Translate this page into:
An unusual case of benign cutaneous lymphoid hyperplasia masquerading as diffuse Addisonian-like pigmentation with skin infiltration – An atypical presentation
Corresponding author: Dr. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Ahuja R, Patel V, Dagar S, Khandpur S. An unusual case of benign cutaneous lymphoid hyperplasia masquerading as diffuse Addisonian-like pigmentation with skin infiltration – An atypical presentation. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1268_2023
Dear Editor,
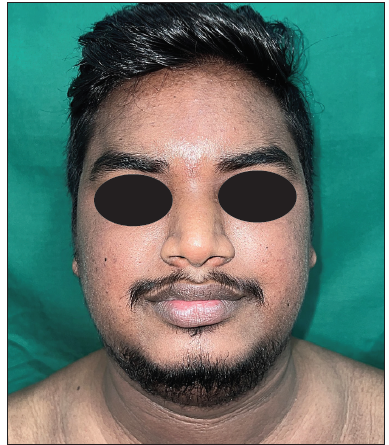
A 19-year-old boy presented with a 5-year history of gradually progressive hyperpigmented macules and papules involving the face, neck, trunk, and extremities. The disease had started as multiple erythematous papules that gradually progressed to involve the entire body over 1–2 years, becoming hyperpigmented and coalescent with time. Over the next two years, he noticed thickening of the skin on his face and neck, accompanied by noticeable neck widening. There was no history of fever, weight loss, or constitutional symptoms. The lesions spared the skin creases and folds and on the distal upper limbs, the papules were more discrete and linearly arranged. There was diffuse infiltration of the lower face, neck, upper back, axilla, and medial thigh [Figure 1]. In the left inguinal region, a single mobile, firm, and non-tender lymph node measuring 1.5 × 1 cm was palpable. There was no hepatosplenomegaly.
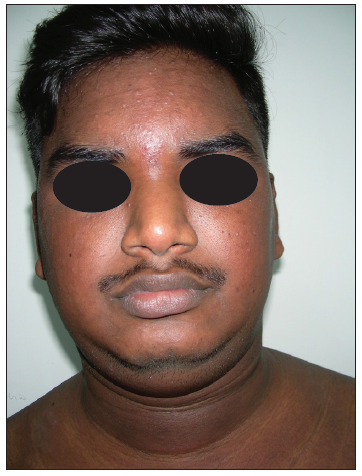
- The face shows diffuse infiltration and hyperpigmentation.

- Diffuse infiltration and hyperpigmentation across the trunk, with skin creases remaining unaffected.

- On the distal upper limbs, the hyperpigmented papules are arranged in a more discrete and linear fashion.
Dermoscopy of the lesions showed accentuation of the brown pigment network along with brown to black dots. There were no blue dots or globules. Various differentials were considered including addisonian pigmentation with paraproteinaemia, paraneoplastic acanthosis nigricans, POEMS syndrome, and papuloerythroderma of Ofuji. Haematological and biochemical investigations including early morning serum cortisol, vitamin B12 level, and serum and urine electrophoresis were unremarkable. There was no peripheral eosinophilia. A skin biopsy was performed from the infiltrated hyperpigmented skin on the neck and also from the discrete papule on the distal forearm. Histopathological examination of both specimens revealed multiple small, round to oval aggregates of lymphocytes and few plasma cells present in a peri-vascular and peri-eccrine location in both superficial and deep dermis [Figure 2]. Notably, there were no signs of cellular atypia, necrosis, or crush artefacts. Immunohistochemical analysis revealed CD3-positive lymphocytes dominating the superficial infiltrate, while the deeper nodular infiltrate contained lymphocytes positive for both CD3 and CD20 [Figure 3]. Subsequent immunohistochemistry showed CD3+ cells expressing a combination of both CD4 and CD8. These histological and immunohistochemical findings were indicative of a benign cutaneous lymphoid hyperplasia. As benign cutaneous lymphoid hyperplasia was not initially considered among our list of potential diagnoses, two additional biopsies were performed, both yielding similar findings. A lymph node biopsy was also done from the inguinal lymph node; however, it was a small fragment containing only adipose tissue.

- Photomicrograph from a biopsy of papule on forearm showing predominantly superficial and some deep dermal infiltrate of lymphocytes (Haematoxylin and Eosin stain, 20×)
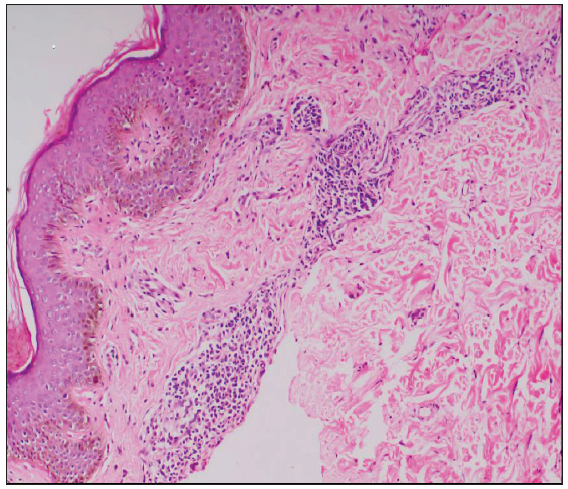
- Small, oval to oblong aggregates of lymphocytes and some plasma cells distributed in a peri-vascular distribution in the upper dermis (Haematoxylin and Eosin stain, 100×).

- Deep nodular collection of lymphocytes near dermal-subcutis junction (Haematoxylin and Eosin stain, 100×).
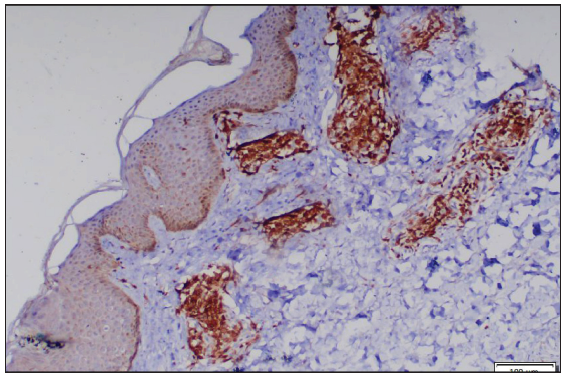
- Superficial infiltrates showing CD3+ lymphocytes (IHC for CD3, 100×). (IHC: immunohistochemistry)

- Deeper nodular infiltrate composed of (b) CD3+ lymphocytes (100×).
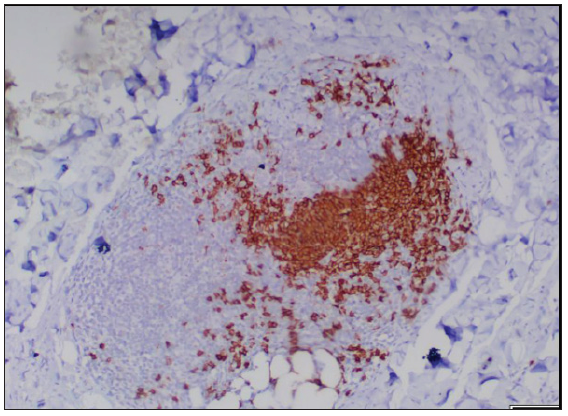
- Deeper nodular infiltrate composed of CD20+ lymphocytes (IHC for CD20, 100×). (IHC: immunohistochemistry)
Ultrasound of the neck revealed multiple sub-centimetric lymph nodes., A subsequent positron emission tomography-computed tomography (PET-CT) scan showed multiple, mildly metabolically active lymph nodes bilaterally in the cervical, axillary, and inguinal regions, suggestive of reactive involvement. While undergoing these investigations, the patient experienced an increase in facial and neck swelling, along with a painless swelling on the left eyelid and an extension of hyperpigmented lesions on the arms. Based on the radio-imaging results, the diagnosis of BCLH was confirmed, and the patient was started on treatment with oral prednisolone at 30 mg/day and hydroxychloroquine at 300 mg/day. Within one month, significant improvement in eyelid swelling was observed, completely resolving by the end of the second month. By the third month, there was substantial flattening of hyperpigmented papules on the arms, accompanied by reduced skin infiltration [Figure 4]. We have now begun to taper prednisolone and methotrexate has been introduced as a steroid-sparing agent. The patient remains under our care and follow-up.
- Substantial reduction in infiltration and pigmentation on the face after treatment.

- Marked reduction in infiltration and pigmentation of trunk.

- Reduction in both size and number of hyperpigmented papules on the forearm following the initiation of treatment.
Benign cutaneous lymphoid hyperplasia or pseudolymphoma refers to a benign reactive lymphocytic proliferation that can clinically or histologically resemble cutaneous lymphoma.1 The clinical spectrum of BCLH is diverse ranging from solitary to multiple nodules, grouped or disseminated papules, patches and plaques, eczematous pruritic plaques (lymphomatoid contact dermatitis), or even as erythroderma (lymphomatoid drug reaction).2 Extension of these lymphoid proliferations into deeper layers, invading the subcutis and insinuating between muscular planes have also been reported.3
Our patient presented with generalised hyperpigmentation along with areas of diffuse infiltration. Although there was a prior history of erythematous papules, on examination, only a few linearly arranged discrete hyperpigmented papules were appreciated on the distal forearms. The presence of underlying infiltration ruled out the clinical possibilities of lichen planus pigmentosus and Addisonian pigmentation. Though the pigmentation was more pronounced in the flexures, there was no evidence of velvety thickening in the intertriginous areas, nor was there any associated pruritus, oral papillomatosis, or palmoplantar thickening to suggest acanthosis nigricans maligna.4 While generalised skin hyperpigmentation is seen in POEMS syndrome, the absence of concomitant hypertrichosis, sclerodermoid skin thickening, and distal paresthesias to suggest peripheral neuropathy makes this diagnosis also less likely.5 Moreover, the absence of weight loss, constitutional symptoms, or Type B symptoms along with a chronic disease course spanning over five years favoured a benign aetiology.
The histologic finding of upper and mid-dermal nodular infiltrates of the polymorphous population of lymphocytes along with histocytes and plasma cells with no evidence of necrosis, atypical mitoses, or crush artefact strongly suggested a possibility of cutaneous lymphoid hyperplasia. Further immunopositivity for CD3 and CD20 suggested a mixed cell population (T- and B-cell type) compatible with pseudolymphoma.6
This atypical presentation with widespread skin involvement has not been previously reported in pseudolymphoma. In a report by Prka et al., they observed generalised hyperpigmentation along with disseminated lymphadenopathy as the initial manifestation in CD30+ anaplastic large cell lymphoma. Histopathological examination revealed numerous, brown-pigmented macrophages interspersed within the tumour cell infiltrate, which stained positive with Prussian blue. The authors hypothesised that hemosiderin-laden macrophages might be responsible for the diffuse hyperpigmentation, possibly arising from an unknown paraneoplastic process.7
This case underscores the diverse clinical spectrum of cutaneous lymphoid hyperplasia and highlights the importance of considering pseudolymphoma in the differential diagnosis of unusual dermatological presentations. Although diffuse hyperpigmentation is not a typical presentation of pseudolymphoma, the presence of areas of infiltration, prolonged disease duration, findings of reactive lymphadenopathy on imaging, and the biopsy results showing nodular lymphocytic aggregates confirmed the diagnosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- The many faces of lymphocytoma cutis. J EurAcad Dermatol Venereol. 2003;17:3-6.
- [CrossRef] [PubMed] [Google Scholar]
- Radiotherapy in aggressive cutaneous pseudolymphoma: A case report and review of literature. Radiat Oncol J. 2016;34:76-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Paraneoplastic cutaneous manifestations: Concepts and updates. An Bras Dermatol. 2013;88:9-22.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous manifestations in POEMS syndrome: Case report and review. Case Rep Dermatol. 2015;7:61-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous pseudolymphoma: A clinicopathological study and immunohistochemical patterns. Caspian J Intern Med. 2021;12:283-289.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Diffuse skin hyperpigmentation in CD30+ lymphoproliferation. Ann Saudi Med. 2012;32:318-20.
- [CrossRef] [PubMed] [Google Scholar]





