Translate this page into:
Annular purpuric eruption in an adult male
2 Department of Pathology, University College of Medical Sciences and GTB Hospital, University of Delhi, Delhi, India
Correspondence Address:
Archana Singal
B-14, Law Apartments, Karkardooma, Delhi - 110 092
India
| How to cite this article: Sonthalia S, Singal A, Pandhi D, Singh UR. Annular purpuric eruption in an adult male. Indian J Dermatol Venereol Leprol 2011;77:731 |
Sir,
Purpuric pityriasis rosea, a rare variant of pityriasis rosea (PR), is characterised by the presence of purpuric lesions over the trunk and proximal limbs. While this atypical variant of PR is itself an uncommon entity, annular lesions have been described in even fewer cases. Annular purpuric eruption is also characteristic of purpura annularis telangiectoides of Majochhi (PATM) which should be considered in the differential diagnosis of purpuric PR. Since the course, prognosis, and management of the two conditions are remarkably different, their differentiation in an individual case is of vital importance.
We describe the case of a 35-year-old man who presented with progressive eruption of mildly itchy, dusky red lesions of 2 weeks′ duration that started on thighs and extended to involve the abdomen, back, and arms. There was no history of preceding fever, sore throat, arthralgia, recent drug intake, or any systemic complaints. Cutaneous examination revealed multiple, 1-3 cm sized round to oval, purpuric, maculopapular lesions over the trunk, arms, and thighs. Trunkal lesions were arranged along the skin cleavage lines [Figure - 1]. Many lesions were annular with mildly raised erythematous margins and flat rust-colored centers with mild scaling [Figure - 2]. A herald patch was not discernable. Peripheral lymph nodes were not enlarged. Mucosal and systemic examinations were normal. Clinically, differential diagnoses of purpuric PR, PATM, and cutaneous vasculitis were considered and lesional skin biopsies were performed for histopathology and direct immunofluorescence. Histopathological findings of mild spongiosis, dermal edema, superficial dermal perivascular lymphohistiocytic infiltrate with prominent extravasation of erythrocytes [Figure - 3] without evidence of capillaritis or vasculitis, and negative immunofluorescence confirmed the diagnosis of purpuric PR. Laboratory evaluation including complete blood count, hepatic and renal function tests, coagulation studies, anti-streptolysin antibody, VDRL, serology for HIV, and urinalysis revealed no abnormality. The patient was started on oral antihistamines and emollients. Over the next 4 weeks, new lesions developed and pruritus increased for which he was given 1% hydrocortisone acetate cream for twice-a-day application. All lesions cleared completely in the next two weeks without any recurrence.
 |
| Figure 1: Multiple round to oval purpuric lesions over the trunk arranged along skin cleavage lines |
 |
| Figure 2: Close-up of lesions over the thigh revealing annular lesions with erythematous margins and rust-colored centers |
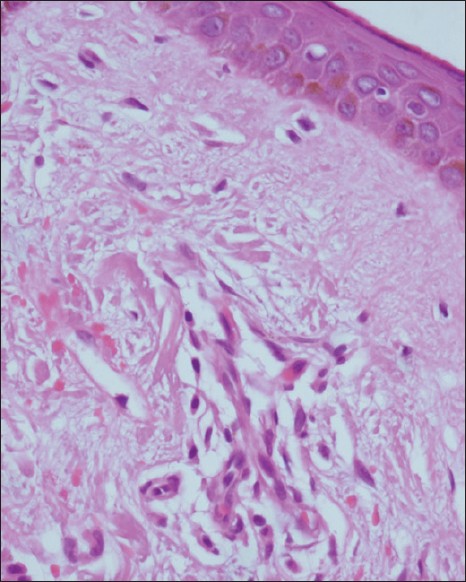 |
| Figure 3: Prominent extravasation of erythrocytes with moderate perivascular lymphohistiocytic infiltrate in superficial dermis without evidence of capillaritis (H and E, ×400) |
PR is an acute, self-limited dermatosis of unclear etiology seen most commonly in 10- to 35-year-olds with equal sex distribution. Many atypical variants of PR have been reported including papular, vesicular, urticarial, purpuric, inversus, and gigantea. [1] Purpuric PR, first described by Hartman in 1944, is a rare variant with less than 15 cases reported in English literature till now. [2],[3],[4],[5],[6] It is characterised by round to oval purpuric macules and papules over trunk and proximal aspect of limbs. Similar to classical PR, a herald patch may be present and lesions are often oriented along skin cleavage lines ("christmas tree" pattern).
In this case, many lesions showed annular morphology, a feature rarely described in purpuric PR previously. [3] Since similar lesions are also encountered in PATM, a variant of pigmented purpuric dermatosis (PPD), we considered it in the differential diagnosis. However, certain clinical and histological features helped in differentiation. While lesions are seen predominantly over the trunk and proximal limbs in purpuric PR, lower extremities are the favoured sites for PATM. [7] The "christmas tree" pattern is characteristic of PR and its purpuric variant. Atrophy of lesions observed in late stages of PATM is not seen in purpuric PR. In contrast to the self-limiting course of purpuric PR, lesions of PATM tend to persist with a remitting-relapsing course and are usually refractory to therapy. [7] Histologically, purpuric PR is characterised by patchy parakeratosis, spongiosis, dermal edema, superficial dermal perivascular lymphohistiocytic infiltrate, and extravasation of erythrocytes without evidence of capillaritis or vasculitis. [2],[3],[4],[5] While PATM and other PPDs show a similar histology, features suggestive of capillaritis are often seen like the presence of endothelial cell swelling in early stages and dilated capillaries with endothelial proliferation and hemosiderin-laden macrophages in older lesions. [8] In this case, the characteristic morphology of lesions, distribution over trunk and proximal extremities in a "christmas tree′′ pattern, and extravasation of erythrocytes without any evidence of capillaritis on histology prompted us to label it as purpuric PR.
The course and prognosis of purpuric PR have been described to be similar to classical PR. [2],[3],[4],[5] Therefore, Paller et al., [3] in their report of four cases, have suggested that detailed hematological evaluation in these patients is unnecessary. [3] However, Singal et al. [6] have described a case with purpuric PR-like eruption with underlying acute myeloid leukemia and emphasized the need of detailed hematological investigations. [6] In this case, no hematological abnormality was detected and the course was uneventful. While emollients and oral antihistamines are often the only treatment required for purpuric PR, low potency topical steroids may be added to control pruritus and to hasten the resolution of lesions.
| 1. |
Chuh A, Zawar V, Lee A. Atypical presentations of pityriasis rosea: Case presentations. J Eur Acad Dermatol Venereol 2005;19:120-6.
[Google Scholar]
|
| 2. |
Verbov J. Purpuric pityriasis rosea. Dermatologica 1980;160:142-4.
[Google Scholar]
|
| 3. |
Paller AS, Esterly NB, Lucky AW, Milstone EB, Higgins TP. Haemorrhagic pityriasis rosea: An unusual variant. Pediatrics 1982;70:357-9.
[Google Scholar]
|
| 4. |
Pierson JC, Dijkstra JW, Elston DM. Purpuric pityriasis rosea. J Am Acad Dermatol 1993;28:1021.
[Google Scholar]
|
| 5. |
Sezer E, Saracoglu ZN, Urer SM, Bildirici K, Sabuncu I. Purpuric pityriasis rosea. Int J Dermatol 2003;42:138-40.
[Google Scholar]
|
| 6. |
Singal A, Pandhi D, Rusia U. Purpuric pityriasis rosea-like eruption: A cutaneous marker of acute myeloid leukaemia. J Eur Acad Dermatol Venereol 2007;21:822-3.
[Google Scholar]
|
| 7. |
Hoesly FJ, Huerter CJ, Shehan JM. Purpura annularis telangiectodes of Majocchi: Case report and review of the literature. Int J Dermatol 2009;48:1129-33.
[Google Scholar]
|
| 8. |
Barnhill RL, Nousari CH, Xu X, Barksdale SK. Vascular diseases. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's Histopathology of the Skin. 10 th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 205-34.
th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 205-34.'>[Google Scholar]
|
Fulltext Views
3,708
PDF downloads
3,546





