Translate this page into:
An atypical presentation of lupus vulgaris
Correspondence Address:
Rima Gammoudi
Department of Dermatology, Farhat Hached University Hospital, Avenue Ibn Jazzar, 4002 Sousse
Tunisia
| How to cite this article: Gammoudi R, Lahouel M, Saidi W, Denguezli M. An atypical presentation of lupus vulgaris. Indian J Dermatol Venereol Leprol 2020;86:573-576 |
Sir,
Although lupus vulgaris is one of the most common forms of cutaneous tuberculosis, the condition often remains undiagnosed and treated inappropriately due to its variable clinical presentation and paucibacillary nature. An atypical case of disseminated lupus vulgaris in an immunocompetent woman is presented. Salient recount of the natural history, clinical connotation, histopathological features and the relevant laboratory details are described.
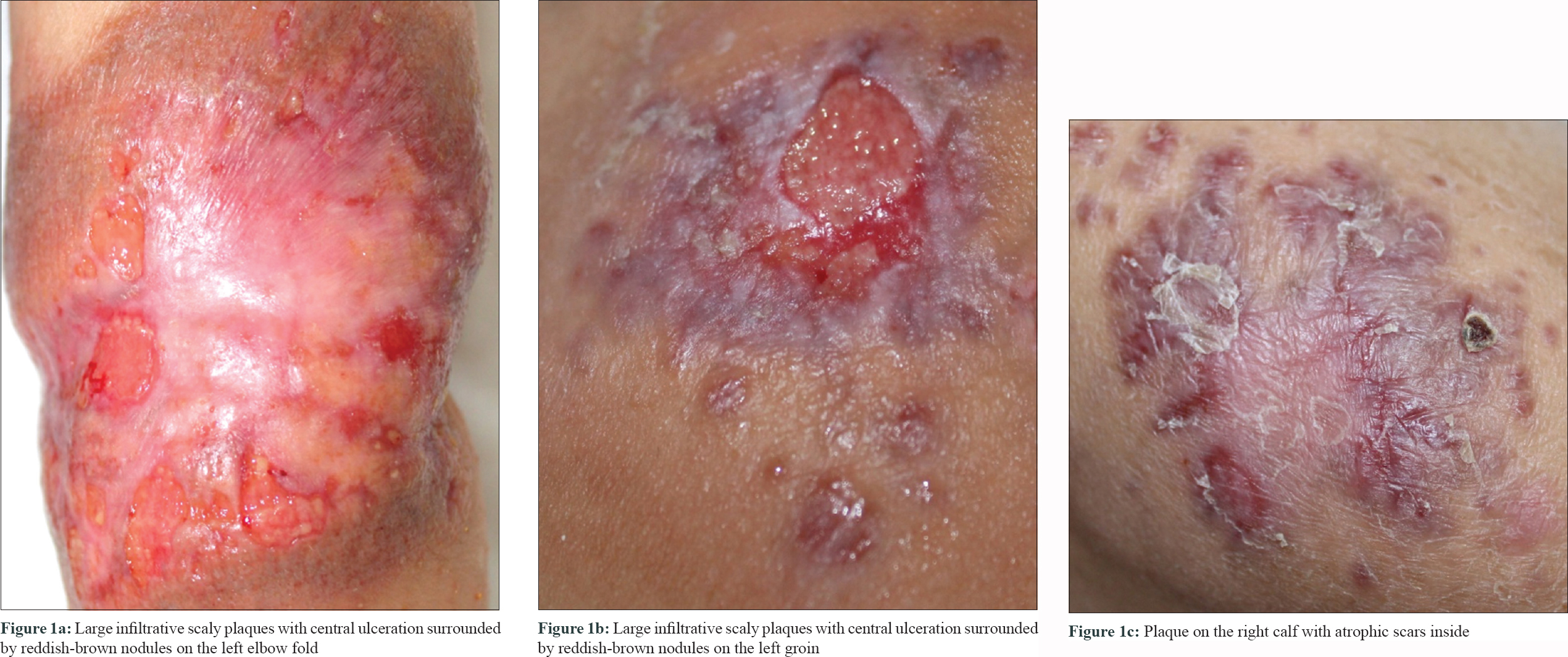
A Bacillus Calmette-Guérin-vaccinated 48-year-old well-nourished woman presented with a long history of reddish plaques with an elevated scaly surface located on her left elbow fold, left groin and right calf. She informed that these asymptomatic lesions had been present since infancy and had been slowly enlarging since then. The patient was referred to a dermatology clinic at the age of 38 years, where it was diagnosed as capillary-venous malformation after magnetic resonance imaging examination. However, the “birthmark” had ulcerated over the last 8 months and expanded despite regular dressing by nurses. There was no past history of tuberculosis and no known exposure to tuberculosis. She denied fever, night sweats, weight loss, cough and dyspnea. General physical examination was normal. However, the dermatological examination revealed three large, brownish-red, infiltrative plaques with whitish atrophic scars inside the plaques and central ulceration [Figure - 1]. There was no associated lymphadenopathy. Results of routine laboratory examinations were within normal limits. Dermoscopic examination revealed fine-focused telangiectasias on an orange-colored background with some whitish reticular streaks. These dermoscopic findings were suggestive of granulomatous skin disease. Biopsy specimens were taken from the three lesional sites. Histopathological examination found that each lesion showed granulomas in the dermis, composed of epithelioid cells and Langerhans giant cells surrounded by lymphocytes and plasma cells [Figure - 2]. Caseation necrosis was not seen. Ziehl-Neelsen staining and culture of biopsy tissues for mycobacteria were negative. A real-time polymerase chain reaction analyses of the DNA extracts from the elbow biopsy specimens detected Mycobacterium tuberculosis complex. Cultures of sputum and urine samples were negative for mycobacteria. Systemic computed tomography was normal. A final diagnosis of lupus vulgaris was made. Accordingly, a combination of rifampicin (600 mg/day), isoniazid (300 mg/day), pyrazinamide (1500 mg/day) and ethambutol (1500 mg/day) was successfully administered to treat the cutaneous lesions [Figure - 3]. The patient completed 9-month course of antituberculous therapy.
 |
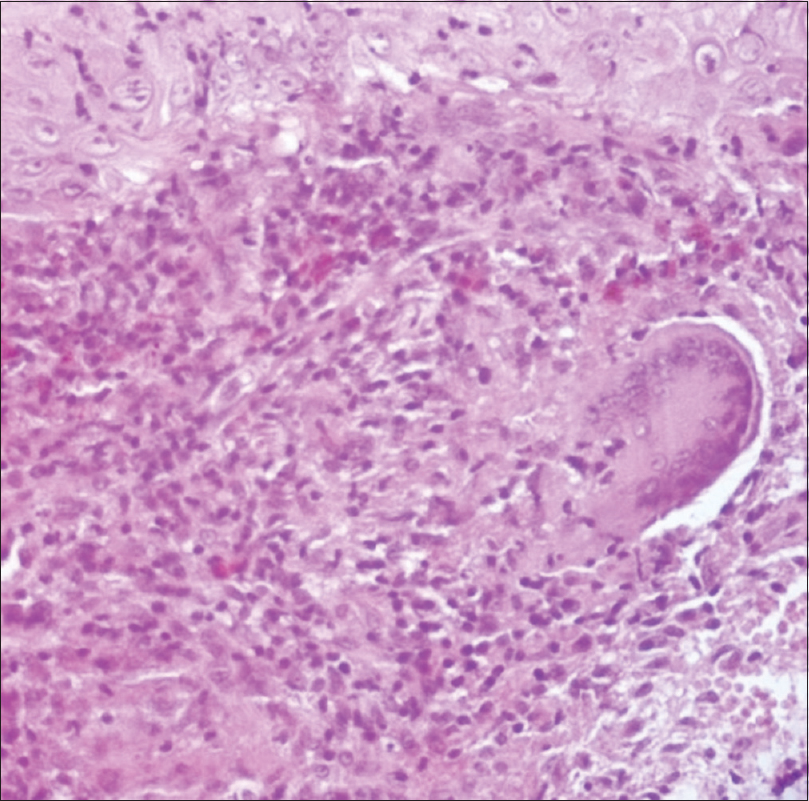 |
| Figure 2: Inflammatory infiltrate in the dermis which consists of granulomatous reaction composed of lymphocytes, epithelioid and giant cells (H and E, ×200) |
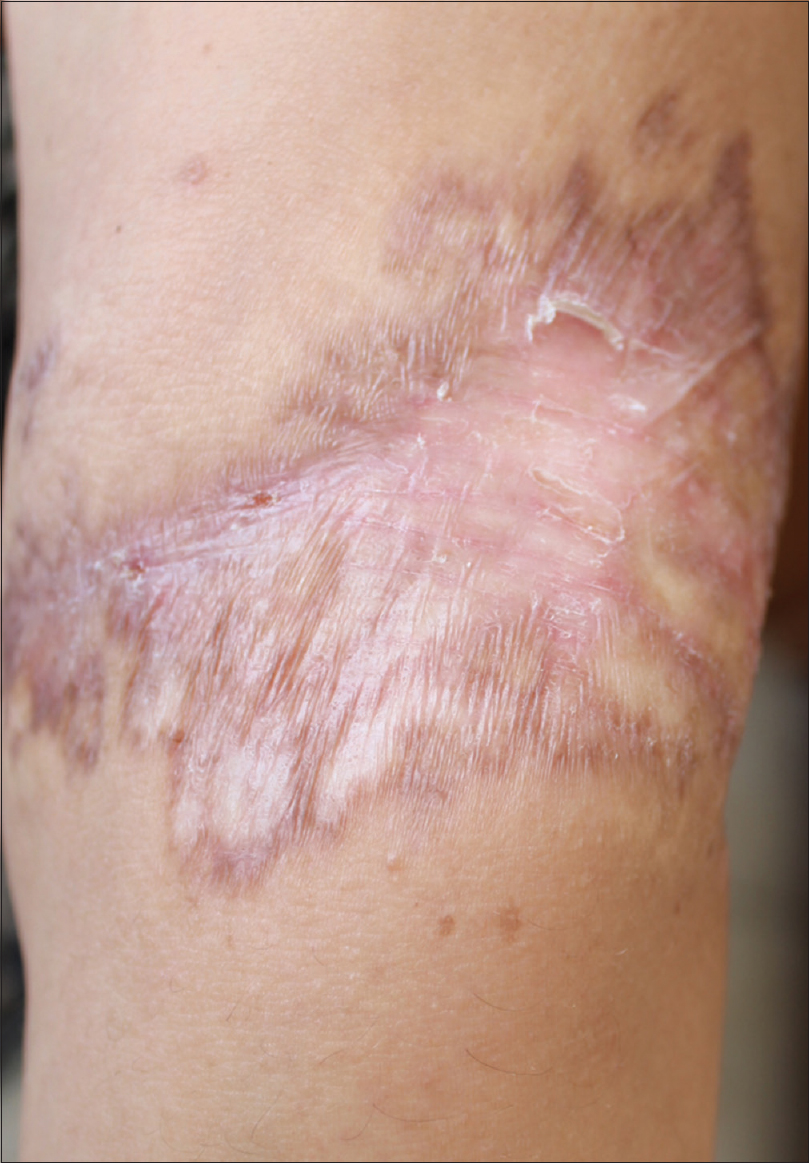 |
| Figure 3: Antituberculous therapy caused the lesions to regress with residual skin atrophy |
Tuberculosis is still an important health problem in underdeveloped and developing countries. Lupus vulgaris starts either by reinfection or by the lymphatic or hematogenous spread.[1] Since no endogenous source for tuberculosis was found, we speculated that reinfection was the case for this patient. Earlier, metastatic tubercular abscesses with systemic involvement have been reported in immunocompetent individuals.[2] However, disseminated lupus vulgaris in an immunocompetent host and its presence in a good general health host is very unusual.[3] Confirmation of diagnosis of lupus vulgaris continues to pose an enormous challenge. The chronicity, the variable clinical presentation and the paucibacillary nature may also lead to under-recognition of the condition and delayed initiation of treatment. Notwithstanding difficulties in diagnosis, a correct and adequate treatment is crucial because lupus vulgaris, if left untreated, carries the risk of local destruction or development of malignant skin tumors, especially squamous cell carcinoma. Although the chronicity of the disease is well-documented, only a few cases of lupus vulgaris diagnosed more than 40 years after onset have been previously reported.[4] Moreover, this common type of tuberculosis typically presents as a solitary well-demarcated reddish-brown plaque, often seen in the head and neck region, particularly on the nose and cheek but rarely seen in the limbs.[1] Several previous reports discussed similar cases of lupus vulgaris misdiagnosed as vascular malformation condition [Table - 1].[4] Therefore, the confusion between the two conditions could be resolved with careful history-taking, correlated with clinical and pathological findings. Our case suggests that dermoscopy potentially may enlighten clinics and provide clues for lupus vulgaris diagnosis when it shows an orange to golden color associated or not with linear vessels; the latter yellowish structureless area is the dermoscopic equivalent of the so-called “apple-jelly” sign seen under traditional diascopy. Nevertheless, none of the observed dermoscopic features is sufficiently specific alone for lupus vulgaris diagnosis, while their combination may result in increased sensitivity.[5] Therefore, a skin biopsy is recommended to confirm granulomatous skin disease and conduct tissue culture and polymerase chain reaction assays for a precise diagnosis of lupus vulgaris. Our case illustrates the importance of having a high index of suspicion for this condition on any atypical chronic lesion, as it is curable.

Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity but anonymity cannot be guaranteed.
Acknowledgements
We thank the patient for granting permission to publish this information. We are also indebted to Badreddine Sriha, MD, PhD, Department of Pathology, Farhat Hached University Hospital, for his interpretation of the cutaneous biopsies. He received no compensation for his contributions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol 2007;25:173-80.
[Google Scholar]
|
| 2. |
Almagro M, Del Pozo J, Rodríguez-Lozano J, Silva JG, Yebra-Pimentel MT, Fonseca E. Metastatic tuberculous abscesses in an immunocompetent patient. Clin Exp Dermatol 2005;30:247-9.
[Google Scholar]
|
| 3. |
Bayramgürler D, Sayan M, Aktürk AS, Bilen N, Aslan N, Turan D. Disseminated lupus vulgaris presenting with different atypical lesions. J Dermatol 2007;34:849-51.
[Google Scholar]
|
| 4. |
Yaldız M, Erdem T, Dikicier BS, Dilek FH. Lupus vulgaris mimicking hemangioma diagnosed 42 years after onset: A case report. J Med Case Rep 2015;9:215.
[Google Scholar]
|
| 5. |
Brasiello M, Zalaudek I, Ferrara G, Gourhant JY, Capoluongo P, Roma P, et al. Lupus vulgaris: A new look at an old symptom – The lupoma observed with dermoscopy. Dermatology 2009;218:172-4.
[Google Scholar]
|
Fulltext Views
4,813
PDF downloads
1,616





