Translate this page into:
An unusual case of lymphomatoid papulosis type E with extensive necrosis
2 Department of Pathology, Hospital Ramon Y Cajal, Madrid, Spain
Correspondence Address:
Cristina Pindado-Ortega
Department of Dermatology, Hospital Ramon Y Cajal, Carretera Colmenar Viejo, km 9.100, 28034 Madrid
Spain
| How to cite this article: Pindado-Ortega C, Fonda-Pascual P, Buendía-Castaño D, Fernández-González P, Peña-Jaimes L, Carrillo-Gijón R. An unusual case of lymphomatoid papulosis type E with extensive necrosis. Indian J Dermatol Venereol Leprol 2018;84:515-517 |
Abstract
Lymphomatoid papulosis type E (LyP) is a recently described subtype of LyP characterized by an angioinvasive infiltrate of atypical lymphocytes expressing CD30. We present a case of type E LyP with extensive cutaneous necrosis in the histopathological evaluation which was misdiagnosed as an ulcerative form of bacterial skin infection. The remarkable cutaneous necrosis showed in our case might be related to the angiodestructive infiltrate that was present in this circumstance.
Introduction
Lymphomatoid papulosis (LyP) is a primary cutaneous CD30-positive T-cell lymphoproliferative disorder.[1] LyP is classified into five histologic subtypes according to histopathological findings (types A, B, C, D, and E). LyP type E is a recently described subtype of LyP characterized by an angioinvasive infiltrate of atypical lymphocytes expressing CD30 that can be misdiagnosed with aggressive forms of angiocentric cutaneous lymphomas. Herein we describe a case of type E LyP with extensive cutaneous necrosis in the histopathological evaluation.
Case Report
A 69-year-old Caucasian man with a non-significant medical history presented to the emergency department with a 2-month history of cutaneous lesions. They were primarily located in the upper extremities. The trunk and lower extremities were later involved. Spontaneous regression of the primary lesions had occurred. He complained of mild pruritus when the lesions initially appeared, but they were asymptomatic upon presentation. He did not report any associated pain or trauma. He acknowledged two episodes of diarrhea in the previous month. No fever or other symptoms were present and the results of a routine blood test were normal. Physical examination revealed indurated papules and plaques with raised edges, some with focal necrosis and some with hemorrhagic crusting, involving upper and lower extremities [Figure - 1]a and [Figure - 1]b. An 8 mm punch biopsy was taken from one of the necrotic lesions. Amoxicillin 875 mg/clavulanate 125 mg was prescribed three times daily for 7 days with no improvements seen in his condition. Histopathological examination showed extensive wedge-shaped necrosis affecting the central part of the biopsy [Figure - 2]. There was a prominent epidermal necrosis. At the edge of this necrosis it was observed a lichenoid reaction pattern and conspicuous epidermotropism of small-sized to medium size lymphoid cells. At the periphery of the prominent necrosis there was an intense infiltrate of small and medium sized atypical lymphocytes mixed with small lymphocytes, neutrophils and eosinophils. The infiltrate was dense, band-like within superficial dermis, whereas in the mid and deep dermis, it was disposed around the vessels, with a prominent angiocentric and angiodestructive pattern [Figure - 3]. Many vessels showed intraluminal thrombosis. Immunohistochemical staining showed a strong positive result for CD30, CD8, CD3, and Multiple Myeloma Oncogene 1 [Figure - 4]. Other pan-T-cell markers (CD5 and CD7) were partially lost. Cytotoxic proteins (T-cell intracellular antigen-1, perforin, and granzyme B) as well as CD56 were negative. Epstein-Barr virus in situ hybridization was negative. With these findings, a diagnosis of type E LyP was made and the patient was treated with topical methylprednisolone acetate. After 3 months of follow-up, all lesions had resolved, with scarring in the areas of the preceding lesions.
 |
| Figure 1 |
 |
| Figure 2: Biopsy specimen of the right leg shows a markedly intense wedge-shaped necrosis affecting the central part of the biopsy (H and E, ×20) |
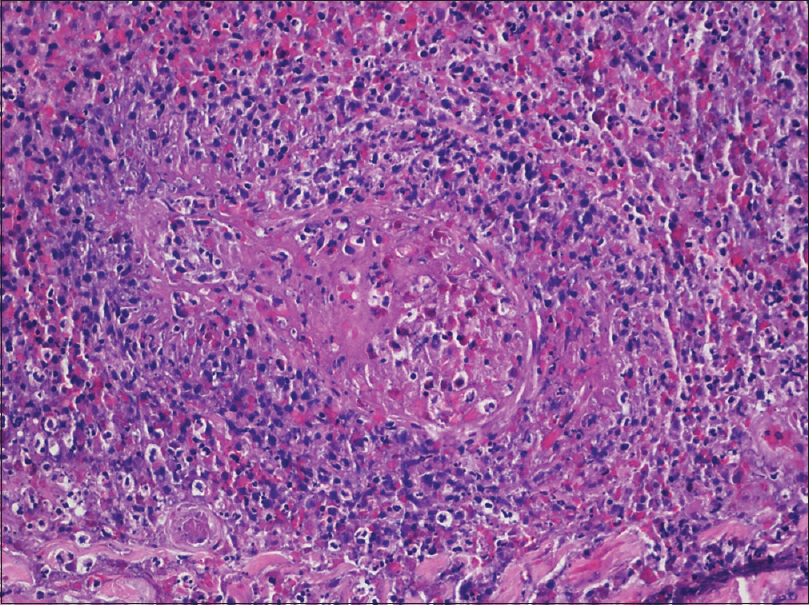 |
| Figure 3: Biopsy demonstrating an angiocentric and angiodestructive infiltrate of atypical lymphocytes (H and E, ×100) |
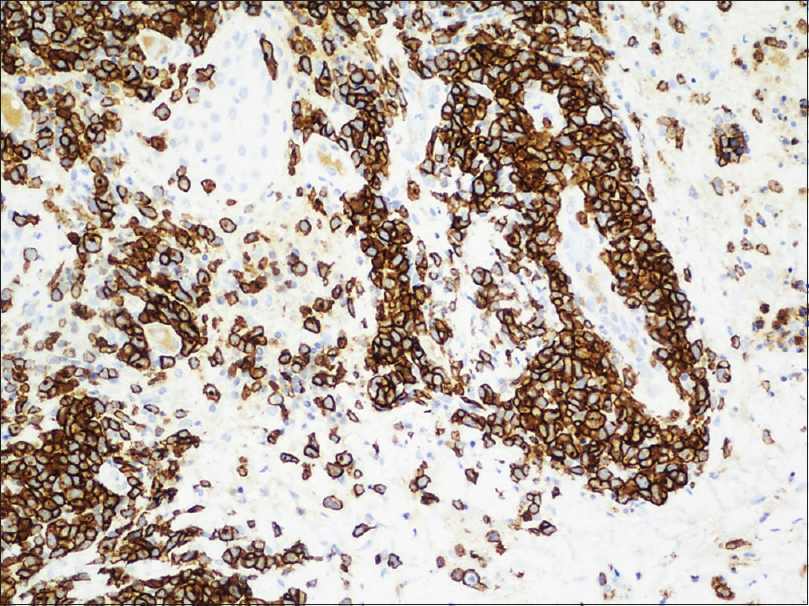 |
| Figure 4: Atypical lymphocytes expressing CD30 (×100) |
Discussion
LyP is defined as a primary cutaneous CD30 (Ki-1)-positive T-cell lymphoproliferative disorder [1] firstly described by Macaulay in 1968.[2] Five histological types of LyP have been identified: A, B, C, D, and E. Type A is characterized by the existence of large pleomorphic positive lymphocytes scattered in a background of mixed inflammatory cells. Type B exhibits an epidermotropic infiltrate of small-size lymphocytes expressing CD30. Type C exhibits cohesive sheets of large pleomorphic CD30 positive lymphocytes. Type D shows an epidermotropic infiltrate of lymphocytes coexpressing CD30 and CD8. Type E is characterized by an angioinvasive infiltrate of atypical lymphocytes expressing CD30 and frequently CD8.[1] LyP subtypes can coexist synchronously or metachronously in the same patient.[3] All LyP types manifest with a few papulonodular lesions which rapidly evolve into larger ulcerations that undergo spontaneous regression within a few weeks, occasionally leaving behind scars.[1]
Type E LyP was described by Kempf et al.[1]g in 2013 in a series of 16 patients, but it was firstly reported in 2004 by Wu and Tsai.[4] The histopathological changes include a dermal infiltrate of small to large pleomorphic CD30 and mostly CD8 lymphoid cells that infiltrate the walls of small to medium size dermal and subcutaneous blood vessels.[1]
Diagnosis is based on clinical, histological, and immunohistochemical findings. It is vital to recognize this variant to avoid misdiagnosis with aggressive cutaneous lymphomas. Nasal type extranodal NK/T-cell lymphomas uncommonly express CD30 and Epstein-Barr virus can be detected by in situ hybridization. Type E LyP lack the expression of T-cell receptor-d and express the a/b chain of TCR which excludes cutaneous g/d-positive T-cell lymphoma. Primary cutaneous CD8-positive epidermotropic cytotoxic T cell lymphomas are CD30 negative. Occasionally, the course of the disease with spontaneous regression and recurrences without visceral spread will help us in the diagnosis. Lymphoid malignancies co-occur with LyP in approximately 20–40% of patients,[5] but only in 5% of patients with LyP type E.[6] In contrast to its angiodestructive character, type E LyP may exhibit a more indolent course than other subtypes.
Treatments reported in the literature include topical steroids, surgical excision, methotrexate, radiation, and phototherapy. Spontaneous resolution of lesions has also been observed.[1] We were unable to find any previous reports of disease progression or death.
Dermatologists should be aware of the existence of LyP type E as its clinical features may be misdiagnosed as an ulcerative form of bacterial skin infections leading the patient to undergo unnecessary antibiotic treatment. The fact that our case shows remarkably cutaneous necrosis might be related to the angiodestructive infiltrate that was present in this circumstance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kempf W, Kazakov DV, Schärer L, Rütten A, Mentzel T, Paredes BE, et al. Angioinvasive lymphomatoid papulosis: A new variant simulating aggressive lymphomas. Am J Surg Pathol 2013;37:1-13.
[Google Scholar]
|
| 2. |
Macaulay WL. Lymphomatoid papulosis. A continuing self-healing eruption, clinically benign – Histologically malignant. Arch Dermatol 1968;97:23-30.
[Google Scholar]
|
| 3. |
El Shabrawi-Caelen L, Kerl H, Cerroni L. Lymphomatoid papulosis: Reappraisal of clinicopathologic presentation and classification into subtypes A, B, and C. Arch Dermatol 2004;140:441-7.
[Google Scholar]
|
| 4. |
Wu WM, Tsai HJ. Lymphomatoid papulosis histopathologically simulating angiocentric and cytotoxic T-cell lymphoma: A case report. Am J Dermatopathol 2004;26:133-5.
[Google Scholar]
|
| 5. |
Kunishige JH, McDonald H, Alvarez G, Johnson M, Prieto V, Duvic M. Lymphomatoid papulosis and associated lymphomas: A retrospective case series of 84 patients. Clin Exp Dermatol 2009;34:576-81.
[Google Scholar]
|
| 6. |
Kiavash K, Abner SM, Malone JC. New variant lymphomatoid papulosis type E preceding and coexisting with mycosis fungoides - A case report and review of the literature. J Cutan Pathol 2015;[Doi: 10.1111/cup. 12606].
[Google Scholar]
|
Fulltext Views
4,279
PDF downloads
1,919





