Anti-neutrophil cytoplasmic antibodies-negative Churg–Strauss syndrome presenting as granuloma annulare-like lesions: An unusual cutaneous presentation and a diagnostic pitfall
Corresponding author: Dr. Weining Huang, Department of Dermatology, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou 510120, P.R. China. 2282233580@qq.com
-
Received: ,
Accepted: ,
How to cite this article: Zhu H, Huang M, Huang W. Anti-neutrophil cytoplasmic antibodies-negative Churg–Strauss syndrome presenting as granuloma annulare-like lesions: An unusual cutaneous presentation and a diagnostic pitfall. Indian J Dermatol Venereol Leprol 2021;87:259-62.
Sir,
A 35-year-old male complained of generalized skin rashes. Four years prior to admission to our hospital, the patient had many skin-colored papules on his trunk, limbs and extremities, which were diagnosed as papular granuloma annulare by histological examination at another hospital. The gradual increase in respiratory distress started 6 months prior to admission. It was interpreted as asthma but had no response to inhaled combined steroid therapy and long-acting bronchodilators. Progressively, the patient had visual deterioration and developed tingling with a sensation of numbness of both legs, extending from the posterior thighs to the feet. The patient had a history of sinusitis for more than 10 years and Raynaud’s phenomenon since the previous 7 years.
Dermatological examination showed symmetrical skin-colored and solid papules with a diameter of 0.3–0.5 cm with smooth surface, over his face, neck, trunk, limbs and extremities [Figure 1], without any pustules, ulcers, wheals or purpura. The right upper and lower eyelids were swollen. On respiratory examination, tachypnea and wheezing was noted. Computed tomography scan of the chest showed bronchial thickening, centrilobular nodules, bilateral ground-glass opacity, and tumescent lymph nodes at lung hilus and mediastinum. Sinus computed tomography scan revealed bilateral maxillary, ethmoidal and sphenoidal sinusitis. Ultrasonography showed bilateral cervical lymphadenopathy.
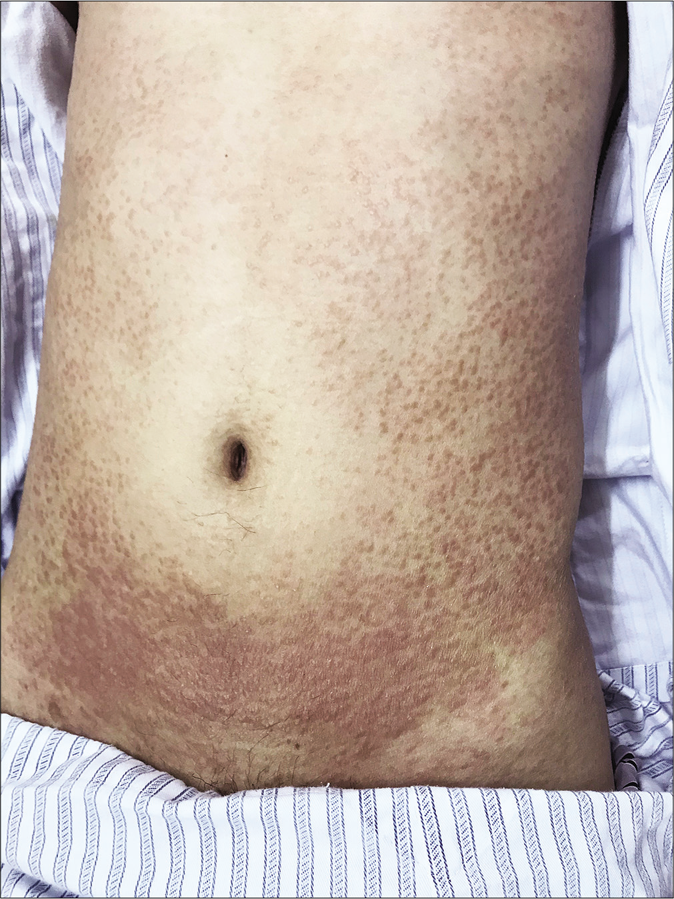
- Cutaneous lesions presenting as solid, symmetrical, generalized, skin-colored papules on torso

- Cutaneous lesions presenting as solid, symmetrical, generalized, skin-colored papules on left flank and trunk

- Cutaneous lesions presenting as solid, symmetrical, generalized, skin-colored papules on the limb

- Cutaneous lesions presenting as solid, symmetrical, generalized, skin-colored papules on left foot
Complete blood count revealed leukocytosis (24,300/mm3), and marked eosinophilia (15,090 cells/mm3). Elevated immunoglobulin E (716 IU/mL), erythrocyte sedimentation rate (98 mm/h) and C reactive protein level (14.1 mg/dL) were present. Anti-neutrophil cytoplasmic antibodies, antinuclear antibody, and antinuclear antibody profiles were negative. Liver and renal function tests indicated normal levels.
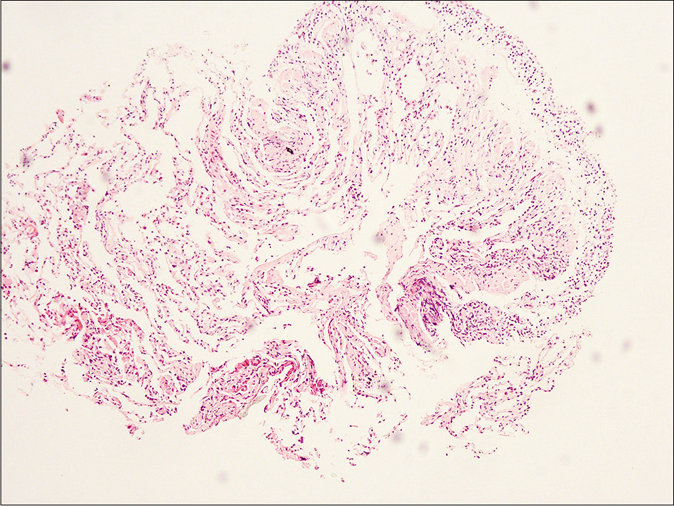
Skin biopsy (hematoxylin-eosin stain) revealed perivascular lymphohistiocytic infiltrate with multinuclear giant cells and eosinophils in the superficial and middermis. There were some lymphohistiocytes scattered between and around the collagen bundles [Figure 2]. Collagen degeneration, dermal mucin, fibrinoid necrosis of the vessel wall, neutrophils or neutrophilic fragments were not observed. Histopathology was reviewed in another hospital and similar findings were reported. Percutaneous lung biopsy revealed diffuse infiltration of lymphohistiocytes and eosinophils in the alveolar septa [Figure 3]. Bone marrow biopsy ruled out any hematologic malignancies.
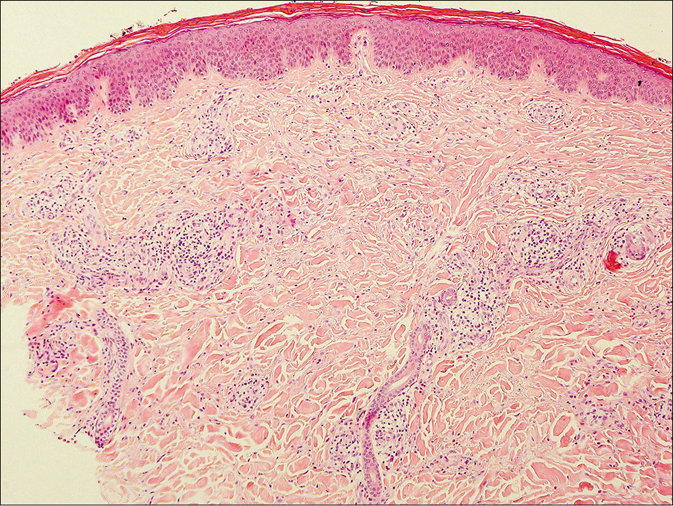
- Lymphohistiocytes, multinuclear giant cells and eosinophils infiltrating around vessels and scattered between the collagen bundles (H and E, ×100)
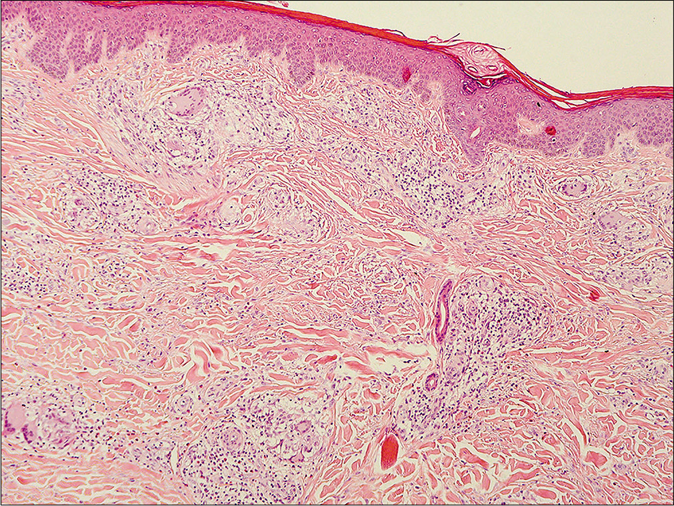
- Lymphohistiocytes, multinuclear giant cells and eosinophils infiltrating around vessels and scattered between the collagen bundles -- another view (H and E, ×100)
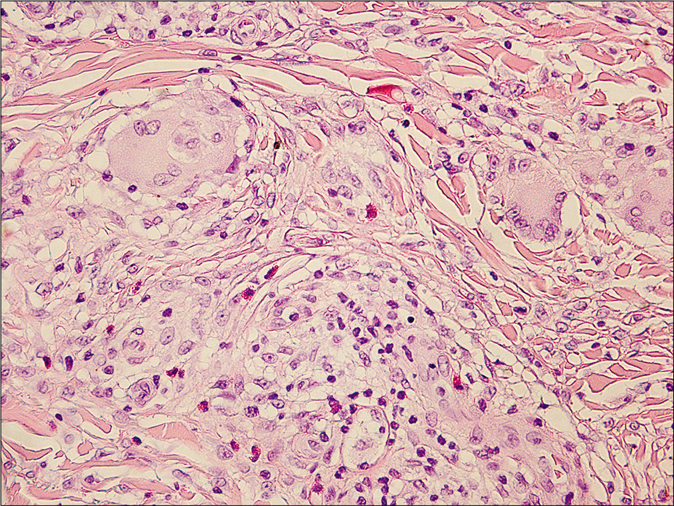
- Lymphohistiocytes, multinuclear giant cells and eosinophils infiltrating around vessels and scattered between the collagen bundles - high power view (H and E, ×400)
- Lymphohistiocytic infiltrate with eosinophils in the alveolar septa (H and E, ×100)
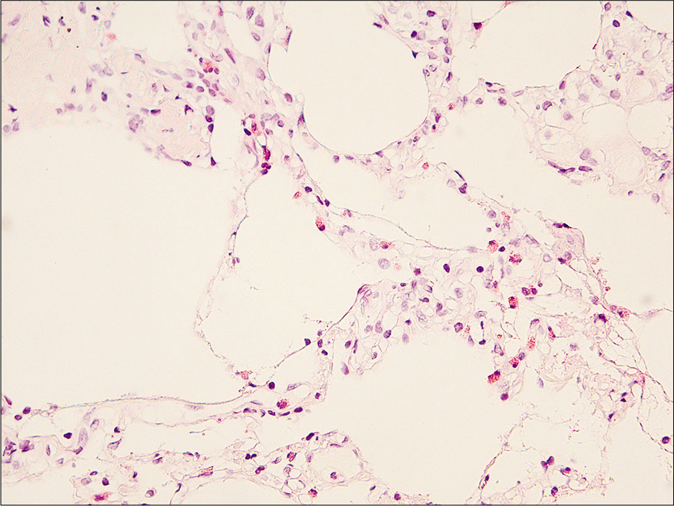
- Lymphohistiocytic infiltrate with eosinophils in the alveolar septa - high power view(H and E, ×400)
The patient was thus diagnosed with Churg–Strauss syndrome. He was transferred to the respiratory department. Treatment was started with intravenous injection of methylprednisolone (80 mg/d, with decreasing doses) and pulse doses of cyclophosphamide (800 mg once monthly). He displayed gradual improvement in the skin lesions, respiratory distress, tingling sensation and swelling of the eyelids. Unfortunately, he was lost to follow-up 3 months after treatment was initiated.
According to the American College of Rheumatology, Churg–Strauss syndrome can be diagnosed by the presence of any four or more of the following six criteria: asthma, eosinophilia (>10%), neuropathy, migratory pulmonary infiltrates, paranasal sinus abnormalities, and biopsy-proven extravascular eosinophils.1 The patient fulfilled all six diagnostic criteria in our case. This case presented with five clinical manifestations: respiratory distress, sinusitis, polyneuropathy, skin lesions and ocular involvement. Radiologic, laboratory and histological examinations verified five factors: marked eosinophilia, elevated immunoglobulin E, lymphadenopathy, pulmonary infiltration and extravascular eosinophilic infiltration with granulomatous inflammation in the skin lesions. Although orbital involvement is not common, it has been reported in literature. The swelling of the right eyelid was considered as one of the presentations of Churg–Strauss syndrome after exclusion of angioedema, orbital complications secondary to sinusitis and thyroid eye disease.
The typical skin changes in Churg–Strauss syndrome are palpable purpuras, petechiae, ecchymoses, hemorrhagic vesicles and bullae.2 Less frequently, erythematous and purpuric papules with overlying erosions or crusts, confined to the extensor surfaces of the extremities can also be observed.3
We were unable to find any previous reports of cutaneous lesions presenting as symmetrical and generalized papules. In our case, the patient presented with multiple skin-colored papular lesions all over his body, which resembled the cutaneous manifestation of generalized papular granuloma annulare. Isolated and generalized papular presentation without typical cutaneous manifestations in Churg–Strauss syndrome is a rare skin change and may mislead the dermatologist.
The most common pathological characteristics of Churg–Strauss syndrome are extravascular necrotizing granulomas and leukocytoclastic vasculitis.2 There is no single type of vasculitis that appears consistently in such cases. A case presenting with only extravascular granulomas and eosinophils but with the absence of vasculitis has been reported.4 The cutaneous biopsy in our case showed not only perivascular lymphohistiocytes infiltrating with multinuclear giant cells and eosinophils but also interstitial granulomas. On the other hand, the interstitial pattern of histiocytic infiltration is the most common pattern in granuloma annulare, and a number of previous studies have found eosinophils in the cases of this disease.5 However, no collagen degeneration or dermal mucin was observed in our case, which was common in granuloma annulare.5
Eruptive xanthoma, xanthoma disseminatum and Wegener’s granulomatosis were also considered and excluded according to the clinical characters and the results of radiologic, laboratory and histological examination. Isolated and generalized papular presentation is normal in eruptive xanthoma and xanthoma disseminatum however, the histological findings of our case showed extravascular eosinophilic infiltration with interstitial granulomas. No foam cells or extracellular lipid, which are present in eruptive xanthoma and xanthoma disseminatum were abserved. No similar cutaneous manifestations like our case were found in literature in Wegener’s granulomatosis.
Acknowledgment
The authors will thank Professor Baoqing Sun in Guangzhou institute of Respiratory Disease for her great help in this case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis) Arthritis Rheum. 1990;33:1094-100.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous manifestations of Churg-Strauss syndrome: A clinicopathologic correlation. J Am Acad Dermatol. 1997;37:199-203.
- [CrossRef] [Google Scholar]
- Cutaneous manifestations of Churg-Strauss syndrome: Key to diagnosis. An Bras Dermatol. 2017;92:56-8.
- [CrossRef] [PubMed] [Google Scholar]
- Granuloma annular-like lesions as a manifestation of eosinophilic granulomatosis with polyangiitis. Rheumatol Clin. 2017;13:357-8.
- [CrossRef] [Google Scholar]
- Evaluating the unusual histological aspects of granuloma annulare: A study of 30 cases. Indian Dermatol Online J. 2018;9:409-13.
- [Google Scholar]





