Translate this page into:
Aminolevulinic acid photodynamic therapy for bowenoid papulosis
Correspondence Address:
Hong Fang
Department of Dermatology, The First Affiliated Hospital, College of Medicine, Zhejiang University, No. 79, Qingchun Road, Hangzhou, Zhejiang Province
People's Republic of China
| How to cite this article: Wu Yh, Qiao Jj, Bai J, Fang H. Aminolevulinic acid photodynamic therapy for bowenoid papulosis. Indian J Dermatol Venereol Leprol 2015;81:219-220 |
Sir,
Photodynamic therapy (PDT) is a new treatment based on a phototoxic reaction caused by a photosensitizer that is activated by light to form reactive oxygen species. [1] For treating skin diseases, photodynamic therapy is performed by using topical precursor molecules of the biosynthetic pathway of heme such as 5-aminolevulinic acid (ALA) or its methyl ester methyl aminolevulinate. In dermatology, this modality is used as a primary treatment for malignant and premalignant skin lesions, such as actinic keratosis, Bowen′s disease, and superficial squamous cell carcinoma. Topical photodynamic therapy has also effectively treated diseases caused by human papillomavirus (HPV) infection, including various warts and epidermodysplasia verruciformis. [1]
Bowenoid papulosis is an entity characterized by circumscribed, round, usually multiple red-brown papules. [2] Many reports demonstrate that this disease is caused by human papilloma virus infection. Thus it is potentially responsive to photodynamic therapy.
We report two patients of bowenoid papulosis who were successfully treated by photodynamic therapy.
Case 1 was a 45-year-old female, who presented with a 1-year history of multiple brown and flat papules in the perianal area [Figure - 1]a. Skin biopsy from one of the lesions revealed acanthosis with full-thickness epidermal dysplasia and atypical mitoses [Figure - 1]b. Polymerase chain reaction analysis of the specimen showed positivity for the high-risk HPV 16. The patient first received microwave therapy (local anesthesia with lidocaine, output power was 25 W) and followed by six cycles of topical photodynamic therapy. 20% aminolevulunic acid (118 mg in 0.5 ml sterile water for injection) was applied to the skin for a 3-h incubation. The light-emitting diode (LED) exposure duration was 20 min. The interval between two sessions was 1-2 weeks. The lesions disappeared [Figure - 1]c and human papilloma virus polymerase chain reaction was negative 1 month after the therapy. The patient was followed-up for 6 months and did not show any recurrence.
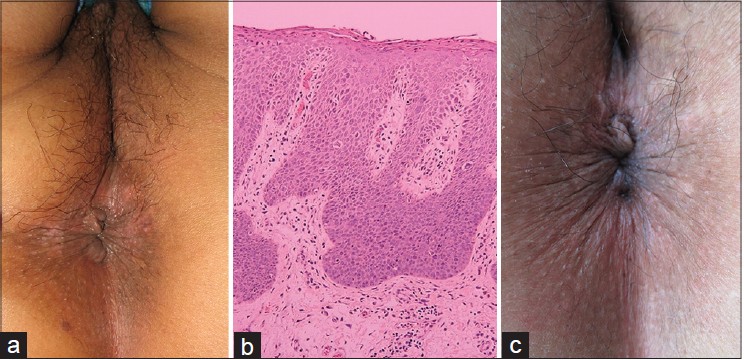 |
| Figure 1: Patient 1. (a) Multiple brown and flat papules involving the perianal area. (b) Acanthosis with full-thickness epidermal dysplasia, atypical mitoses. (H and E,×100) (c) One month after ALA-PDT therapy |
Case 2 was a 31-year-old female who presented with a 1-year history of vulvar lesions. She had a history of vulvar condyloma acuminata 13 years before and was in remission since then. There were some discrete brown and flat papules in the posterior commissure labiorum [Figure - 2]a. Skin biopsy revealed multiple mitoses and marked pleomorphism in keratinocytes in all the epidermal layers [Figure - 2]b. Polymerase chain reaction analysis of the lesion demonstrated the presence of high-risk HPV 16. We used CO 2 laser (local anesthesia with lidocaine, output power was 4 W) to destroy the lesions followed by four cycles of topical photodynamic therapy. At present, the patient has no recurrence after a 1-year follow-up period[Figure - 2]c.
 |
| Figure 2: Patient 2. (a) Lesions in commissura labiorum posterior. (b) Multiple mitoses and marked pleomorphism in keratinocytes in the epidermis. (H and E,×100). (c) After PDT therapy |
Treatment approaches for bowenoid papulosis include topical 5-fluorouracil cream, topical imiquimod cream, electrocoagulation, cryotherapy, laser ablation, and surgical excision. [2] Although photodynamic therapy is still a new modality, it may be one of the best options due to the combination of a high and sustained response rate, limited downtime for patients, and an excellent aesthetic outcome. [1] It has been reported that two patients with bowenoid papulosis improved after a single session of photodynamic therapy using a high-intensity light source. [2] Another report described partial improvement in a 65-year-old male after four treatment sessions. [3]
The major problem with this modality is pain during illumination. Pain usually disappears after stopping the illumination. [1] In comparison to conventional treatments, including cryotherapy, surgery, and electrocoagulation, this therapy shows great advantages including high efficacy and tolerability, excellent cosmetic results, and low risk of scarring. [3]
Both our patients received ablative therapies including microwave therapy and CO 2 laser, prior to photodynamic therapy. There are advantages of such combined therapy. Studies of condylomata acuminata have shown that photodynamic therapy is more effective when combined with cryotherapy or laser ablation. [4],[5] Firstly, conventional therapies for condylomata acuminata such as cryotherapy, CO 2 laser, and microwave therapy cannot destroy subclinical infected cells but can more easily destroy bulky lesions. [4],[5] In contrast, photodynamic therapy shows efficacy as a technique for the treatment of superficial lesions as well as latent infections, which may be due to its antiviral properties. [4] Secondly, previous studies indicate that it is an effective, safe, and non-invasive method compared with conventional therapies. [1],[4] In conclusion, combined therapy appears safer, more effective, and less painful. Intensified therapy may enable long-term maintenance of complete remission.
Although the current report shows that photodynamic therapy is beneficial for bowenoid papulosis, it was done for a limited number of patients. Further studies with larger sample size are needed to establish the clinical benefits and recurrence rate.
ACKNOWLEDGMENT
This work was supported by a CDA-FDZJ photodynamic therapy grant to JQ in 2010 and by The National Natural Science Foundation of China (No. 81271743).
| 1. |
Darlenski R, Fluhr JW. Photodynamic therapy in dermatology: Past, present, and future. J Biomed Opt 2013;18:061208.
[Google Scholar]
|
| 2. |
Yang CH, Lee JC, Chen CH, Hui CY, Hong HS, Kuo HW. Photodynamic therapy for bowenoid papulosis using a novel incoherent light-emitting diode device. Br J Dermatol 2003;149:1297-9.
[Google Scholar]
|
| 3. |
Calzavara-Pinton PG, Rossi MT, Sala R, Italian group for Photodynamic Therapy. A retrospective analysis of real-life practice of off-label photodynamic therapy using methyl aminolevulinate (MAL-PDT) in 20 Italian dermatology departments. Part 2: Oncologic and infectious indications. Photochem Photobiol Sci 2013;12:158-65.
[Google Scholar]
|
| 4. |
Mi X, Chai W, Zheng H, Zuo YG, Li J. A randomized clinical comparative study of cryotherapy plus photodynamic therapy vs. cryotherapy in the treatment of multiple condylomata acuminata. Photodermatol Photoimmunol Photomed 2011;27:176-80.
[Google Scholar]
|
| 5. |
Chen K, Chang BZ, Ju M, Zhang XH, Gu H. Comparative study of photodynamic therapy vs CO2 laser vaporization in treatment of condylomata acuminata: A randomized clinical trial. Br J Dermatol 2007;156:516-20.
[Google Scholar]
|
Fulltext Views
2,984
PDF downloads
1,742





