Translate this page into:
Angiosarcoma of the scalp and face associated with Kasabach–Merritt syndrome and disseminated intravascular coagulation
Correspondence Address:
Jianfang Sun
Institute of Dermatology, Chinese Academy of Medical Sciences and Peking Union Medical College, Nanjing
China
| How to cite this article: Wen S, Zhang W, Yang Y, Sun J. Angiosarcoma of the scalp and face associated with Kasabach–Merritt syndrome and disseminated intravascular coagulation. Indian J Dermatol Venereol Leprol 2016;82:96-97 |
Sir,
Angiosarcoma is a rare sarcoma that mostly affects the elderly and usually occurrs on the head. Kasabach–Merritt syndrome is a condition of consumption coagulopathy, mostly described in children with a benign hemangioma, only a few cases have been reported to be correlated with angiosarcoma in adults. Disseminated intravascular coagulation is a clinico-pathological syndrome which can result in the generation of fibrin clots that may cause organ failure with concomitant consumption of platelets and coagulation factors. We report a case of angiosarcoma of the scalp and face associated with Kasabach–Merritt syndrome and disseminated intravascular coagulation in a 78-year-old man.
A 78-year-old Chinese man presented with a mass and swelling on the scalp and forehead of 5 months duration. The patient was once treated with antibiotics and corticosteroid but the lesion continued to increase in size and gradually became more infiltrative.
On clinical examination, diffuse infiltrative violaceous plaques and nodules were noted on the scalp and forehead along with ecchymoses involving the left orbital and malar region [Figure - 1]. Histopathological examination revealed irregular vascular spaces lined by atypical endothelial cells and immunohistochemical examination showed positive staining for CD31, CD34 and factor VIII related antigen [Figure - 2]. Hematology investigations indicated thrombocytopenia with a platelet count of 30 × 109/L (normal: 100–300 × 109/L), hemoglobin 94 g/L (120–160 g/L), red blood cell count 2.5 × 1012/L (5.0–6.0 × 1012/L), mean corpuscular volume 107 fl (82–95 fl), mean corpuscular hemoglobin 36.9 (27–31 fl) and white blood cells 5.7 × 109/L (4–10 × 109/L). Coagulation profile showed fibrinogen 1.4 g/L (2.0–5.0 g/L), elevated D-dimer 5408 ng/ml (0–450 ng/ml), activity of factor VIII 69% and positive 3P test. Bone marrow examination showed an increased number of megakaryocytes indicating that thrombocytopenia was associated with peripheral platelet consumption. Computerized tomography showed hematoma and swelling of the scalp. Chest X-ray showed left sided pleural effusion. Liver and renal function tests were normal. Serum alpha-fetoprotein and carcinoembryonic antigen levels were normal. Autoimmune antibodies were negative.
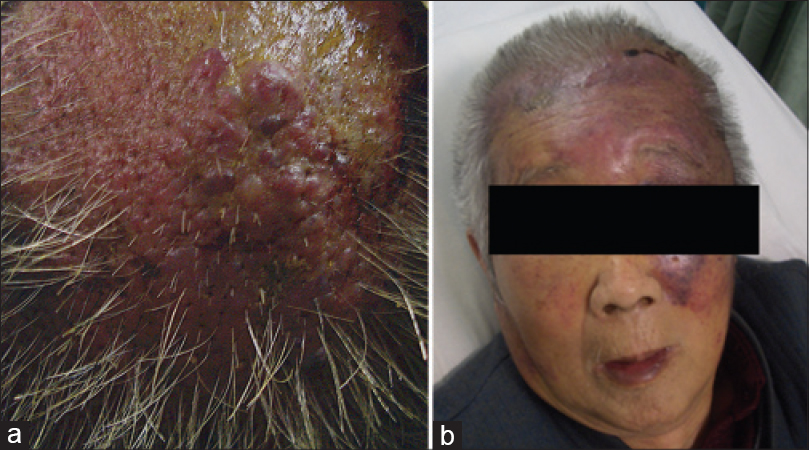 |
| Figure 1: Angiosarcoma manifesting as plaques and nodules on the scalp and face. (a) Infiltrative violaceous nodules on the scalp (b) diffuse and infiltrative violaceous plaques and nodules on the scalp and forehead with large ecchymoses around the left eyelid and malar region |
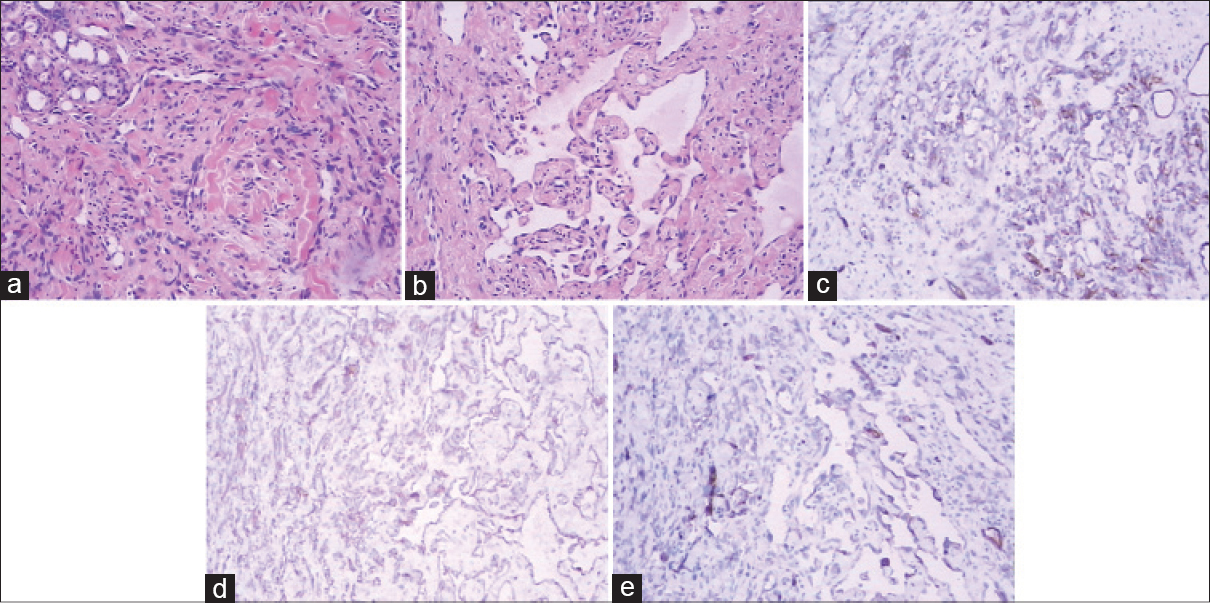 |
| Figure 2: Neoplastic infiltration in the dermis, composed of sheets of spindle cells (H and E, ×100). (a) The more differentiated parts of the tumor had irregular vascular spaces lined by atypical endothelial cells (H and E, ×100). (b) Atypical endothelial cells positive for CD31 (c), CD34 (d) and factor VIII related antigen (e) |
A final diagnosis of angiosarcoma of the scalp and face associated with Kasabach–Merritt syndrome and disseminated intravascular coagulation was made. The patient was treated with platelet transfusion and intravenous dexamethasone but the platelet counts still stayed at a low level. We assumed that disseminated intravascular coagulation might be improved by anti-angiosarcoma therapy. However, it was difficult to resect the angiosarcoma completely because of its large size. After consulting the oncologist, weekly paclitaxel (120 mg/week, 3 consecutive weeks) was initiated, combined with radiotherapy (amount of radiation: 30 Gy) of the scalp. Platelet counts were elevated to 62 × 109/L, but fibrinogen was still lower than normal level. D-dimer and 3P test were still positive. Unfortunately, the patient declined taking any treatment and eventually died of congestive cardiac failure.
The association of cutaneous angiosarcoma with Kasabach–Merritt syndrome, though rare, has been reported previously.[1],[2],[3],[4] The consumption coagulopathy which occurs in Kasabach–Merritt syndrome may be diverse, ranging from only mild thrombocytopenia and anemia to the development of disseminated intravascular coagulation. Imafuku et al. described a case of early stage angiosarcoma of the scalp associated with Kasabach–Merritt syndrome and disseminated intravascular coagulation.[3] Thrombocytopenia with increased megakaryocyte numbers in bone marrow may suggest the presence of idiopathic thrombocytopenic purpura. However, the presence of consumptive coagulopathy and anemia is not typical for idiopathic thrombocytopenic purpura. Thrombotic thrombocytopenic purpura was ruled out because renal function and body temperature were normal and neurological abnormalities were absent.
Treatment options include platelet transfusion, corticosteroids, interferon-γ, anti-fibrinolytic agents and anti-sarcoma treatments such as surgical resection, radiotherapy and chemotherapy, of which the anti-sarcoma treatments are the most important. Radiation therapy, which is known to prolong survival in angiosarcoma, could improve disseminated intravascular coagulation.[3],[5] It is also possible that chemotherapeutic agents including taxane and doxorubicin could relieve disseminated intravascular coagulation. Our patient was treated with corticosteroids, platelet transfusion, radiotherapy and chemotherapy and the disseminated intravascular coagulation improved to some extent.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Salameh F, Henig I, Bar-Shalom R, Maza I. Metastatic angiosarcoma of the scalp causing Kasabach-Merritt syndrome. Am J Med Sci 2007;333:293-5.
[Google Scholar]
|
| 2. |
Grellety T, Italiano A. Angiosarcoma associated with a Kasabach-Merritt syndrome: Report of two cases treated with paclitaxel. Future Oncol 2013;9:1397-9.
[Google Scholar]
|
| 3. |
Imafuku S, Hosokawa C, Moroi Y, Furue M. Kasabach-Merritt syndrome associated with angiosarcoma of the scalp successfully treated with chemoradiotherapy. Acta Derm Venereol 2008;88:193-4.
[Google Scholar]
|
| 4. |
Massarweh S, Munis A, Karabakhtsian R, Romond E, Moss J. Metastatic angiosarcoma and kasabach-merritt syndrome. Rare Tumors 2014;6:5366.
[Google Scholar]
|
| 5. |
Pawlik TM, Paulino AF, McGinn CJ, Baker LH, Cohen DS, Morris JS, et al. Cutaneous angiosarcoma of the scalp: A multidisciplinary approach. Cancer 2003;98:1716-26.
[Google Scholar]
|
Fulltext Views
2,998
PDF downloads
1,633





