Translate this page into:
Asymptomatic brownish hyperkeratotic scaly plaque on the thigh
Corresponding author: Dr. Ossama Abbas, Department of Dermatology, American University of Beirut Medical Center, P.O. Box 11-0236, Riad El Solh, Beirut 1107 2020, Lebanon. ossamaabbas2003@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Al-Hage J, Hanna E, Kurban M, Abbas O. Asymptomatic brownish hyperkeratotic scaly plaque on the thigh. Indian J Dermatol Venereol Leprol 2022;88:74-5.
The Case
A 21-year-old man presented with an asymptomatic skin lesion over the ventro-lateral aspect of his left thigh since last 5 days. He also suffers from Down’s syndrome and was initiated on chemotherapy for acute lymphoblastic leukemia 2 weeks prior to his presentation. The chemotherapeutic regimen consisted of vincristine, daunorubicin, and L-asparaginase.
Skin examination revealed a brownish hyperkeratotic scaly plaque approximately 8 × 5 cm in size, surrounded by an erythematous to purpuric halo [Figure 1]. Skin biopsy and histopathology demonstrated epidermal hyperkeratosis, compact parakeratosis and retention of basophilic keratohyalin granules within the stratum corneum along with mild superficial perivascular dermal lymphocytic infiltrate [Figure 2].
What Is Your Diagnosis?
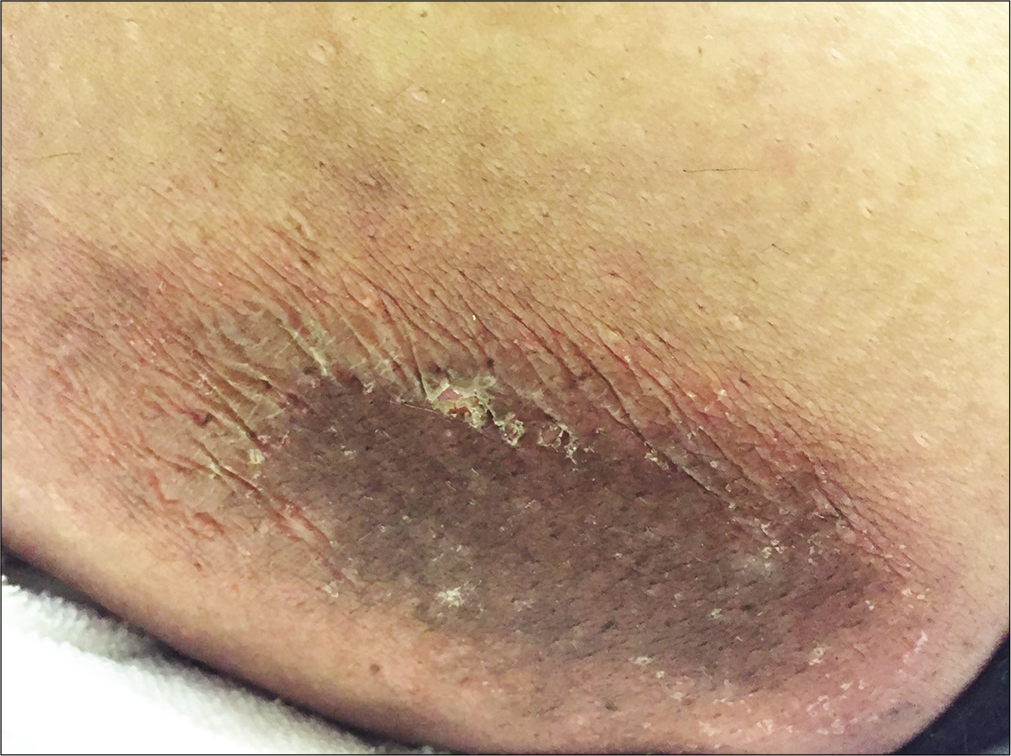
- Brownish hyperkeratotic scaly plaque, surrounded by an erythematous to purpuric halo on the left thigh
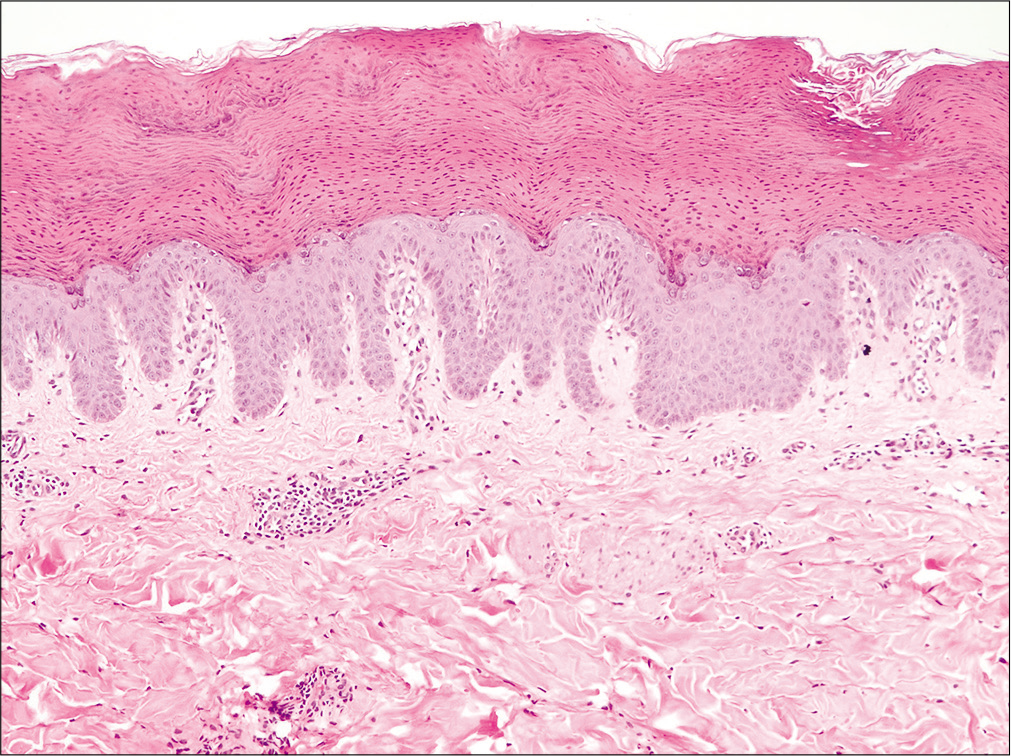
- Thick stratum corneum with retention of nuclei and basophilic keratohyalin granules (H and E, ×100)
Diagnosis
Granular parakeratosis.
Discussion
First described in 1991, granular parakeratosis is an uncommon, benign dermatologic condition,1,2 representing a unique type of parakeratosis characterized by retention of both nuclei and keratohyalin granules within the stratum corneal keratinocytes. It results from altered keratinocyte maturation from the stratum granulosum to stratum corneum. Intertriginous regions are commonly affected like axillae and groins.1
Clinically, granular parakeratosis classically manifests as erythematous to brownish papules which may coalesce into large hyperkeratotic plaques. Though intertriginous sites are commonly affected, non-intertriginous areas like flanks, cheeks, and scalp, similar to our patient, may be rarely involved.1-5 Notably, only two cases of granular parakeratosis have been reported in the setting of chemotherapy, both on intertriginous sites.3,4 In one case, lesions developed in association with doxorubicin, a chemotherapeutic agent belonging to the same family as daunorubicin, which our patient was receiving. In our case, the temporal association with chemotherapy highly supports a possible etiologic role of these cytotoxic drugs.
The exact pathogenesis of this condition remains unknown. Several possible risk factors have been implicated like occlusion, friction, moist environment and the application of certain antiperspirants and zinc oxide, which interrupt the breakdown of profilaggrin to filaggrin during epidermal differentiation.2 Additionally, it may also occur as an incidental histological reaction pattern with unrelated conditions and may not be restricted to the flexures.1 In our case, no local triggering factor could be identified, though friction remains a possibility. We propose that certain chemotherapeutic drugs like anthracycline antibiotics could be possible inducers of granular parakeratosis through their direct effect on keratinocyte maturation, especially in predisposed individuals. This may be considered analogous to other dyskeratotic/keratinocyte dysmaturation entities reported following chemotherapy like syringosquamous metaplasia.6 We also report the first case of granular parakeratosis in the setting of Down’s syndrome.
Differential diagnoses include contact dermatitis, acanthosis nigricans, confluent and reticulated papillomatosis, seborrheic keratoses, acantholytic dyskeratosis, Hailey–Hailey disease, Darier’s disease, pemphigus vegetans, and fungal infection which may mimick it clinically or affect similar sites.1 Characteristic histopathological features help to rule out these differentials and establish the correct disgnosis.
Currently, convincing therapeutic options are lacking for this condition. Multiple therapeutic agents have been tried with varying rates of success like topical corticosteroids, tretinoin, antifungals, antimicrobials, vitamin D analogs and pimecrolimus as well as systemic isotretinoin, antibiotics, antifungals and corticosteroids. Destructive modalities including cryotherapy and lasers have also been attempted. In case of possible drug-induced granular parakeratosis, discontinuation of culprit medication may result in its resolution. Spontaneous remission has been reported frequently. Our patient reported complete resolution of the lesion with 6 weeks of topical tretinoin. No recurrence was observed during the next 16 weeks.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Granular parakeratosis: A comprehensive review and a critical reappraisal. Am J Clin Dermatol. 2015;16:495-500.
- [CrossRef] [PubMed] [Google Scholar]
- Granular parakeratosis: A case report and literature review. J Cutan Pathol. 2003;30:332-5.
- [CrossRef] [PubMed] [Google Scholar]
- Granular parakeratosis in a patient treated with liposomal doxorubicin for ovarian carcinoma. J Am Acad Dermatol. 2008;58:S84-7.
- [CrossRef] [PubMed] [Google Scholar]
- Granular parakeratosis presenting with facial keratotic papules. Indian J Dermatol Venereol Leprol. 2008;74:53-5.
- [CrossRef] [PubMed] [Google Scholar]
- Syringometaplasia: Variants and underlying mechanisms. Int J Dermatol. 2016;55:142-8.
- [CrossRef] [PubMed] [Google Scholar]





