Translate this page into:
Asymptomatic erythematous plaques on the left arm and trunk
Correspondence Address:
Hyun Jeong Park
Department of Dermatology, YeouidoSt. Mary's Hospital, College of Medicine, The Catholic University of Korea, 62 Yeouido-dong, Youngdeunpo-gu, Seoul, 315-713
Korea
| How to cite this article: Lim J, Woo Y, Kim M, Park HJ. Asymptomatic erythematous plaques on the left arm and trunk. Indian J Dermatol Venereol Leprol 2019;85:76-80 |
A 23-year-old man presented to our department with a 3-year history of asymptomatic, erythematous plaques and patches on the left arm and trunk. The skin lesions gradually increased in size over the past 2 years. There was no relevant medical history. Clinical examination revealed a 3 × 2 cm annular erythematous plaque on the left arm [Figure - 1] and thin erythematous patches of varying sizes on the trunk [Figure - 2]. There was no lymphadenopathy. Histopathological findings are shown in [Figure - 3] and [Figure - 4].
 |
| Figure 1: A 3 cm×2 cm annular erythematous plaque on the left arm |
 |
| Figure 2: Variable-sized erythematous patches on the trunk |
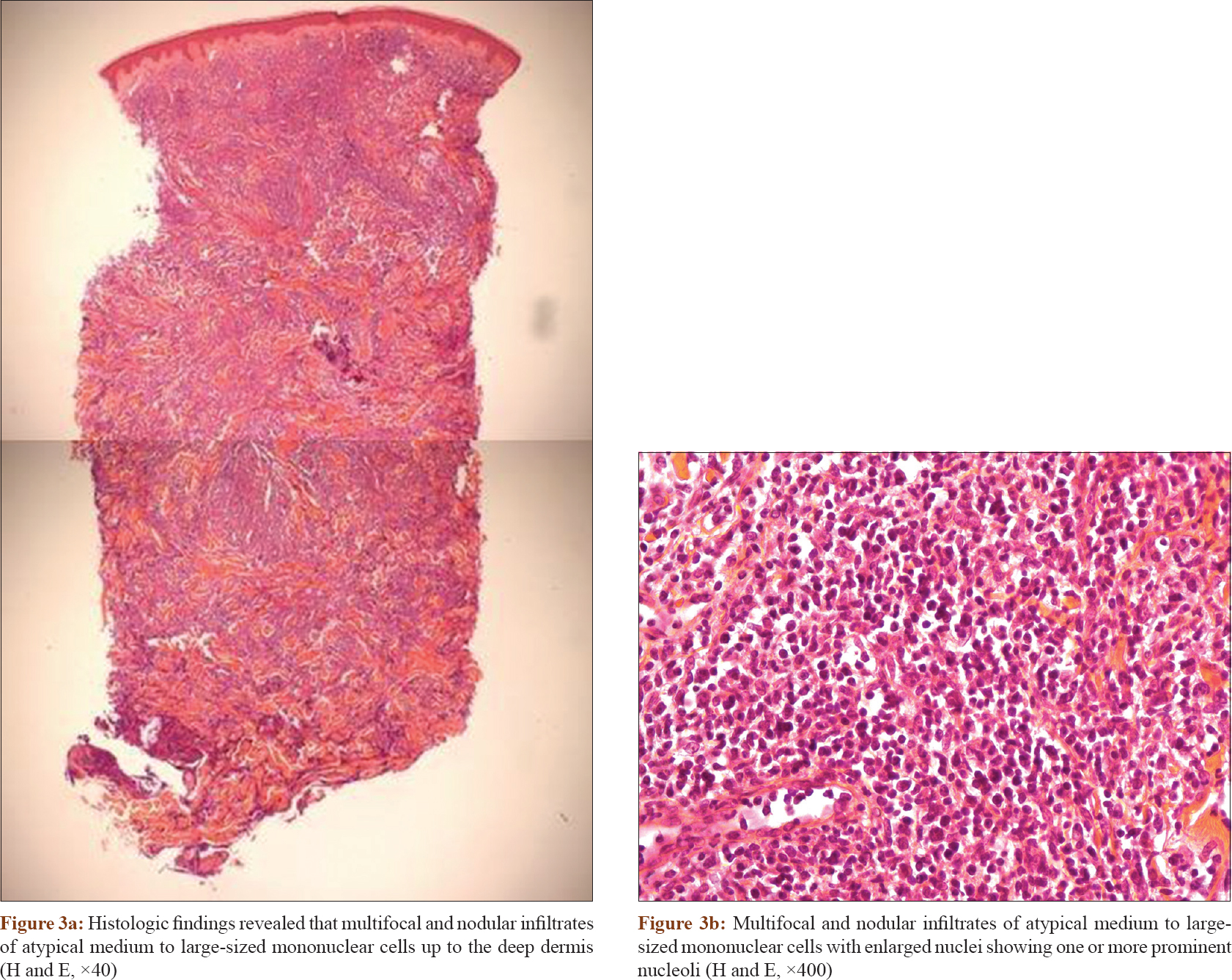 |
| Figure 3 |
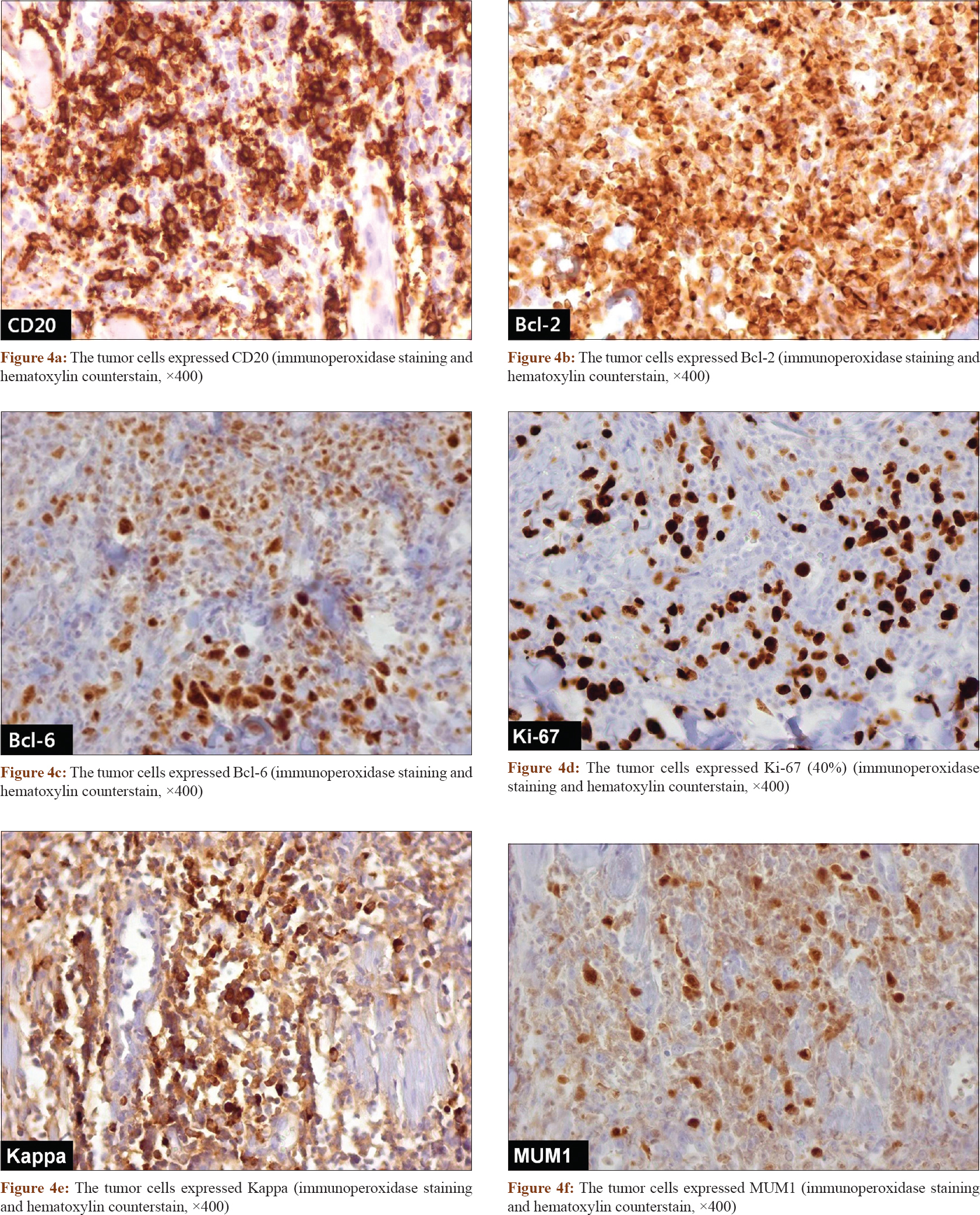 |
| Figure 4 |
Question
What is your diagnosis?
Answer
Diagnosis: Primary cutaneous diffuse large B-cell lymphoma, leg type
Histological examination of the lesions revealed multifocal and nodular infiltrates of atypical medium to large sized mononuclear cells with enlarged nuclei showing one or more prominent nucleoli [Figure - 3]a and [Figure - 3]b. Immunohistochemical examination revealed that the tumor cells were positive for CD20, Bcl-2, Bcl-6, ki-67 (40%), kappa and multiple myeloma oncogene 1 (MUM 1) but negative for CD3, CD10, lambda, Epstein–Barr virus (EBV), CD21, CD23and CD30 [Figure - 4]a,[Figure - 4]b,[Figure - 4]c,[Figure - 4]d,[Figure - 4]e,[Figure - 4]f. Complete staging investigations including peripheral blood, computed tomography scans of the thorax and abdomen, and positron emission tomography-computed tomography (PET-CT) whole body imaging studies did not detect metastatic or disseminated disease. A bone marrow examination showed it to be uninvolved. Based on these results, the patient was diagnosed with primary cutaneous diffuse large B-cell lymphoma, leg type, which was stage II according to World Health Organization–European Organization for Research and Treatment of Cancer classification. Six cycles of chemotherapy with combination of rituximab, cyclophosphamide, adriamycin, vincristine and prednisone were administered from the hematooncology department every 21 days. After six cycles of chemotherapy, the patient achieved complete remission. Followup PET-CT whole body imaging studies did not detect any metastatic or disseminated disease. Furthermore, after 5-months follow-up biopsy of the lesions was negative for malignancy. He was asymptomatic during the follow-up after 6 months.
Discussion
Primary cutaneous B cell lymphomas are defined as B-cell phenotype tumors that are confined to the skin, with no evidence of extracutaneous involvement at the time of initial diagnosis.[1] Primary cutaneous B cell lymphomas are categorized into primary cutaneous marginal zone B-cell lymphoma, primary cutaneous follicle center lymphoma, primary cutaneous diffuse large B-cell lymphoma, leg type and primary cutaneous diffuse large B-cell lymphoma, other, according to the World Health Organization- European Organisation for Research and Treatment of Cancer classification.[1] Primary cutaneous diffuse large B-cell lymphoma, leg type clinically presents as a rapidly growing red or bluish-red tumor located on the lower legs, with most occurring in elderly persons with a median age of 76 years, primarily in females.[1],[2]
Although primary cutaneous diffuse large B-cell lymphoma, leg type is a rare subtype comprising only 4% of all cutaneous lymphomas,[1] some clinicians reported that diffuse large B-cell lymphoma was more prevalent in Korea than in Western countries and primary cutaneous diffuse large B-cell lymphoma, leg type was the more common type of primary cutaneous B cell lymphoma in Korea.[3] Primary cutaneous diffuse large B-cell lymphoma, leg type exhibits more aggressive behavior than other groups of primary cutaneous B cell lymphomas with a poor prognosis. Estimated 5-year specific survival rates are approximately 50%.[2]
The differential diagnoses to consider include primary cutaneous follicle center lymphoma and primary cutaneous marginal zone B-cell lymphoma. Primary cutaneous follicle center lymphoma characteristically shows a proliferation of large centrocytes, which generally do not express Bcl-2 or Mum-1 and most patients showed localized cutaneous lesions on the head or trunk. Primary cutaneous marginal zone B-cell lymphoma can be distinguished from primary cutaneous diffuse large B-cell lymphoma, leg type through composition of small cells with irregular nuclei.[1]
Follicular lymphoma is the most common indolent nonHodgkin lymphoma with a median age at presentation ranging from 60 to 70 years and is rare in patients younger than 40 years.[4] The prognosis of follicular lymphoma in young adults may be more favorable than that in elderly, despite presenting with a similar extent of disease.[4] However, the true prognosis of primary cutaneous diffuse large B-cell lymphoma, leg type in young patients remains unclear and further study is needed to understand the basis of its clinicopathological characteristics.
This is an interesting and rare case of primary cutaneous diffuse large B-cell lymphoma, leg type in a young adult who presented with lesions at sites other than leg. Till now, only one case of primary cutaneous diffuse large B-cell lymphoma, leg type in adults less than 30 years of age has been reported.[5] Therefore, cutaneous lymphoma in young adults should be differentiated from benign skin disorders, which can have a similar presentation. Suspicious lesions should be biopsied for early diagnosis and treatment.
Acknowledgement
This research was supported by the Basic Science Research program and Creative Materials Discovery Program through the National Research Foundation of Korea (NRF), which is funded by the Ministry of Education, Science and Technology and the Ministry of Science, ICT and Future Planning (2015R1C1A2A01055073, 2016M3D1A1021387).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85.
[Google Scholar]
|
| 2. |
Suárez AL, Pulitzer M, Horwitz S, Moskowitz A, Querfeld C, Myskowski PL. Primary cutaneous B-cell lymphomas: Part I. Clinical features, diagnosis, and classification. J Am Acad Dermatol 2013;69:329.e1-13.
[Google Scholar]
|
| 3. |
Lee JH, Lee JH, Yoo DS, Kang H, Kim GM, Park HJ, et al. Characteristics of primary cutaneous lymphoma according to WHO-EORTC classification in Korea. Clin Exp Dermatol 2013;38:457-63.
[Google Scholar]
|
| 4. |
Gangatharan SA, Maganti M, Kuruvilla JG, Kukreti V, Tiedemann RE, Gospodarowicz MK, et al. Clinical characteristics and early treatment outcomes of follicular lymphoma in young adults. Br J Haematol 2015;170:384-90.
[Google Scholar]
|
| 5. |
Mondal SK, Mandal PK, Roy S, Biswas PK. Primary cutaneous large B-cell lymphoma, leg type: Report of two cases and review of literature. Indian J Med Paediatr Oncol 2012;33:54-7.
[Google Scholar]
|
Fulltext Views
6,983
PDF downloads
3,662





