Translate this page into:
Angiolymphoid hyperplasia with eosinophilia on penis in HIV-positive patient: An unusual presentation
Correspondence Address:
Dhananjay K Damle
B-2/302, Lunkad Colonnade-I, Viman nagar, Pune - 411014, Maharashtra
India
| How to cite this article: Damle DK, Raotole SS, Belgaumkar VA, Mhaske CB. Angiolymphoid hyperplasia with eosinophilia on penis in HIV-positive patient: An unusual presentation. Indian J Dermatol Venereol Leprol 2013;79:109-111 |
Sir,
A 36-year-old uncircumcised male, known HIV-positive since 3 years, presented with an asymptomatic, solitary, flesh-colored growth on his penis with a history of gradual increase in the size of the lesion over 6 weeks. There was no history of painful erections, deviation of penis on erection, dyspareunia, or any urinary symptoms. The CD4 count, before initiating highly active anti-retroviral treatment (zidovudine, lamivudine, and nevirapine) two years ago, was 198/ mm 3 .
Cutaneous examination revealed a solitary, sub-preputial pink, flesh-colored non-foul-smelling exophytic polypoid eroded indurated growth with moist surface measuring about 1.5 × 1 cm over ventrolateral aspect of penile shaft, [Figure - 1]a which was non-tender, non-friable, did not bleed on manipulation and was covered with scant yellowish slough, without significant inguinal lymphadenopathy. The rest of dermatological and systemic examination was normal. Other differentials considered were donovanosis, hypertrophic genital herpes, and primary chancre.
 |
| Figure 1: (a) Single, sub-preputial exophytic polypoid eroded growth measuring 1.5 × 1 cm at first presentation. (b) Lesion measuring 3 cm × 2.5 cm after 12 weeks. |
Routine laboratory parameters were normal, and screening tests for sexually transmitted infections including venereal disease research laboratory (VDRL) test were negative. CD4 + T lymphocyte count was 345/mm 3 . On failure to respond to 14 days of oral acyclovir and 21 days of oral erythromycin, incisional biopsy was performed, which revealed extensive mucosal ulceration lined by acute inflammatory infiltrate. [Figure - 2]a Sub-epithelial tissue showed nodulovascular proliferation lined by plump epithelioid endothelial cells with abundant eosinophilic cytoplasm, hyperchromatic nuclei, prominent nucleoli and few lesional cells showed intracytoplasmic vacuoles. [Figure - 2]b The inflammatory infiltrate was rich in eosinophils and lymphocytes with few plasma cells. [Figure - 2]c Pleomorphism was minimal without any cytological atypia, which was consistent with diagnosis of angiolymphoid hyperplasia with eosinophilia (ALHE). There was no peripheral blood eosinophilia.
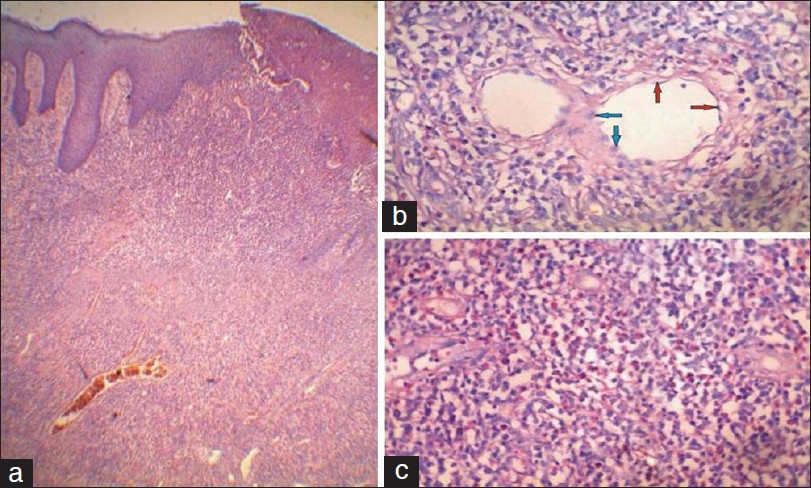 |
| Figure 2: (a) Ulcerated epithelium. Vascular proliferation with dense infiltrate in sub-epithelial tissue on hematoxylin and eosin stain at 4×. (b) Vascular channels lined by plump endothethelial cells (blue arrow) with intracytoplasmic vacuoles (red arrow) on hematoxylin and eosin stain at 40×. (c) Dense inflammatory infiltrate with predominance of lymphocytes and Eosinophils on hematoxylin and eosin stain at 40× |
Due to progressive increase in size of lesion to 3 cm × 2.5 cm over 12 weeks, [Figure - 1]b a complete local excision of the growth with therapeutic circumcision was performed with no recurrence over 14 months of follow-up.
ALHE, first reported in 1969, is an uncommon idiopathic condition with female preponderance, presenting between 3 rd to 5 th decade of life. [1] It is seen most commonly in Asians, followed by whites and rarely in blacks. Approximately 85% of lesions occur near the ear, forehead, or scalp, extremities being the next most common site. It presents as solitary, few or multiple, sometimes grouped, erythematous, violaceous or brown papules, plaques, or nodules, typically being unilateral. [1] Most lesions are 0.5-2 cm in diameter and may be eroded or crusted. Lesions may be associated with pruritus or pain, or may pulsate. [1] Rare sites of involvement include the hands, shoulders, breasts, penis, oral mucosa and tongue, orbit, eyelids, and lacrimal glands. [2] Natural course of ALHE tends to be chronic and non-remitting over months to years. Approximately 20% patients have peripheral blood eosinophilia.
Histology shows a well-defined area of vascular proliferation in the dermis and/or subcutis, with large epithelioid or histocytoid endothelial cells containing abundant cytoplasm, often with vacuoles and an infiltrate of variable numbers of eosinophils and lymphocytes. The stroma is myxoid, with minimal or no fibrosis. [1],[3]
Olsen and Helwig found, in 53 cases out of 116, an "an arterial structure" appearing to be associated with venules or "area of endothelial proliferation," which provided evidence that these lesions represent a form of arterio-venous shunt. [4]
The pathogenesis of ALHE is unknown but is considered to be a reactive phenomenon, possibly in response to or in association with an underlying vascular malformation. [1] There is history of trauma in some cases, and hyperestrogenemia (e.g. pregnancy, oral contraceptive use) may foster lesion growth. [1] T-cell monoclonality has been reported in few cases.
A comprehensive review of literature revealed less than 25 cases of ALHE occurring on penis. [5],[6],[7],[8] In the largest series, Fetsch et al described 19 cases of ALHE occurring on penis. [5] D′Offizi et al reported a case of ALHE in an HIV-seroreactive patient at extragenital site. [9]
Despite some clinico-pathological overlap, ALHE and Kimura Disease (KD) appear to be distinct entities. Lesions of ALHE are usually smaller, more superficial, more numerous and often symptomatic than those of KD. Histopathologically, lymphoid follicles represent dominant characteristic of KD, whereas large epithelioid endothelial cells are a key feature of ALHE. [10]
ALHE should be distinguished from a variety of benign and malignant vascular proliferations, including pyogenic granuloma, epithelioid hemangioendothelioma, angiosarcoma, and Kaposi sarcoma, all of which lack a noticeable eosinophil infiltrate. It should also be differentiated from cutaneous lymphoid hyperplasia, cutaneous B-cell lymphomas, bacillary angiomatosis, and bartonellosis- many of which have distinctive histopathological features.
Intervention is indicated by the number, location, and size of the lesions. Solitary or a few small lesions may benefit from excision or Mohs micrographic surgery. Recurrence at the surgical site has been reported, which fortunately was not noted in our patient. Other treatment modalities used with some success include topical, systemic, and intralesional steroid administration, topical tacrolimus, interferon α-2b therapy, cryotherapy, sclerotherapy, intralesional bleomycin, radiofrequency excision, radiotherapy, and lasers. [1]
Thus, ALHE is an uncommon disorder with restricted sites of predilection and its occurrence on penis is extremely rare. To the best of our knowledge, a case of ALHE on penis in an HIV sero-reactive patient is hitherto unreported.
| 1. |
Leiferman KM, Peters MS. Eosinophils in cutaneous diseases. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7 th ed. New York: McGraw Hill; 2008. p. 307-17.
th ed. New York: McGraw Hill; 2008. p. 307-17.'>[Google Scholar]
|
| 2. |
Taylor SK, Meyerle JH, Glusac EJ . Angiolymphoid hyperplasia with eosinophilia. Available from: http://emedicine.medscape.com/article/1082603-overview. [Last accessed on 2012 May 5].
[Google Scholar]
|
| 3. |
Ismail M, Damato S, Freeman A, Nigam R. Epithelioid hemangioma of the penis: Case report and review of literature. J Med Case Reports 2011;5: 260.
[Google Scholar]
|
| 4. |
Olsen TG, Helwig EB. Angiolymphoid hyperplasia with eosinophilia. A clinicopathologic study of 116 patients. J Am Acad Dermatol 1985;12:781-96.
[Google Scholar]
|
| 5. |
Fetsch JF, Sesterhenn IA, Miettinen M, Davis CJ Jr. Epithelioid hemangioma of the penis: A clinicopathologic and immunohistochemical analysis of 19 cases, with special reference to exuberant examples often confused with epithelioid hemangioendothelioma and epithelioid angiosarcoma. Am J Surg Pathol 2004;28:523-33.
[Google Scholar]
|
| 6. |
Dewan P, Francis ND, Lear JT, Bunker CB. Angiolymphoid hyperplasia with eosinophilia affecting the penis. none Br J Dermatol 2008;159:755-7.
[Google Scholar]
|
| 7. |
Nishi M, Matsumoto K, Fujita T, Satoh T, Iwabuchi K, Iwamura M, et al. Angiolymphoid hyperplasia with eosinophilia on penile skin in a 7-year-old child. J Pediatr Surg 2011;46:559-61.
[Google Scholar]
|
| 8. |
Ohmori S, Sugita K, Sawada Y, Hino R, Nakamura M, Tokura Y. Angiolymphoid hyperplasia with eosinophilia occurring on the penis. none Eur J Dermatol 2010;20:545-6.
[Google Scholar]
|
| 9. |
D'Offizi G, Ferrara R, Donati P, Bellomo P, Paganelli R. Angiolymphoid hyperplasia with eosinophils in HIV infection. AIDS 1995;9:813-4.
[Google Scholar]
|
| 10. |
Wood G S. Inflammatory diseases that simulate lymphomas: Cutaneous pseudolymphomas. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7 th ed. New York: McGraw Hill; 2008. p. 1402-13.
th ed. New York: McGraw Hill; 2008. p. 1402-13.'>[Google Scholar]
|
Fulltext Views
2,529
PDF downloads
1,291





