Translate this page into:
Argyria an unrecognized cause of cutaneous pigmentation in Indian patients: A case series and review of the literature
Correspondence Address:
Meenakshi Batrani
Delhi Dermatology Group, 10, Aradhana Enclave, R.K. Puram, Sector 13, New Delhi - 110 066
India
| How to cite this article: Kubba A, Kubba R, Batrani M, Pal T. Argyria an unrecognized cause of cutaneous pigmentation in Indian patients: A case series and review of the literature. Indian J Dermatol Venereol Leprol 2013;79:805-811 |
Abstract
Argyria is an uncommon grey-blue pigmentation of skin and mucous membranes caused by prolonged silver exposure. The impetus behind this review is our experience with cases of generalized argyria resulting from a uniquely Indian socio-cultural practice and belief that it is under reported. Our objective is to increase the awareness for this esoteric entity through a review of the pertinent literature and to highlight clinical and histological features using our four well worked-up cases as examples.Introduction
Silver-the metal
Silver is a naturally occurring metallic element that has no known physiological or biological function in the human body. It is present widely in the human environment; henceforth, low concentrations are also present in the human body. Normal healthy people have silver levels of <3 μg/L. [1]
Toxicity and metabolism of silver
The ability of a metal to produce toxic effects on body depends on the type of compound/form of the metal, the amount and mode of absorption, its metabolism in the body and the cellular vulnerability to toxic damage. [1],[2] Absorption of metallic silver is much less when compared with soluble silver compounds. [2] Silver is absorbed into the body through inhalation, ingestion, intraparentaral through insertion of needles or implantation of medical devices or accidental puncture wounds and through dermal or mucosal contact. [1],[2] The percutaneous absorption through intact skin is very low, however, in wounds and burns the absorption increases significantly. [1],[3] The metallic and inorganic silver compounds ionize to silver ion on exposure to body fluids, which after absorption in the systemic circulation by ion uptake binds to thiol and proteins ligands such as metallothioneins, albumins and macroglobulins and is metabolized. [1],[4]
The acute toxicity due to exposure to large doses of inorganic silver salts such as silver nitrate is similar to corrosive effects leading to irritation of the gastrointestinal tract (if ingested) manifested in the form of epigastric burning, vomiting and diarrhea or respiratory tract irritation (if inhaled), severe toxicity will cause decreased blood pressure and decreased respiration ultimately leading to convulsions and shock. [2],[3],[5] Instillation of silver nitrate in the renal pelvis or urinary tract for chyluria have been reported to be associated with renal and hepatic failure, acute necrotizing ureteritis, obstructive nephropathy and papillary necrosis. [1] The corrosive effects are likely to be due to the nitrate in the compound rather than by the silver itself. [2] Organic silver compounds such as colloidal silver are less toxic however consumption of large doses of colloidal silver may lead to coma, pleural edema and hemolysis. [5]
The chronic toxicity occurs after prolonged exposure when the absorption of silver exceeds body metabolizing capacity leading to precipitation as inert silver sulfide and/or silver selenide in soft- tissues [1] (with highest concentrations in skin, liver, spleen and adrenal glands). [3] The chronic toxicity is not associated with an irreversible toxic damage to organs or carcinogenicity and the principal clinical manifestation is disfiguring cutaneous pigmentation called argyria or corneal/conjunctival pigmentation called argyrosis. [1]
Several safe limits set up by different regulatory authorities exist for silver depending upon the form of silver and mode of exposure. For occupational exposure a recommended exposure limit of 0.01 mg/m 3 in the air for both metallic and soluble compounds of silver and two separate exposure limits of 0.1 mg/m 3 for metallic silver and 0.01 mg/m 3 for soluble silver compounds are established by The National Institute for Occupational Safety and Health and The American Conference of Governmental Industrial Hygienists respectively. [2] A chronic oral reference dose of 5 μg/kg/day is given by The environmental protection agency. [3] World Health Organization limits are up to 0.1 mg/L for drinking water levels and total lifetime oral intake of 10 g for no observable adverse effect levels. [1] However, it is difficult to determine the lowest dose of silver leading to argyria because various studies have not been able to establish a clear relationship between exposure to silver, blood silver levels or minimal body silver concentrations with early signs of the condition. [1]
Pathogenesis of argyria
The photocatalyzed reaction analogous to developing a photographic film is the underlying mechanism behind the discoloration of argyria seen preferentially in sun exposed areas. [2] Recently, Liu et al. have proposed a conceptual model for pathogenesis of argyria. Sunlight catalyzes the silver complexes in the skin to elemental silver, which spontaneously forms the immobile silver nanoparticles. This is followed by transformations of silver nanoparticles into sulfides and further into selenides or Se/S mixed phases through exchange reactions. [4] In addition, silver also stimulates melanin production thus adding to the discoloration. [2]
Case Report
A total of 4 patients, of these 1 were male and 3 were female presented with insidious onset grey-blue macular shiny pigmentation involving predominantly sun exposed areas [Figure - 1] and [Figure - 2]. Nail involvement (azure lunulae) was observed in two patients [Figure - 3] while discoloration of the oral mucosa was present in one patient. The cause of argyria was elucidated to be long-term ingestion of silver coated cardamoms in two and silver coated betel nut in other two [Table - 1].

 |
| Figure 1: (a) Diffuse slate-grey pigmentation with accentuation along nasolabial folds and forehead. (b) Pigmentation of pinna and neck |
 |
| Figure 2: Shiny diffuse ash-blue pigmentation |
 |
| Figure 3: Azure lunulae (nail pigmentation) |
Histopathological examination showed similar features in all patients. The distinctive feature observed was deposition of fine black granules in the basement membrane of eccrine secretory coils [Figure - 4], blood vessels wall, around pilosebaceous units and along the elastic fibers of the papillary dermis [Figure - 5]. The granules were refractile under dark field microscopy [Figure - 6]. Masson-Fontana and Perl′s stain were performed to exclude melanin and hemosiderin granules respectively.
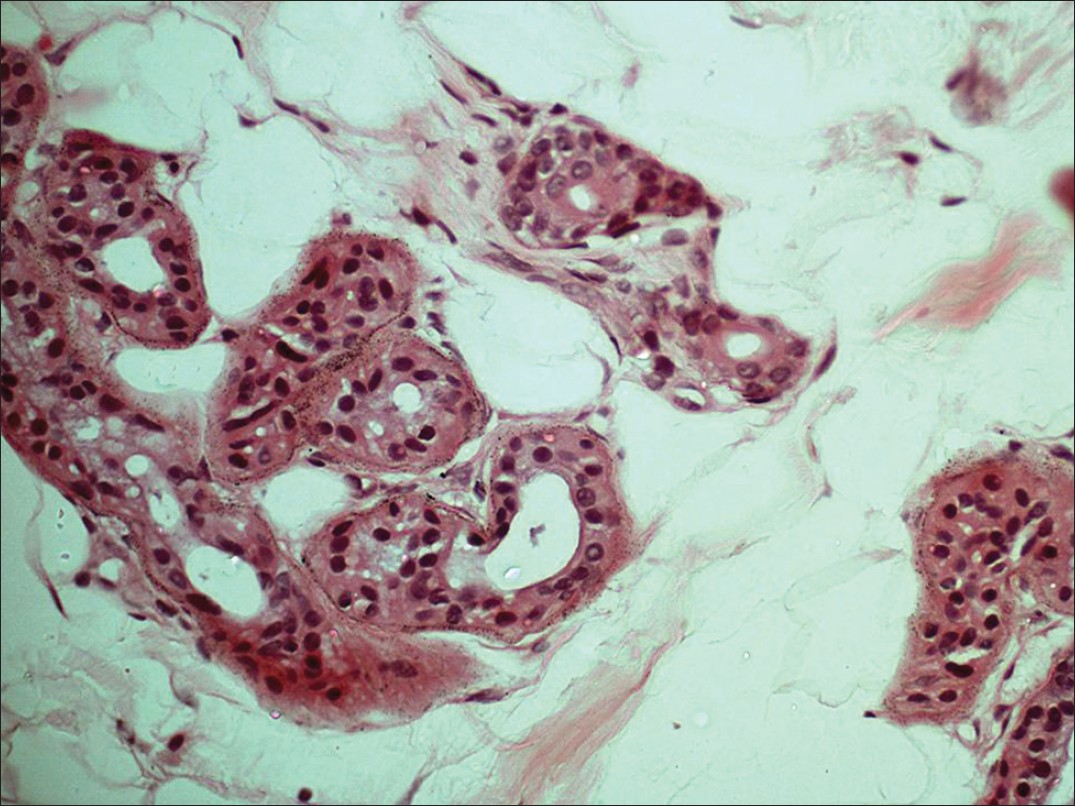 |
| Figure 4: Fine black granules of silver in eccrine gland basal lamina (H and E, ×400) |
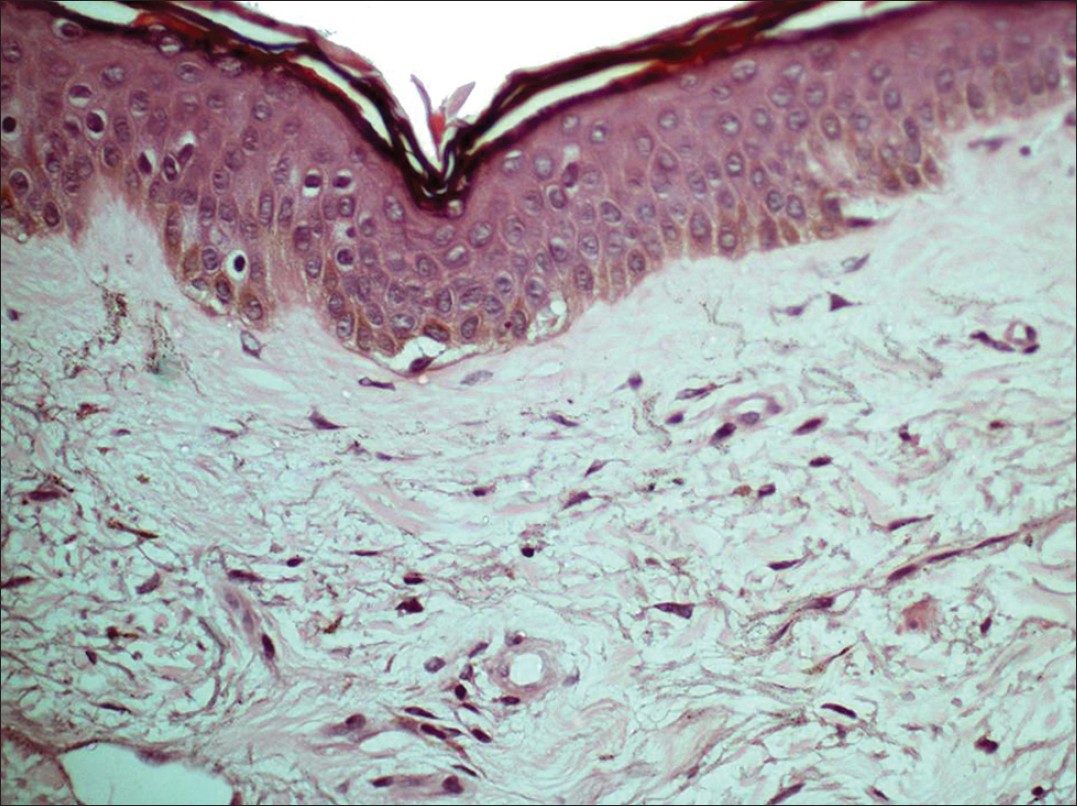 |
| Figure 5: Fine black granules of silver along the elastic fibers in papillary dermis (H and E, ×400) |
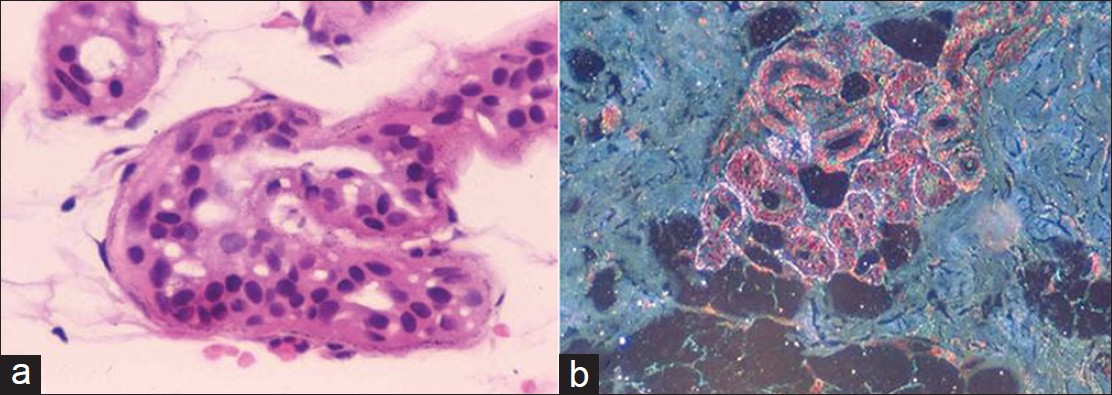 |
| Figure 6: (a) Silver granules along eccrine glands not prominent under light microscopy, (H and E, ×400). (b) Brightly refractile silver granules under dark field microscopy (H and E, ×400) |
Discussion
Silver deposition leading to pigmentation had been recorded as early as 8 th century. The term "argyria" was coined by Fuchs in 1840. [5] It was prevalent in 19 th and early 20 th century. [6]
Argyria can be localized or generalized, depending upon the mode and amount of silver absorbed. Localized argyria is the pigmentation of skin or mucous membranes due to impregnation of silver confined to the site of direct contact. [2] Besides the commonly characterized forms of localized argyria i.e., cutaneous, ocular (argyrosis) and oral cavity (amalgam tattoo), some unusual locations of localized argyria are nasal mucosa, [7] trachea, [8] urinary tract, [9] vagina, [10] and penis. [11] In generalized argyria, the silver is systemically absorbed and is widely deposited in skin, eyes, mucous membranes and nails. [2]
Etiological factors
Occupational
Silver, apart from its wide usage in jewelry and silverware, has extensive industrial applications including photography, soldering, in batteries, in mirrors to name a few. [2] Silver exposure in miners and other occupations as the cause of argyria, especially generalized, has become less prevalent due to availability as well as enforcement of better protective measures at work place. [2] However, isolated cases of occupational argyria mostly localized [7],[12],[13],[14],[15],[16] and rarely generalized [17] continue to be recorded. Some interesting reports of occupation related argyria cited in the literature include black tears as a result of occupational inhalation of silver, [18] localized argyria in an antique restorer [19] and localized cutaneous argyria in a dental surgeon called as cutaneous amalgam tattoo by the authors. [20]
Medicinal and therapeutic
Silver has had medicinal uses since ancient times. Historically, silver nitrate was used for neurological disorders such as epilepsy and tabes dorsalis. In the late 19 th and early 20 th century, silver compounds and colloidal silver proteins for their antimicrobial, caustic, astringent and hemostatic properties had varied spectrum of usage. Silver compounds were used for treatment or prevention of infectious diseases like gonorrhea including Crede′s method for ophthalmia neonatorum and syphilis, gastrointestinal disorders, oral ulcers, for removal of warts and for bladder irrigation. Silver was also used in allergy and cold remedies, eye drops, nasal sprays, lozenges and antismoking pills. [2],[3],[5],[9],[21] Thus, the medical exposure was the most common source of argyria. [2],[3] With the development of antibiotic and better pharmaceutical agents the medicinal use of silver declined. [2],[5] In 1999, US Food and Drug Administration prohibited the sale of over the counter (OTC) medications containing silver. [5]
In present day medicine, the use of silver is mainly confined to silver dressings for burns/wound management and in medical appliances. [3],[21] The silver dressings have come a long way from silver foils to popular silver sulfadiazine cream to present day nanocrystalline dressings. [5],[21] The spectrum of silver based medical appliances has also evolved from silver wire sutures to various other devices such as prosthetic implants, splints, catheters, heart valve, stents, bone cement, dental fillings. [1],[21] The incidence of argyria with these forms of applications is low, however, localized argyria has been reported with the use of silver dressings/cream [10],[11],[22],[23],[24] and with the implantation of medical devices. [8],[25],[26],[27] Rarely generalized argyria has been documented either with prolonged use of silver dressings/cream or application over large body surface area such as in cases of burns, epidermolysis bullosa and venous leg ulcers. [10],[28],[29],[30]
Recently, there has been a resurgence in the unregulated use of silver in the form of dietary supplements and as a constituent of alternative medicine/home remedies. [2],[5] There are hundreds of websites proclaiming the benefits of silver compounds. [2],[5],[31],[32],[33] Most of the reported cases of generalized argyria in the 21 st century have been associated with long-term and indiscriminate use of these preparations. [5],[6],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41],[42],[43],[44],[45],[46],[47],[48],[49],[50],[51],[52] It is worth mentioning herein, two reports of familial argyria in members of the same family due to prolonged use of silver containing formulations as a form of alternative medicine. [53],[54] Apart from this, localized cases of argyria have also been reported following acupuncture. [55],[56],[57]
Personal and socio-cultural
Cases of argyria have been associated with certain personal and socio-cultural practices. Examples include argyria associated with the use of mouth fresheners [55],[58],[59],[60] and sugar coated particles. [61] Silver earrings [62],[63] and eyelash dye [64] have led to localized argyria. Generalized argyria cases have been reported in psychiatric illnesses, such as, schizophrenia, [58] somatic delusions, [31],[51] schizoaffective disorder [52] and due to chewing of photographic film. [65]
Environmental and incidental
Localized argyria has occurred due to chemical explosion, [66] and trauma. [67],[68] Contaminated water used in hemodialysis has led to generalized argyria. [69]
Clinical features
In general, the macular pigmentation in argyria is slate - grey. It arises insidiously and is asymptomatic. The pigmentation is subtle and goes unrecognized for months and years. [6],[32],[33],[46] It is more pronounced on sun exposed areas including face, neck, [Figure - 1] arms and dorsum of the hands. [2] It is often viewed by the patient as persistent tan. However, the clinical morphology and anatomic pattern is sufficiently distinctive as exemplified by our four patients. The shiny quality of pigmentation [Figure - 2] and the diffuse pattern is in contrast to brown-black patchy pigmentation of melasma. Mucosal/conjunctival involvement and azure lunulae (nails) [Figure - 3] are characteristic attributes of argyria. In our opinion, with knowledge and awareness, argyria can be clinically recognized.
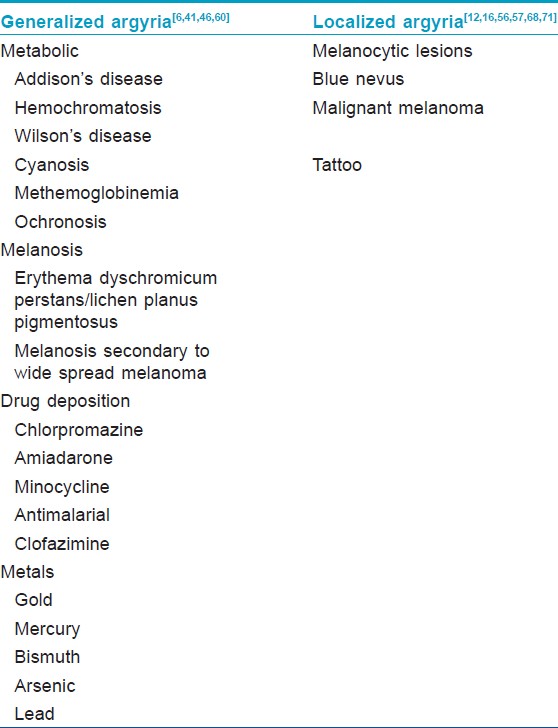
Clinical differential diagnosis of argyria includes other causes of cutaneous discoloration [Table - 2]. Generalized argyria can closely mimic metabolic causes of pigmentation, which too are uncommon and only a thorough clinical work-up will allow the correct diagnosis to be arrived at. Generalized argyria has been mistaken for cyanosis in individuals of light skin. [32],[41],[70] The localized argyria needs to be distinguished from melanocytic lesions like blue nevi [12],[57],[68] and malignant melanoma. [12],[16],[56],[71]
An exhaustive history is necessary for eliciting the mode and duration of silver exposure. At times, the exposure to silver may not be readily apparent as is evident from a reported case of generalized argyria caused by silver element in a tea kettle. [70]
Histological features
Argyria appears as invisible dermatosis under scanning magnification. Diagnostic features seen on high power are characterized by the deposition of uniform fine brown black granules in the basal lamina of the secretory portion of eccrine glands [Figure - 4], blood vessel walls and elastic fibers of the papillary dermis [Figure - 5]. To a lesser extent deposits are also seen in connective tissue sheath surrounding pilosebaceous units, perineural tissues and arrector pili muscles. [12],[72] Dark field microscopy under which the granules are brightly retractile is particularly useful in suspected cases of argyria where the deposits are not evident under light microscopy [Figure - 6]. In localized argyria an unusual histological finding of yellow brown collagen bundles similar to pseudo-ochronosis has occasionally been described. [12],[56]
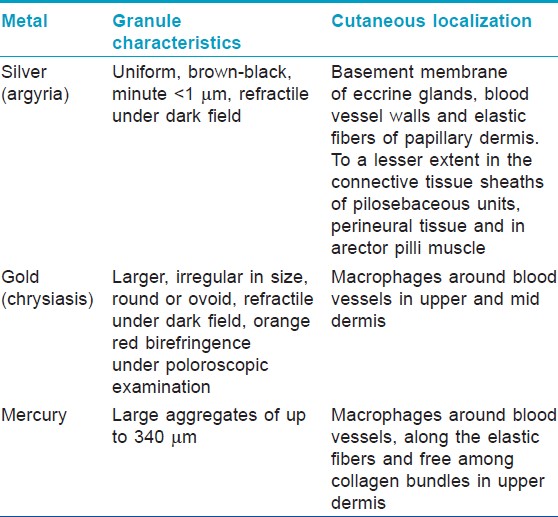
Histopathological examination is important to establish the definite diagnosis and to exclude other causes of pigmentation because these have significantly different implications from the management and prognostic point of view. The cutaneous deposits can be histochemically characterized as silver compounds by techniques such as transmission electron microscopy with electron loss spectroscopy or scanning electron microscopy with energy dispersive radiograph microanalysis. [73] However, these techniques are not readily available, in this setting, the specific characteristics and the localization of the silver granules as observed under light microscopy with dark field microscopy can distinguish it from some of the other common heavy metal granules [Table - 3]. [12],[72],[74]
Management
Cessation of silver exposure and sun-protection with sunscreen are useful for preventing further progression of pigmentation. Various treatment options such as chelation, hydroquinone and dermabrasion are not effective. Recently, Q-switched 1064-nm neodymium-doped yttrium aluminium garnet laser has been reported to be useful for resolving the skin discoloration in argyria. [42],[47],[50],[54]
Indian perspective
All the four cases of argyria, described in this article are due to intake of silver coated betel nut/cardamoms [Table - 1]. An extensive literature search conducted with the purpose to identify the reports of argyria pertaining to related forms of exposure yielded five citations. [55],[58],[59],[60],[61] Interestingly, of these, four are from Japan and one from Taiwan. In four of the citations the cause of argyria is ingestion of mouth freshener "Jintan," [55],[58],[59],[60] while in one, argyria is attributed to consumption of silver coated sugar particles. [61] This appears to be a unique cause of argyria due to cultural practice confined to the Asia.
The thin silver leaves called as "Warq" are quite commonly used to coat sweets, cardamoms and betel nut and mouth fresheners. Ash of silver is also widely used in Ayurveda one of the Indian traditional systems of medicine. [75] Silver containing topical medicines are freely available as OTC drugs in India. To the best of our knowledge, this pattern of argyria has not been previously documented from India. Knowing how habit forming is the practice of chewing silver coated mouth fresheners and how widely it is prevalent in India, it comes as a surprise that there are not many more reported cases of argyria. We are tempted to speculate that argyria is under diagnosed because of lack of awareness and because of its insidious onset resulting in a "darkened skin" that is probably tolerated as a natural age or sun exposure related deterioration of the skin.
Conclusion
Argyria, particularly the generalized type, is worth remembering in the differential diagnosis of cutaneous pigmentation. The clinical picture and the natural course of the disease are sufficiently distinctive. The diagnosis is easily clinched by eliciting history of silver ingestion by asking leading questions (may require Sherlockian approach!) and by demonstrating silver deposition in the skin through appropriate histopathological evaluation. Failure to recognize argyria may result in prolonged psycho-social morbidity and unnecessary investigations and treatments.
| 1. |
Lansdown AB. A pharmacological and toxicological profile of silver as an antimicrobial agent in medical devices. Adv Pharmacol Sci 2010;2010:910686.
[Google Scholar]
|
| 2. |
Drake PL, Hazelwood KJ. Exposure-related health effects of silver and silver compounds: A review. Ann Occup Hyg 2005;49:575-85.
[Google Scholar]
|
| 3. |
Fung MC, Bowen DL. Silver products for medical indications: Risk-benefit assessment. J Toxicol Clin Toxicol 1996;34:119-26.
[Google Scholar]
|
| 4. |
Liu J, Wang Z, Liu FD, Kane AB, Hurt RH. Chemical transformations of nanosilver in biological environments. ACS Nano 2012;6:9887-99.
[Google Scholar]
|
| 5. |
Wadhera A, Fung M. Systemic argyria associated with ingestion of colloidal silver. Dermatol Online J 2005;11:12.
[Google Scholar]
|
| 6. |
Brandt D, Park B, Hoang M, Jacobe HT. Argyria secondary to ingestion of homemade silver solution. J Am Acad Dermatol 2005;53:S105-7.
[Google Scholar]
|
| 7. |
Naqvi AH, Shields JW, Abraham JL. Nasal argyria (deposition of silver-selenium) in the photographic film industry: Histopathology and microanalysis. Am J Otolaryngol 2007;28:430-2.
[Google Scholar]
|
| 8. |
Schreiber J, Schreiber C, Hege S, Knolle J. Localized argyria of the proximal trachea. J Bronchology 2005;12:234-5.
[Google Scholar]
|
| 9. |
Gordon DH, Singla SK, Goode R, Pollack HM, Glanz S. Argyrosis of the urinary tract. AJR Am J Roentgenol 1981;136:423-6.
[Google Scholar]
|
| 10. |
Thomas K, Sproston AR, Kingsland CR. A case of vaginal argyrosis: All that glistens isn't gold. BJOG 2001;108:890-1.
[Google Scholar]
|
| 11. |
Griffiths MR, Milne JT, Porter WM. Penile argyria. Br J Dermatol 2006;155:1074-5.
[Google Scholar]
|
| 12. |
Robinson-Bostom L, Pomerantz D, Wilkel C, Mader R, Lerner L, Dufresne R, et al. Localized argyria with pseudo-ochronosis. J Am Acad Dermatol 2002;46:222-7.
[Google Scholar]
|
| 13. |
Pala G, Fronterré A, Scafa F, Scelsi M, Ceccuzzi R, Gentile E, et al. Ocular argyrosis in a silver craftsman. J Occup Health 2008;50:521-4.
[Google Scholar]
|
| 14. |
Sánchez-Huerta V, De Wit-Carter G, Hernández-Quintela E, Naranjo-Tackman R. Occupational corneal argyrosis in art silver solderers. Cornea 2003;22:604-11.
[Google Scholar]
|
| 15. |
Tajirian AL, Campbell RM, Robinson-Bostom L. Localized argyria after exposure to aerosolized solder. Cutis 2006;78:305-8.
[Google Scholar]
|
| 16. |
Zografos L, Uffer S, Chamot L. Unilateral conjunctival-corneal argyrosis simulating conjunctival melanoma. Arch Ophthalmol 2003;121:1483-7.
[Google Scholar]
|
| 17. |
Cho EA, Lee WS, Kim KM, Kim SY. Occupational generalized argyria after exposure to aerosolized silver. J Dermatol 2008;35:759-60.
[Google Scholar]
|
| 18. |
Palamar M, Midilli R, Egrilmez S, Akalin T, Yagci A. Black tears (melanodacryorrhea) from argyrosis. Arch Ophthalmol 2010;128:503-5.
[Google Scholar]
|
| 19. |
Kapur N, Landon G, Yu RC. Localized argyria in an antique restorer. Br J Dermatol 2001;144:191-2.
[Google Scholar]
|
| 20. |
Rumayor Piña A, Martínez Martínez M, Toral Rizo VH, Ajudarte Lopes M, Paes de Almeida O. Cutaneous amalgam tattoo in a dental professional: An unreported occupational argyria. Br J Dermatol 2012;167:1184-5.
[Google Scholar]
|
| 21. |
Lansdown AB. Silver in health care: Antimicrobial effects and safety in use. Curr Probl Dermatol 2006;33:17-34.
[Google Scholar]
|
| 22. |
Fisher NM, Marsh E, Lazova R. Scar-localized argyria secondary to silver sulfadiazine cream. J Am Acad Dermatol 2003;49:730-2.
[Google Scholar]
|
| 23. |
Wang XQ, Chang HE, Francis R, Olszowy H, Liu PY, Kempf M, et al. Silver deposits in cutaneous burn scar tissue is a common phenomenon following application of a silver dressing. J Cutan Pathol 2009;36:788-92.
[Google Scholar]
|
| 24. |
Schwieger-Briel A, Kiritsi D, Schumann H, Meiss F, Technau K, Bruckner-Tuderman L. Grey spots in a patient with dystrophic epidermolysis bullosa. Br J Dermatol 2010;163:1124-6.
[Google Scholar]
|
| 25. |
Holck DE, Klintworth GK, Dutton JJ, Foulks GN, Manning FJ. Localized conjunctival argyrosis: A late sequela of strabismus surgery. Ophthalmic Surg Lasers 2000;31:495-8.
[Google Scholar]
|
| 26. |
Frei J, Schröder B, Messerli J, Probst A, Meyer P. Localized argyrosis 58 years after strabismus operation - An ophthalmological rarity. Klin Monbl Augenheilkd 2001;218:61-3.
[Google Scholar]
|
| 27. |
Ellison DW, Chant AD, Harrison TA, Theaker JM. Localized argyria: A complication of the repair of inguinal hernia with silver filigree. Br J Surg 1993;80:1325.
[Google Scholar]
|
| 28. |
Trop M, Novak M, Rodl S, Hellbom B, Kroell W, Goessler W. Silver-coated dressing acticoat caused raised liver enzymes and argyria-like symptoms in burn patient. J Trauma 2006;60:648-52.
[Google Scholar]
|
| 29. |
Flohr C, Heague J, Leach I, English J. Topical silver sulfadiazine-induced systemic argyria in a patient with severe generalized dystrophic epidermolysis bullosa. Br J Dermatol 2008;159:740-1.
[Google Scholar]
|
| 30. |
Browning JC, Levy ML. Argyria attributed to silvadene application in a patient with dystrophic epidermolysis bullosa. Dermatol Online J 2008;14:9.
[Google Scholar]
|
| 31. |
Anderson EL, Janofsky J, Jayaram G. Argyria as a result of somatic delusions. Am J Psychiatry 2008;165:649-50.
[Google Scholar]
|
| 32. |
Chang AL, Khosravi V, Egbert B. A case of argyria after colloidal silver ingestion. J Cutan Pathol 2006;33:809-11.
[Google Scholar]
|
| 33. |
Chung IS, Lee MY, Shin DH, Jung HR. Three systemic argyria cases after ingestion of colloidal silver solution. Int J Dermatol 2010;49:1175-7.
[Google Scholar]
|
| 34. |
Gulbranson SH, Hud JA, Hansen RC. Argyria following the use of dietary supplements containing colloidal silver protein. Cutis 2000;66:373-4.
[Google Scholar]
|
| 35. |
White JM, Powell AM, Brady K, Russell-Jones R. Severe generalized argyria secondary to ingestion of colloidal silver protein. Clin Exp Dermatol 2003;28:254-6.
[Google Scholar]
|
| 36. |
Tomi NS, Kränke B, Aberer W. A silver man. Lancet 2004;363:532.
[Google Scholar]
|
| 37. |
Wickless SC, Shwayder TA. Medical mystery - The answer. N Engl J Med 2004;351:2349-50.
[Google Scholar]
|
| 38. |
Van de Voorde K, Nijsten T, Schelfhout K, Moorkens G, Lambert J. Long-term use of silver containing nose-drops resulting in systemic argyria. Acta Clin Belg 2005;60:33-5.
[Google Scholar]
|
| 39. |
Sakai N, Aoki M, Miyazawa S, Akita M, Takezaki S, Kawana S. A case of generalized argyria caused by the use of silver protein as a disinfection medicine. Acta Derm Venereol 2007;87:186-7.
[Google Scholar]
|
| 40. |
Baker CD, Federico MJ, Accurso FJ. Case report: Skin discoloration following administration of colloidal silver in cystic fibrosis. Curr Opin Pediatr 2007;19:733-5.
[Google Scholar]
|
| 41. |
Baernstein A, Smith KM, Elmore JG. Singing the blues: Is it really cyanosis? Respir Care 2008;53:1081-4.
[Google Scholar]
|
| 42. |
Rhee DY, Chang SE, Lee MW, Choi JH, Moon KC, Koh JK. Treatment of argyria after colloidal silver ingestion using Q-switched 1,064-nm Nd: YAG laser. Dermatol Surg 2008;34:1427-30.
[Google Scholar]
|
| 43. |
Tóth V, Marschalkó M, Hársing J, Kárpáti S. Grayish discoloration of the face - Argyria. Orv Hetil 2009;150:1503-7.
[Google Scholar]
|
| 44. |
Kim Y, Suh HS, Cha HJ, Kim SH, Jeong KS, Kim DH. A case of generalized argyria after ingestion of colloidal silver solution. Am J Ind Med 2009;52:246-50.
[Google Scholar]
|
| 45. |
Kwon HB, Lee JH, Lee SH, Lee AY, Choi JS, Ahn YS. A case of argyria following colloidal silver ingestion. Ann Dermatol 2009;21:308-10.
[Google Scholar]
|
| 46. |
Bowden LP, Royer MC, Hallman JR, Lewin-Smith M, Lupton GP. Rapid onset of argyria induced by a silver-containing dietary supplement. J Cutan Pathol 2011;38:832-5.
[Google Scholar]
|
| 47. |
Han TY, Chang HS, Lee HK, Son SJ. Successful treatment of argyria using a low-fluence Q-switched 1064-nm Nd: YAG laser. Int J Dermatol 2011;50:751-3.
[Google Scholar]
|
| 48. |
Merchant F, Carpenter T. Blue-gray discoloration of the skin. Am Fam Physician 2011;84:821-2.
[Google Scholar]
|
| 49. |
Stafeeva K, Erlanger M, Velez-Montoya R, Olson JL. Ocular argyrosis secondary to long-term ingestion of silver nitrate salts. Clin Ophthalmol 2012;6:2033-6.
[Google Scholar]
|
| 50. |
Saager RB, Hassan KM, Kondru C, Durkin AJ, Kelly KM. Quantitative near infrared spectroscopic analysis of Q-Switched Nd: YAG treatment of generalized argyria. Lasers Surg Med 2013;45:15-21.
[Google Scholar]
|
| 51. |
Thompson R, Elliott V, Mondry A. Argyria: Permanent skin discoloration following protracted colloid silver ingestion. BMJ Case Rep 2009;2009.
[Google Scholar]
|
| 52. |
Schrauben SJ, Bhanusali DG, Sheets S, Sinha AA. A case of argyria: Multiple forms of silver ingestion in a patient with comorbid schizoaffective disorder. Cutis 2012;89:221-4.
[Google Scholar]
|
| 53. |
Bianchi L, Orlandi A, Di Stefani A, Ricci R, Chimenti S. "Familial" generalized argyria. Arch Dermatol 2006;142:789-90.
[Google Scholar]
|
| 54. |
Hovenic W, Golda N. Treatment of argyria using the quality-switched 1,064-nm neodymium-doped yttrium aluminum garnet laser: Efficacy and persistence of results at 1-year follow-up. Dermatol Surg 2012;38:2031-4.
[Google Scholar]
|
| 55. |
Sato S, Sueki H, Nishijima A. Two unusual cases of argyria: The application of an improved tissue processing method for X-ray microanalysis of selenium and sulphur in silver-laden granules. Br J Dermatol 1999;140:158-63.
[Google Scholar]
|
| 56. |
Rackoff EM, Benbenisty KM, Maize JC, Maize JC Jr. Localized cutaneous argyria from an acupuncture needle clinically concerning for metastatic melanoma. Cutis 2007;80:423-6.
[Google Scholar]
|
| 57. |
Alés-Fernández M, Ríos-Martín JJ, Camacho-Martínez FM. Localized argyria secondary to acupuncture mimicking blue nevus. J Drugs Dermatol 2010;9:1019-20.
[Google Scholar]
|
| 58. |
Ohbo Y, Fukuzako H, Takeuchi K, Takigawa M. Argyria and convulsive seizures caused by ingestion of silver in a patient with schizophrenia. Psychiatry Clin Neurosci 1996;50:89-90.
[Google Scholar]
|
| 59. |
Shimamoto Y, Shimamoto H. Systemic argyria secondary to breath freshener "Jintan Silver Pills". Hiroshima J Med Sci 1987;36:245-7.
[Google Scholar]
|
| 60. |
Yang CY, Chen YJ, Shen JL. Generalized argyria-A case report. Dermatol Sin 2008;26:75-9.
[Google Scholar]
|
| 61. |
Hanada K, Hashimoto I, Kon A, Kida K, Mita R. Silver in sugar particles and systemic argyria. Lancet 1998;351:960.
[Google Scholar]
|
| 62. |
Morton CA, Fallowfield M, Kemmett D. Localized argyria caused by silver earrings. Br J Dermatol 1996;135:484-5.
[Google Scholar]
|
| 63. |
Sugden P, Azad S, Erdmann M. Argyria caused by an earring. Br J Plast Surg 2001;54:252-3.
[Google Scholar]
|
| 64. |
Weiler HH, Lemp MA, Zeavin BH, Suarez AF. Argyria of the cornea due to self-administration of eyelash dye. Ann Ophthalmol 1982;14:822-3.
[Google Scholar]
|
| 65. |
Plack W, Bellizzi R. Generalized argyria secondary to chewing photographic film. Report of a case. Oral Surg Oral Med Oral Pathol 1980;49:504-6.
[Google Scholar]
|
| 66. |
Schlötzer-Schrehardt U, Holbach LM, Hofmann-Rummelt C, Naumann GO. Multifocal corneal argyrosis after an explosion injury. Cornea 2001;20:553-7.
[Google Scholar]
|
| 67. |
Hristov AC, High WA, Golitz LE. Localized cutaneous argyria. J Am Acad Dermatol 2011;65:660-1.
[Google Scholar]
|
| 68. |
Espinal ML, Ferrando L, Jimenez Díaz F. Asymptomatic blue nevus-like macule. Diagnosis: Localized argyria. Arch Dermatol 1996;132:461, 464.
[Google Scholar]
|
| 69. |
Sue YM, Lee JY, Wang MC, Lin TK, Sung JM, Huang JJ. Generalized argyria in two chronic hemodialysis patients. Am J Kidney Dis 2001;37:1048-51.
[Google Scholar]
|
| 70. |
Ali A, Wiener K, Sridharan V. Minerva. Br Med J 2009;339:B2919.
[Google Scholar]
|
| 71. |
Utikal J, Thoelke A, Becker JC, Figl R, Goerdt S, Schadendorf D, et al. Local cutaneous argyria mimicking melanoma metastases in a patient with disseminated melanoma. J Am Acad Dermatol 2006;55:S92-4.
[Google Scholar]
|
| 72. |
Granstein RD, Sober AJ. Drug- and heavy metal - Induced hyperpigmentation. J Am Acad Dermatol 1981;5:1-18.
[Google Scholar]
|
| 73. |
Jonas L, Bloch C, Zimmermann R, Stadie V, Gross GE, Schäd SG. Detection of silver sulfide deposits in the skin of patients with argyria after long-term use of silver-containing drugs. Ultrastruct Pathol 2007;31:379-84.
[Google Scholar]
|
| 74. |
al-Talib RK, Wright DH, Theaker JM. Orange-red birefringence of gold particles in paraffin wax embedded sections: An aid to the diagnosis of chrysiasis. Histopathology 1994;24:176-8.
[Google Scholar]
|
| 75. |
Nadeem A, Khanna T, Vohra SB. Silver preperations used in Indian systems of medicine: Neuropsychobehavioural effects. Indian J Pharmacol 1999;31:214-21.
[Google Scholar]
|
Fulltext Views
8,371
PDF downloads
3,197





