Translate this page into:
Allopurinol-induced drug reaction with eosinophilia and systemic symptoms syndrome associated with reactivation of Epstein–Barr virus leading to secondary hemophagocytic lymphohistiocytosis in an HLA-B*5801-negative patient
Corresponding author: Prof. Yang Xu, Department of Dermatology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China. cardioos@163.com
-
Received: ,
Accepted: ,
How to cite this article: Su T, Xiong W, Xu Y, Lu Y. Allopurinol-induced drug reaction with eosinophilia and systemic symptoms syndrome associated with reactivation of Epstein–Barr virus leading to secondary hemophagocytic lymphohistiocytosis in an HLA-B*5801-negative patient. Indian J Dermatol Venereol Leprol 2021;87:545-8.
Sir,
Drug reaction with eosinophilia and systemic symptoms syndrome (DRESS), also known as drug-induced hypersensitivity syndrome, is a severe, life-threatening cutaneous drug-induced eruption characterized by long incubation periods, acute-onset rash, hematological abnormalities and solid organ damage.1 Rarely, it progresses to hemophagocytic lymphohistiocytosis, a severe hyperinflammatory syndrome induced by activated macrophages and cytotoxic T cells.2 We report a case of allopurinol-induced DRESS complicated by hemophagocytic lymphohistiocytosis associated with reactivation of Epstein–Barr virus in a patient with negative HLA-B*5801 allele.
A 69-year-old Chinese man with hypertension, renal stones and chronic renal dysfunction was started on allopurinol (0.3 g/day) for hyperuricemia. After 12 days of starting the treatment, he developed a generalized rash, fever (39.5℃) and anuria following which he was admitted to the dermatology ward. Physical examination revealed diffuse erythema over the face and trunk and petechiae and ecchymoses on the lower limbs [Figures 1a and b]. Mild cervical lymphadenopathy was also present. The spleen was palpable which was confirmed on abdominal ultrasonography.
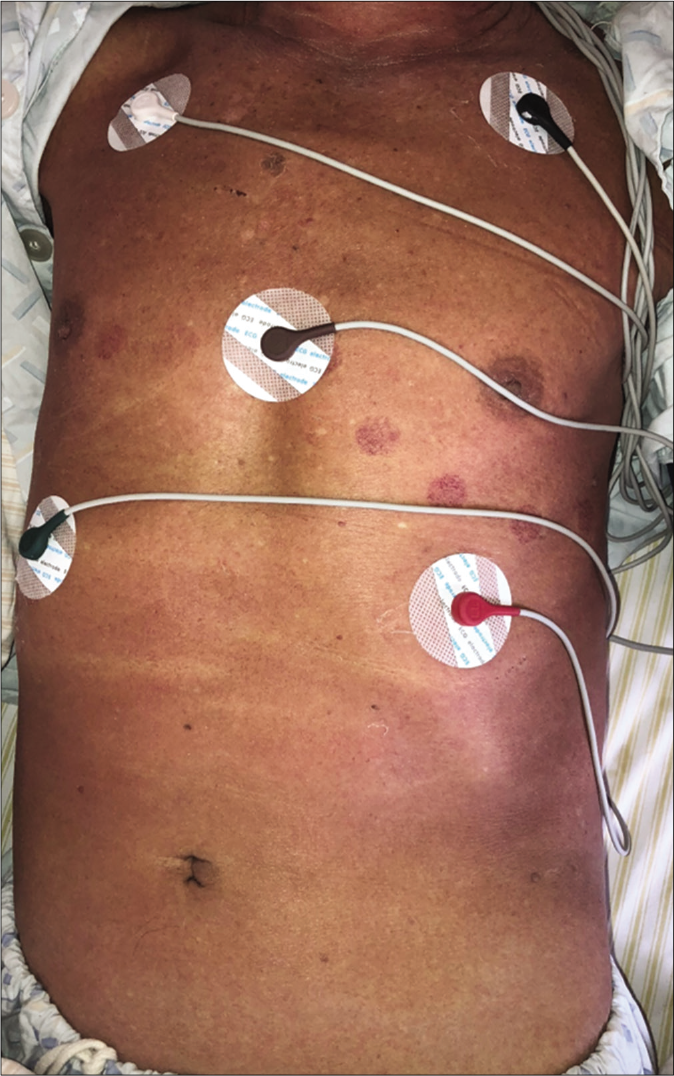
- Diffuse erythema over the trunk, on admission

- Diffuse petechia and ecchymosis on the lower limbs, on admission
Laboratory evaluation showed leukocytosis with eosinophilia (26%) with absolute eosinophil count of 5.86 × 109/L. Serum levels of lactate dehydrogenase, glutamic pyric transaminase, glutamic oxaloacetic transaminase, creatinine and uric acid showed marked elevation with a mild elevation of serum potassium (5.7 mmol/L with a normal range of 3.5–5.5 mmol/L). C-reactive protein was also elevated (47.17 mg/L with a normal range of <8 mg/L). Peripheral smear examination showed atypical lymphocytes. According to the RegiSCAR diagnostic criteria, a score of six was obtained which indicates a definite diagnosis of DRESS. Serology tests for hepatitis viruses, cytomegalovirus, human immunodeficiency virus and parvovirus B19 were found to be negative, but an increased serum DNA copy of Epstein– Barr virus was detected 19 days after the onset of symptoms (1.14 × 103 copies/mL; normal range, <5 × 102 copies/mL). In addition, both anti-Epstein–Barr virus nuclear antigen protein IgG and antiviral capsid antigen IgM in the serum were positive. Bone marrow aspiration revealed an increased number of eosinophils; however, the HLA-B*5801 allele was negative.
The patient was then treated with 20 g of intravenous immunoglobulin daily for five days and 80 mg/d of intravenous methylprednisolone, along with the correction of fluid and electrolyte imbalance. The clinical symptoms improved with this treatment [Figures 1c and 1d] but after seven days, there was a sudden onset of high-grade fever (40°C) accompanied by dyspnea. The laboratory tests showed a sudden decrease in total blood cell count (white cell count – 200/μL; platelet count – 26,000/μL and hemoglobin – 4.8 g/dL) [Figure 2] and an evident increase in serum ferritin (1310.9 μg/L; normal range, 23.9–336.2 μg/L) and soluble CD25 (soluble interleukin-2 receptor alpha, 33,081 ng/L; normal range, 0–2000 ng/ mL). Soluble CD25 is a marker for macrophage activation syndrome. Bone marrow biopsy showed an increased number of macrophages with prominent hemophagocytosis [Figure 3].

- Post-treatment improvement showing only scattered erythema and focal peeling over the trunk

- Post-treatment improvement showing only focal peeling of skin over the lower limbs
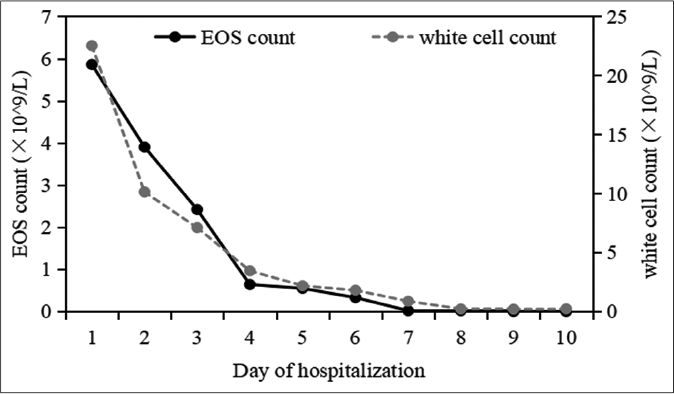
- Clinical parameter over time – EOS: Eosinophils
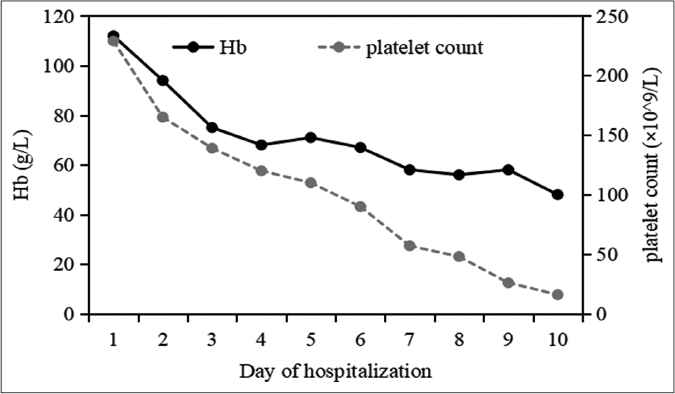
- Clinical parameter over time – Hb: Hemoglobin
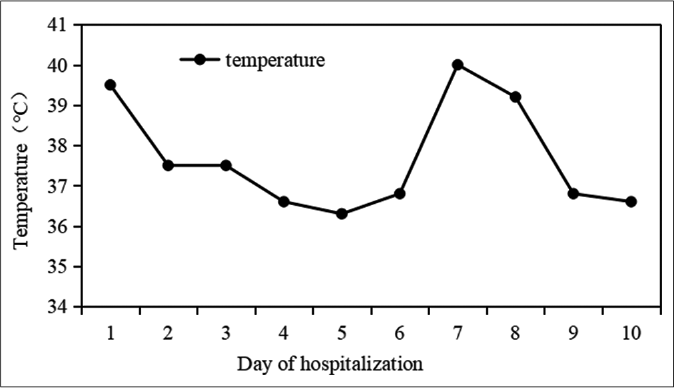
- Clinical parameter over time – Temperature
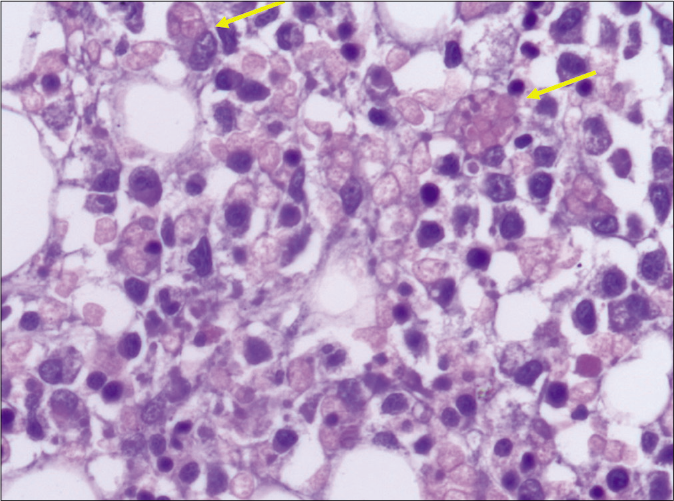
- Bone marrow biopsy smear demonstrating hemophagocytosis (hemophagocytes marked with arrows, H and E, ×400)
Finally, the patient was diagnosed with allopurinol-induced DRESS complicated with hemophagocytic lymphohistiocytosis. He was immediately transferred to the hematology department and started on the hemophagocytic lymphohistiocytosis – 2004 treatment regimen (dexamethasone, etoposide and ciclosporin); however, he died of acute respiratory failure ten days later.
DRESS is a severe type of cutaneous drug-induced eruption, and allopurinol is a commonly associated drug. The risk factors of DRESS can be broadly grouped into three categories: the length of time from the start of treatment, genetic factors and the factors that influence drug concentration.3 Although the HLA-B*58:01 allele has been reported to be associated with increased risk of developing allopurinol-induced cutaneous adverse reactions, other factors may also play an important role, including the concentration of drug, the use of diuretics and presence of renal dysfunction. These factors can prolong the half-life of allopurinol which causes the accumulation of allopurinol in the serum resulting in continuous hypersensitivity in the body, leading to multiple organ damage.3
Hemophagocytic lymphohistiocytosis is an aberrant hyperinflammatory hyperferritinemic immune response syndrome that is driven by T cells and is associated with a potentially fatal cytokine storm.2 Drug-induced hemophagocytic lymphohistiocytosis is relatively rare in the literature and most cases are believed to be due to the activation of Epstein–Barr virus or human herpesvirus-6. Virus reactivation has been detected in over 70% of patients with DRESS, but most of them do not develop hemophagocytic lymphohistiocytosis. Therefore, we suspected that the virus is not the main factor in inducing hemophagocytic lymphohistiocytosis but may have contributed to the final prognosis.4
Our literature search revealed only one case of allopurinol-induced DRESS complicated with hemophagocytic lymphohistiocytosis in which the viral markers were negative and the patient recovered with intravenous immunoglobulin treatment.5 To the best of our knowledge, ours is the first case of allopurinol-induced DRESS associated with hemophagocytic lymphohistiocytosis complicated with Epstein–Barr virus reactivation in China with negative HLAB*58:01 allele. As the patient already had an impaired renal function, the patient’s condition progressed to acute kidney failure which proved fatal despite prompt and adequate treatment. Increased awareness of association of DRESS with hemophagocytic lymphohistiocytosis and its diagnosis is crucial for early detection and treatment. It will be worthwhile to monitor Epstein–Barr virus levels and serial blood cell count in all patients with DRESS, especially those with renal disorders. Early intervention may result in a promising prognosis in patients with such complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This study was supported by the National Science Fund for Distinguished Young Scholars (Grant No. 81301384).
Conflicts of interest
There are no conflicts of interest.
References
- New insights into drug reaction with eosinophilia and systemic symptoms pathophysiology. Front Med (Lausanne). 2017;4:179.
- [CrossRef] [PubMed] [Google Scholar]
- Hemophagocytic lymphohistiocytosis: Clinical presentations and diagnosis. J Allergy Clin Immunol Pract. 2019;7:824-32.
- [CrossRef] [PubMed] [Google Scholar]
- Allopurinol hypersensitivity: Investigating the cause and minimizing the risk. Nat Rev Rheumatol. 2016;12:235-42.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis of a DRESS syndrome has been sufficiently established on the basis of typical clinical features and viral reactivations. Br J Dermatol. 2007;156:1083-4.
- [CrossRef] [PubMed] [Google Scholar]
- Allopurinol-induced DRESS complicated by hemophagocytic lymphohistiocytosis. Ann Dermatol Venereol. 2015;142:767-70.
- [CrossRef] [PubMed] [Google Scholar]





