into blastic, immature and differentiated type and closely mimics malignant lymphoma both on cytology and tissue sections. Histological differentiation from lymphoma is possible on haematoxylin and eosin (H and E)-stained sections by a trained pathologist due to infiltrative pattern of the cells and characteristic multilobated nuclear configuration in myeloid sarcoma as compared to cleaved nuclear pattern in lymphoma. [9]
Myeloperoxidase, naphthol ASD-chloroacetate esterase staining done on cytology smears aid in confirming the diagnosis, while on tissue sections chloroacetate esterase, anti-lysozyme, anti-myeloperoxidase, anti-CD68 and anti-CD43 staining help in demonstrating the myeloid morphology. [8],[10] Other markers include muramidase, alpha-1 anti trypsin, cathepsin G and leukocyte elastase. [10]
In cases of aleukemic leukemia cutis, development of myeloid sarcoma preceding AML in peripheral blood may be due to the proliferation of myeloblasts in the spleen or lymph nodes and unexplained failure of release of myeloblasts from the lymph node. [10] A similar mechanism could be proposed for initial aleukemic presentation with lymphadenopathy seen in our patient. Diagnosis of myeloid sarcoma in non-leukemic patients is usually associated with poor prognosis since acute leukemia can develop within a matter of months. In a study by Meis et al ., out of 16 cases, 25% of patients did not develop leukemia during 3.5 to 16 years of follow-up; however prognostic factors could not be identified. [9] Our patient had a fatal outcome within 3 months of diagnosis probably due to a blast crisis. Early diagnosis of these cases aids in starting early treatment in the form of local radiotherapy or chemotherapy, but a watch has to be kept for development of AML. This case has been reported for its rarity and to emphasize the role of a dermatopathologist in early diagnosis.
Acknowledgment
We are thankful to Dr. N. A. Jambhekar, Department of Pathology, Tata Memorial Hospital for the immunohistochemical studies.
| 1. |
Yoder FW, Schuen RL. Aleukemic leukemia cutis. Arch Dermatol 1976;112:367-9.
[Google Scholar]
|
| 2. |
Hansen RM, Barnett J, Hanson G, Klehm D, Schneider T, Ash R. Aleukemic leukemia cutis. Arch Dermatol 1986;122:812-4.
[Google Scholar]
|
| 3. |
Rencic A, Ramnarayanan J. Leukemia Cutis. eMedicine Dermatology. [Last updated on 2005 Jun 7 th ]. Available from: http://www.emedicine.com/derm/topic924.htm. [Last accessed on 2006 Aug 24 th ].
[Google Scholar]
|
| 4. |
Baer MR, Barcos M, Farrell H, Raza A, Preisler HD. Acute myelogenous leukemia with leukemia cutis. Eighteen cases seen between 1969 and 1986. Cancer 1989;63:2192-200.
[Google Scholar]
|
| 5. |
LeBoit PE, McCmont TH. Cutaneous Lymphomas and Leukemias. In: Elder D, Elenitsas R, Jaworsky C, Johnson B Jr, editors. Lever's histopathology of the skin. 8 th ed. Lippincott-Raven: Philadelphia; 1997. p. 805-44.
th ed. Lippincott-Raven: Philadelphia; 1997. p. 805-44.'>[Google Scholar]
|
| 6. |
Joshi A, Patel A, Patel K, Shah S, Shah P, Shukla SN, et al . Myeloid sarcoma of prostate with urinary obstruction: An unusual presentation of Acute Myelogenous Leukemia in a child. Indian J Med Paediatr Oncol 2005;26:40-2.
[Google Scholar]
|
| 7. |
Tallman MS, Hakimian D, Shaw JM, Lissner GS, Russell EJ, Variakojis D. Granulocytic sarcoma is associated with the 8;21 translocation in Acute Myeloid Leukemia. J Clin Oncol 1993;11:690-7.
[Google Scholar]
|
| 8. |
Kwatra KS, Prabhakar BR, Arora Y. Bilateral granulocytic sarcoma (chloroma) of the breast in CML in blast crisis: A case report. Indian J Pathol Microbiol 2004;47:66-8.
[Google Scholar]
|
| 9. |
Meis JM, Butler JJ, Osborne BM, Manning JT. Granulocytic sarcoma in nonleukemic patients. Cancer 1986;58:2697-709.
[Google Scholar]
|
| 10. |
Muller S, Sangster G, Crocker J, Nar P, Burnett D, Brown G, et al . An immunohistochemical and clinicopathological study of granulocytic sarcoma (chloroma). Hematol Oncol 1986;4:101-12.
[Google Scholar]
|
Fulltext Views
3,912
PDF downloads
1,837





