Translate this page into:
An erythematous nodule on the nasal wing
Corresponding author: Dr. Alfonso Motolese, Department of Clinical and Experimental Medicine, Section of Dermatology, University of Messina, Via Consolare Valeria 1, Messina, Italy. alfonsomotolese93@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Motolese A, Macca L, Lentini M, Borgia F, Vaccaro M. An erythematous nodule on the nasal wing. Indian J Dermatol Venereol Leprol 2023;89:760-2
A 55-year-old Caucasian man presented with a one-month history of an asymptomatic and rapidly growing exophytic lesion on the left nasal wing [Figure 1a]. The lesion was painless with no bleeding or ulceration. His medical history reported a right total nephrectomy one year ago after the diagnosis of clear cell renal cell carcinoma, World Health Organization/International Society of Urological Pathology (WHO/ISUP) grading pT3a. Physical examination revealed a firm non-tender erythematous nodule of 2 × 2 cm size on the left ala nasi. Dermoscopy showed a wide polymorphic vessel characterized by linear and comma-shaped vessels, milky-red areas and bright red vessels on a white and red background [Figure 1b]. A punch-biopsy revealed a dermal nodular proliferation of large atypical cells well-demarcated, without connection with the epidermis [Figure 2a]. The cells presented huge cytoplasm, clear or eosinophilic, with round vesicular nuclei centered by round large nucleoli [Figure 2b]. Immunohistochemically, the neoplastic cells were positive for vimentin [Figure 3a] and paired box gene 8 (PAX8) [Figure 3b]. [Table 1] summarises a panel of immunohistochemical markers of some cutaneous clear cell lesions.

- Erythematous nodule with lobulated surface on the left nasal wing

- Dermatoscopy shows a wide polymorphic vessel characterized by linear and comma-shaped vessels, milky-red areas and bright red vessels on a white and red background (DermLite DL200 hybrid dermatoscope, 10X)
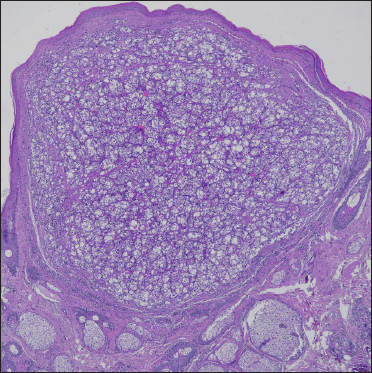
- Dermal nodular proliferation of large atypical cells well demarcated, without connection with the epidermis (haematoxylin & eosin, ×4)
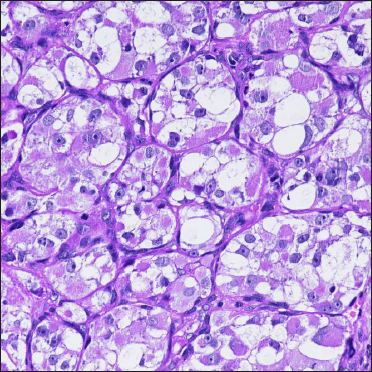
- The cells have huge cytoplasm, clear or eosinophilic, with round vesicular nuclei centered by large round nucleoli (haematoxylin & eosin, ×40)
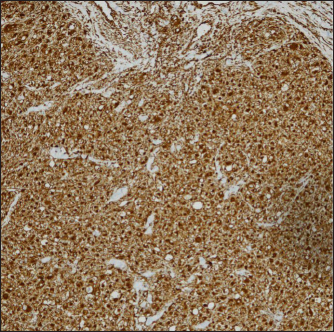
- Positivity for vimentin (diaminobenzidine, ×10)

- Positivity for PAX8 (diaminobenzidine, ×10)
| Cutaneous clear cell lesions | RCC-Ma | CD10 (CALLA) | EMA | CEA | PAX-8 | Vimentin | S-100 |
|---|---|---|---|---|---|---|---|
| CMccRCC | ± | ± | ± | ± | + | + | ± |
| CX | − | + | − | − | nd* | + | ± |
| CCH | − | ± | + | + | − | − | − |
| SA | − | ± | + | ± | nd* | + | + |
| SC | − | ± | ± | − | nd* | + | + |
RCC-Ma: Renal cell carcinoma marker, CD10 (CALLA): Common acute lymphoblastic Leukaemia antigen, EMA: Epithelial membrane antigen, CEA: Carcinoembryonic antigen, PAX-8: Paired box gene 8, CMccRCC: Cutaneous metastasis of clear cell renal cell carcinoma, CX: Cutaneous xanthoma, CCH: Clear cell hidradenoma, SA: Sebaceous adenoma, SC: Sebaceous carcinoma, *nd: Not determined (data not available in literature)
What is your diagnosis?
Diagnosis
Cutaneous metastasis of clear cell renal cell carcinoma
Discussion
Cutaneous metastasis of clear cell renal cell carcinoma is an uncommon condition and reportedly accounts for around 3 percent of all skin metastatic tumors, showing a relatively favourable outcome in solitary cases.1 They commonly occur on the scalp and face, presenting as rapidly growing nodules.2,3 Based on clinical and dermoscopic findings, our differential diagnosis included pyogenic granuloma, basal cell carcinoma, melanoma, Merkel cell carcinoma and Kaposi sarcoma. However, other benign and malignant skin lesions can mimic cutaneous metastasis of clear cell renal cell carcinoma.3 The mean survival is 10.9 months since diagnosis.1 Other common affected sites of clear cell renal cell carcinoma metastasis are the lung (60%), bone (30%), liver, lymph nodes and the brain.1-3 A few cases of renal cell carcinoma with skin metastasis are reported in the literature and majority of them are clear cell histologic type while others are of the papillary type.4,5 Cutaneous metastasis of clear cell renal cell carcinoma occurs due to haematogenous dissemination after initial spread along lymphatics but can also happen because of the tendency to invade the renal vein.2 In some cases, it may be present at the time of diagnosis of the primary disease or even present as a cutaneous growth with no urological symptoms. Patients may also develop cutaneous metastases after several years, especially in the low stage disease.2 Our patient was treated with an anti-programmed death-1 monoclonal antibody, Nivolumab 3 mg/kg per body weight every two weeks intravenously due to the detection of multiple masses in bones not responsive to first-line therapy. The patient did not experience any cutaneous adverse effects. After the third cycle, impressive regression of the lesion was observed, probably acting on the vascular network, as demonstrated by the fibrotic evolution of the nodule. During the follow-up after six months, no recurrence or new onset of skin lesions were observed.
Cutaneous metastasis of clear cell renal cell carcinoma, though infrequent, is not very rare.2 The skin should be always examined, and close attention should be paid to the diagnostic evaluation and follow-up for patients with clear cell renal cell carcinoma. In summary, this case highlights the prominent role of the dermatologist in the early diagnosis of cutaneous metastasis of clear cell renal cell carcinoma, which can contribute significantly to an increase in the survival of these patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Cutaneous metastases in renal cell carcinoma: A systematic review and a case report. Scand J Urol. 2019;53:9-13.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous metastases in renal cell carcinoma. Urol Int. 1999;63:164-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous metastasis of renal cell carcinoma to the cheek: A case report and literature review. Am J Case Rep. 2021;22:e928999.
- [CrossRef] [PubMed] [Google Scholar]
- Papillary renal cell carcinoma with cutaneous metastases. Am J Med Sci. 2010;339:458-61.
- [CrossRef] [PubMed] [Google Scholar]
- Papillary renal cell carcinoma type-II: A distinct. Annals pathol lab med. 2016;3:279-81.
- [Google Scholar]
- Renal cell carcinoma marker (RCC-Ma) is specific for cutaneous metastasis of renal cell carcinoma. J Cutan Pathol. 2007;34:381-5.
- [CrossRef] [PubMed] [Google Scholar]
- The utility of using immunohistochemistry in the differentiation of metastatic, cutaneous clear cell renal cell carcinoma and clear cell hidradenoma. J Cutan Pathol. 2017;44:612-15.
- [CrossRef] [PubMed] [Google Scholar]





