Translate this page into:
An unusual case of blue rubber bleb nevus syndrome with unilateral linear distribution
Correspondence Address:
Dan Luo
Department of Dermatology, the First Affiliated Hospital of Nanjing Medical University
China
| How to cite this article: Xu Y, Zhou B, Zhang M, Luo D. An unusual case of blue rubber bleb nevus syndrome with unilateral linear distribution. Indian J Dermatol Venereol Leprol 2013;79:269-270 |
Sir,
Blue Rubber Bleb Nevus Syndrome (BRBNS) is a rare disorder with only about 200 cases reported in the literature. BRBNS is characterized by multiple venous malformations on the skin and in the gastrointestinal tract. Herein, we present a case of a 26-year-old female patient with multiple lesions distributed along the Blaschko line in the skin fat layer on the right hand and forearm together with venous malformations in the lower esophagus. To the best of our knowledge, this is the first reported case of BRBNS associated with Blaschko line distribution of lesions.
A 26-year-old woman was referred to our department for lesions on her right palm and arm. Total duration of the lesions was 3 years and they had increased in size and number over the past two years without any symptoms. The lesions had not changed during her pregnancy neither had they improved with cryotherapy and carbon dioxide laser therapy treatment in the past. There was no similar case in her family.
Clinically, she was thin looking and pale. Physical examination showed multiple nodules of variable sizes, with diameters ranging from 2mm to15mm, distributed along the Blaschko line on the right hand and forearm medially [Figure - 1].
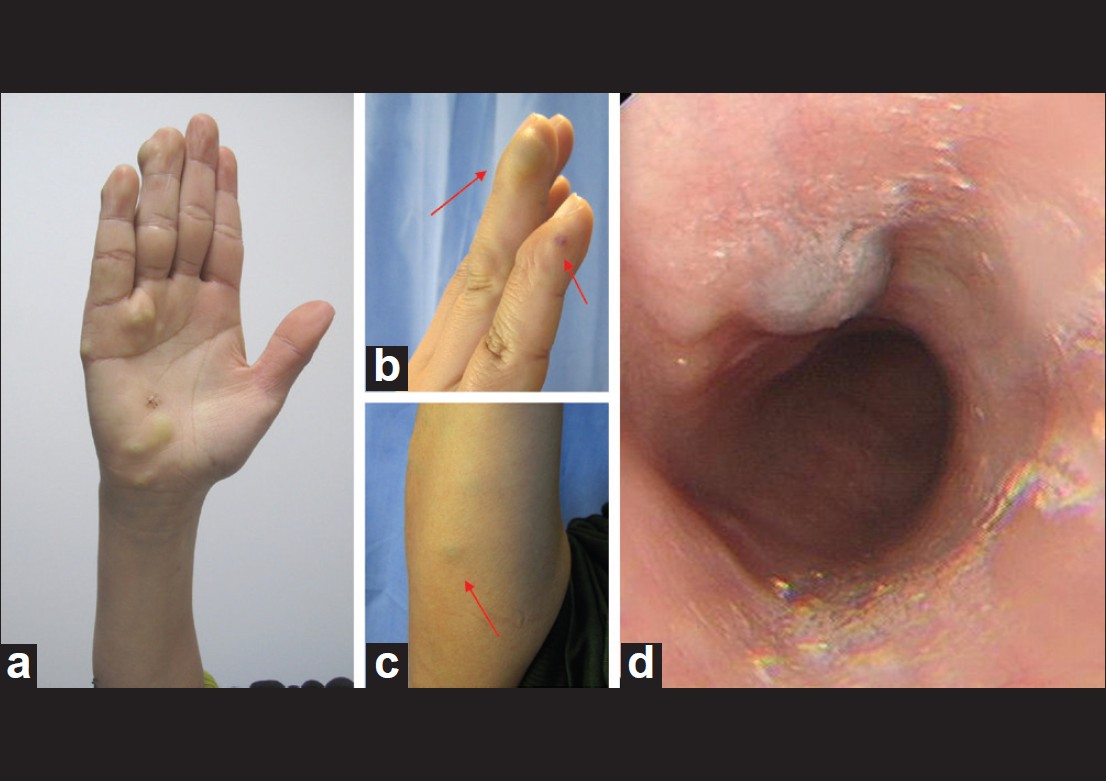 |
| Figure 1: The Blaschko line distribution (a), multiple nodules on the right hand (b) and right forearm (c) (shown by red arrows). Upper gastrointestinal endoscopy showing submucosal blue bulge in the lower esophagus (d) |
Hematological evaluation indicated iron deficiency anemia. Routine stool test showed positive result for occult blood. Further examinations were conducted. B-ultrasonic examination on several skin lesions revealed some hypo echoic areas in the fat layer rich with blood flow. Histopathology revealed a cluster of dilated irregular vein spaces lined by a thin endothelial cells layer in the subcutaneous fat. Some lumina contained thrombi. Immunohistochemical findings were positive for cluster of differentiation (CD)31 (+), CD34 (+), vascular endothelial growth factor (VEGF), F8 (+) and ki-67 and proliferating cell nuclear antige (PCNA) staining showed a proliferation index less than 1% [Figure - 2]. The upper gastrointestinal endoscopy showed submucosal bulge in the lower esophagus while B ultrasound showed echogenic mass under the mucosa, considered to be esophageal hemangioma. Small intestine endoscopy did not reveal any abnormality.
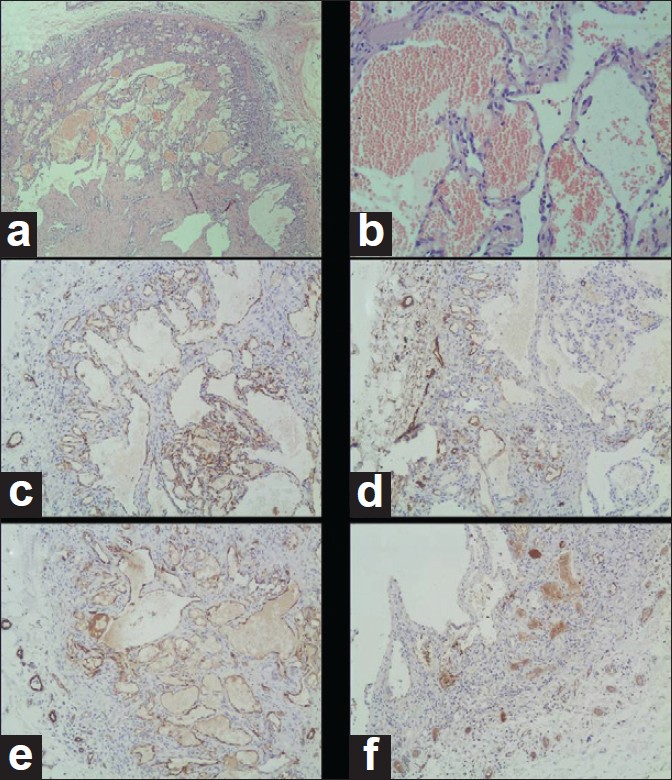 |
| Figure 2: Histopathology showing obviously dilated veins (H and E stain, original magnification × 100 a and × 200 b), in the fat layer. Immunohistochemical positive findings for CD31, CD34, VEGF and F8 (original magnification × 100, shown as c-f, respectively) |
We recommended long-pulsed neodymium-doped yttrium aluminum garnet (Nd:YAG) laser therapy for the skin lesions and endoscopic ligation for the esophageal lesion but the patient refused for economic reasons. Oral iron supplementation and close follow-up were recommended for her.
Thus, our final diagnosis for BRBNS was based on physical examination, B ultrasonic, pathological and immunohistochemical findings, which were all suggestive of BRBNS. These findings are linearly distributed blue colored skin nodules on one side of the forearm and palm together with similar nodules in the lower esophagus, hypoechoic areas in the fat layer rich with blood flow and histopathology showing dilated veins in the fat layer. Additionally, the immunohistochemical results showed that the tumor was composed of veins with low endothelial proliferation, features suggestive of BRBNS.
As reported, BRBNS appears as venous malformations on skin and other organs, arising at birth or within adolescent hood and most commonly affecting the gastrointestinal tract, including mouth. [1] Some of clinical manifestations are chronic iron-deficiency anemia, vomiting, bloody stool, and intussusceptions. [2] BRBNS is rarely seen in respiratory tract, central nervous system, and reproductive tract. [3]
The presence of cutaneous lesions should alert clinicians on possible presence of internal vascular malformations. In our presented case, it was supposed that weight loss and iron deficiency anemia were caused by occult chronic bleeding from gastrointestinal vascular malformations. Unfortunately, the patient refused further examination and treatment. We prescribed oral iron supplementation for anemia and recommended timely routine examination of blood and stool. In case her condition gets worse, the patient should go back to the hospital.
The differential diagnoses can be made according to specific clinical manifestations, laboratory results, or other specific investigations. The following diseases should be ruled out in the differential diagnosis: Klippel-Trenaunay syndrome, familial glomangiomatosis, diffuse neonatal hemangiomatosis, and Maffuci syndrome.
In the literature, skin lesions from BRBNS are mostly diffusely distributed all over the body, with blue subcutaneous nodules more obvious. But in our case, the skin lesions are located deeper in the fat layer, not obviously appearing as blue blebs. The rarest situation was the unilateral linear distribution of lesions along the Blaschko line. This feature has never been reported before.
Several congenital and acquired dermatological conditions are known to follow the Blaschko lines, as reviewed by Tagra et al.,[4] The skin components, separately or in combination, can be involved in special morphological manifestations. The embryological basis of these lines has not yet been clearly elucidated.
Several therapeutic modalities have been reported for treatment of BRBNS. These include cryotherapy, sclerotherapy, surgery and newly-reported long-pulsed Nd:YAG 1064nm laser for cutaneous lesions. [5] For economic reasons our patient refused further treatment except oral iron supplements.
| 1. |
Suma GN, Ravi Prakash SM, Rao D, Goel S. Blue rubber bleb nevus syndrome: Prominent oral findings. Indian J Dermatol Venereol Leprol 2010;76:168-71.
[Google Scholar]
|
| 2. |
Hasosah MY, Abdul-Wahab AA, Bin-Yahab SA, Al-Rabeaah AA, Rimawi MM, Eyoni YA, et al. Blue rubber bleb nevus syndrome: Extensive small bowel vascular lesions responsible for gastrointestinal bleeding. J Paediatr Child Health 2009;46:63-5.
[Google Scholar]
|
| 3. |
Tanaka N, Tsuda M, Samura O, Miyoshi H, Hara T, Kudo Y. Blue rubber bleb nevus syndrome: Report of a patient with hemangiomas of the vaginal portion of the cervix appearing during pregnancy. J Obstet Gynaecol Res 2007;33:546-8.
[Google Scholar]
|
| 4. |
Tagra S, Talwar AK, Walia RL. Lines of Blaschko. Indian J Dermatol Venereol Leprol 2005;71:57-9.
[Google Scholar]
|
| 5. |
Moser CM, Hamsch C. Successful treatment of cutaneous venous malformations in a blue rubber bleb nevus syndrome patient by Nd:YAG laser. Br J Dermatol 2012;166:1143-5.
[Google Scholar]
|
Fulltext Views
2,591
PDF downloads
1,213





