Translate this page into:
Application of a “fish mouth flap” combined with an orbicularis oculi myocutaneous flap after surgical removal of basal cell carcinoma in the facial buccal region
2 Department of Plastic Surgery, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA
Correspondence Address:
Hai Long
Department of Dermatology, Medical Cosmetic Center, The Second Xiangya Hospital, Central South University, Changsha, Hunan 410011
China
| How to cite this article: Fu S, Panayi AC, Lu Q, Long H. Application of a “fish mouth flap” combined with an orbicularis oculi myocutaneous flap after surgical removal of basal cell carcinoma in the facial buccal region. Indian J Dermatol Venereol Leprol 2019;85:649-652 |
Sir,
Basal cell carcinoma (BCC) is a slow-growing, locally invasive malignant skin tumor mostly seen in the facial buccal area consistent with the embryological median line. Surgical excision of the tumor is the mainstay of treatment. We propose a modified “fish mouth flap” combined with the orbicularis oculi myocutaneous flap for cosmetic restoration after surgical removal of buccal BCC.
From July 2013 to October 2017, 25 patients (13 males and 12 females) presenting with a BCC in the facial buccal region in close proximity to the nose and lower eyelid were treated. The mean age was 67 years (44–82 years), and the average size of the tumor was 2.24 × 1.55 cm, ranging from 1.0 × 0.8 cm to 3.5 × 1.55 cm. The course of the disease ranged from 2 to 20 years. All patients were diagnosed with BCC by pathological examination and treated with extended resection under local anesthesia. The indolent-growth subtypes (nodular and superficial) and smaller tumors (<2 cm) were treated with extended 0.3–0.5 cm resections, while the aggressive-growth subtypes (morpheaform, infiltrative, micronodular and basosquamous) and larger tumors (>2 cm) were treated with extended 0.5–1.0 cm resections.[1] All patients underwent Mohs surgery to make sure that the lesional tissues were completely cleared [Figure - 1]a, [Figure - 1]b, [Figure - 1]c.
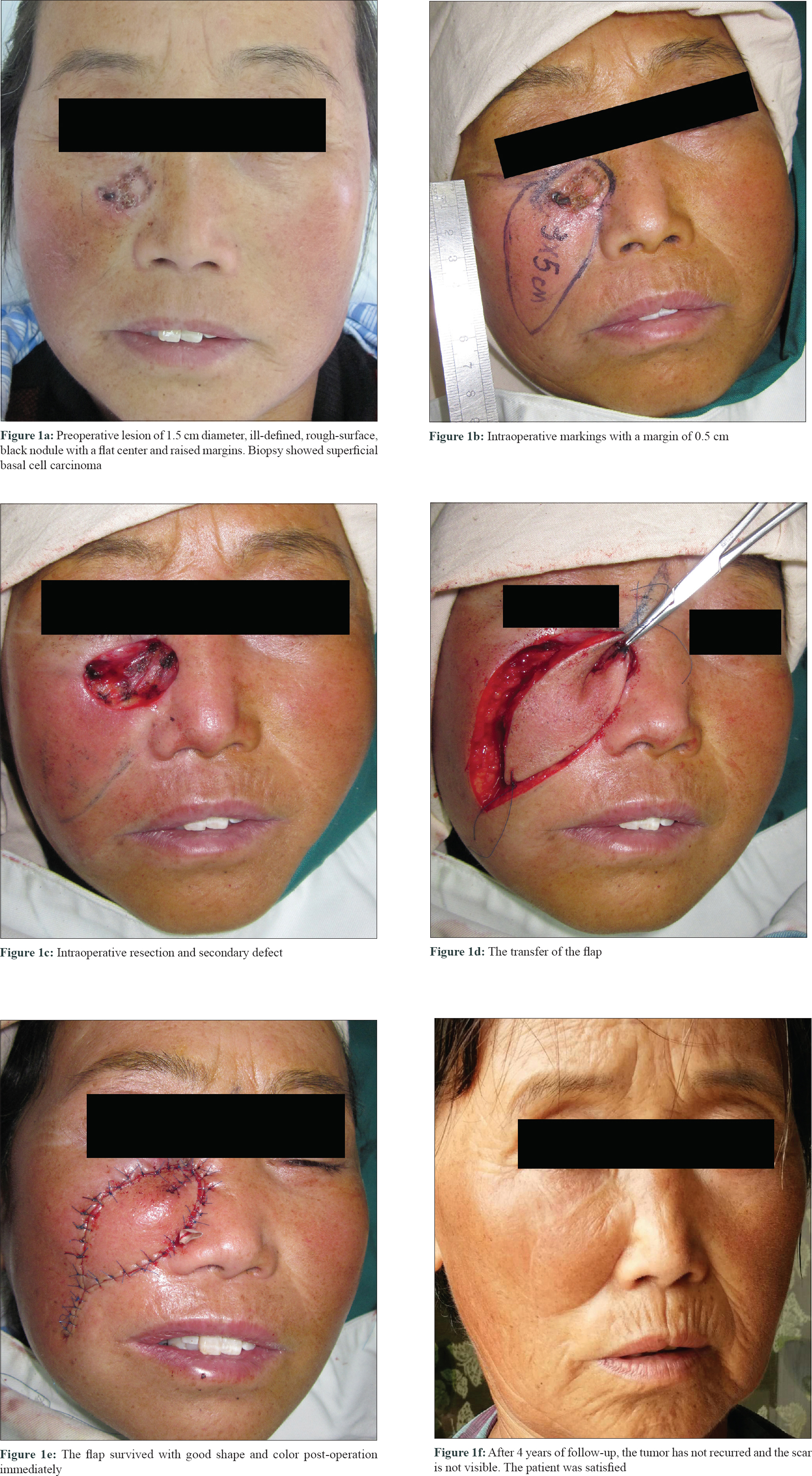 |
| Figure 1: |
The flap was marked on the skin at the lower border and on both sides of the defect. The lower flap corresponded to the “fish body,” while the two sides were “the upper and lower lip of the fish mouth” [Figure - 2]a and [Figure - 2]b. The length of the flap was approximately twice the length of the defect. The tip of the upper and lower lip did not need to be too sharp [Figure - 1]b. The skin and subcutaneous tissue were dissected above the deep fascia surface and the upper lip contained the orbicularis oculi muscle to ensure maximum blood supply. The “fish body” was then stretched to allow advancement and the upper and lower lip flaps of the “fish mouth” were rotated and promoted to cover the wound. The process was similar to the closure of the upper and lower lips, just as the term “fish mouth flap” describes it [Figure - 1]d. Subcutaneous tension and interrupted suturing of the skin was then performed. Finally, Vaseline gauze and a cotton pad were used to dress the surgical area [Figure - 1]e.
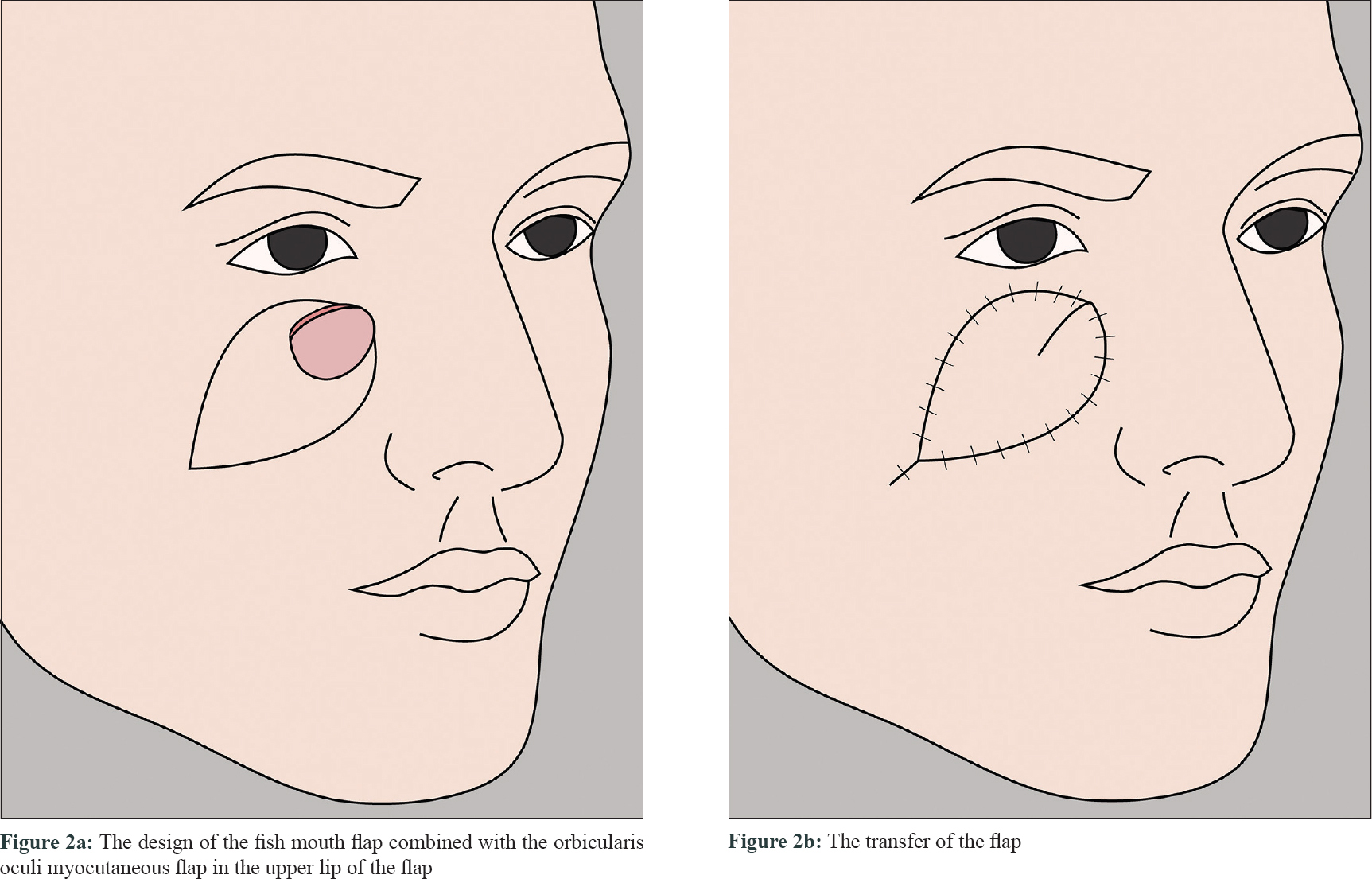 |
| Figure 2: |
All 25 flaps survived with primary healing. The patients were followed up from 6 months to 4 years. No deformation of the lower eyelid and nose was observed and scarring was minimal. The flaps showed adequate matching with the recipient site, in terms of both color and texture. All patients were satisfied with the surgical results [Figure - 1]f.
The occurrence of a BCC is more common in middle-aged and elderly people, with the predilection site at the head-and-neck region. The treatment method varies with factors that can potentially influence the prognosis, such as the tumor size, location and histological type.[2] The lower eyelid and paranasal region are high-risk areas of this tumor. Apart from complete removal of the lesion, attention should be paid to cosmetic satisfaction and the function of the eyelid and nose. Flap transfer is a method that allows for adequate cosmetic and functional restoration.
The “fish mouth flap” described in this study is a type of modified V-Y flap, a combination of the advancement flap and rotation flap.[3] Ellabban and Bremner used fish mouth flap to repair the postexcision defect of a squamous cell carcinoma on the back of the thigh with good results.[4] When using it on the facial buccal region, one should pay attention to the following technical aspects: (1) detaching in the nasolabial groove area should avoid injuring the perforating branch of facial vessels; (2) to maintain adequate blood supply to the flap lip, the orbicularis oculi muscle with multisource blood supply should be included in the upper lip of the fish mouth flap;[5] ( 3) the excision line should be marked on the margin of an aesthetic unit to prevent the trap-door deformity which is more likely to occur in younger patients.
A limitation of our reported technique is that it is not suitable for tumors involving the nasal dorsum or nasal root. Moreover, it is not suitable when the tumor involves the lower palpebral margin. Nevertheless, for a tumor located in the buccal region near the lower eyelid and paranasal area, our method provides a simple, yet effective technique for the cosmetic restoration of a postexcision skin defect.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported in part by the National Natural Science Foundation of China (81773334), Natural Science Foundation of Hunan Province (2018JJ3756), Hu-Xiang Talents Program of Science-Technology Department of Hunan Province (2018RS3031), and Outstanding Innovation Talents Program of Changsha Science-Technology Bureau (kq1802002).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Trakatelli M, Morton C, Nagore E, Ulrich C, Del Marmol V, Peris K, et al. Update of the European guidelines for basal cell carcinoma management. Eur J Dermatol 2014;24:312-29.
[Google Scholar]
|
| 2. |
Marzuka AG, Book SE. Basal cell carcinoma: Pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med 2015;88:167-79.
[Google Scholar]
|
| 3. |
Niranjan NS, Price RD, Govilkar P. Fascial feeder and perforator-based V-Y advancement flaps in the reconstruction of lower limb defects. Br J Plast Surg 2000;53:679-89.
[Google Scholar]
|
| 4. |
Ellabban MG, Bremner N. 'Fish mouth' modification for enhancing the advancement of V-Y flap. J Plast Reconstr Aesthet Surg 2007;60:213-5.
[Google Scholar]
|
| 5. |
Li XQ, Wang JQ. Orbicularis oculi myocutaneous flap for upper cicatricial ectropion. J Craniofac Surg 2016;27:70-3.
[Google Scholar]
|
Fulltext Views
4,391
PDF downloads
2,194





