Translate this page into:
Asymptomatic nodule over the shin
Correspondence Address:
Uday Khopkar
Department of Dermatology, Seth GS Medical College and KEM Hospital, Parel, Mumbai - 400 012
India
| How to cite this article: Gutte R, Garg G, Kharkar V, Khopkar U. Asymptomatic nodule over the shin. Indian J Dermatol Venereol Leprol 2012;78:123 |
A 58-year-old male presented with an asymptomatic dome-shaped shiny, slightly scaly indurated nodule over anterior aspect of left leg. Lesion was present since 1 year and gradually increased to the present size. There was no history of trauma, oozing, crusting, or similar lesions elsewhere or family history of similar lesions. The examination revealed single erythematous, indurated, scaly, nontender sessile nodule measuring 1.5 ΄ 2 cm in size [Figure - 1]. Rest of the cutaneous and systemic examination and blood biochemistry were within normal limits. Serum electrophoresis, thyroid function tests, and venous doppler of bilateral lower limbs showed no abnormality. Antinuclear antibodies and human immunodeficiency virus antibodies were negative.
 |
| Figure 1: Solitary dome-shaped scaly erythematous nodule over anterior aspect of left leg |
Hematoxylin and eosin-stained sections of excision biopsy from such a papule are shown in [Figure - 2], and toluidine blue stain is shown in [Figure - 3].
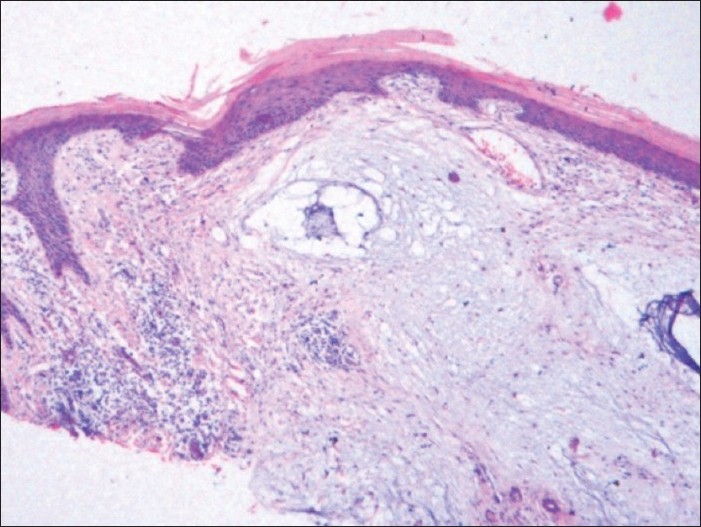 |
| Figure 2: Acanthosis, mild hyperkeratosis, and spares perivascular lymphocytic infiltrate with diffuse dermal mucin deposition (H and E, ×200) |
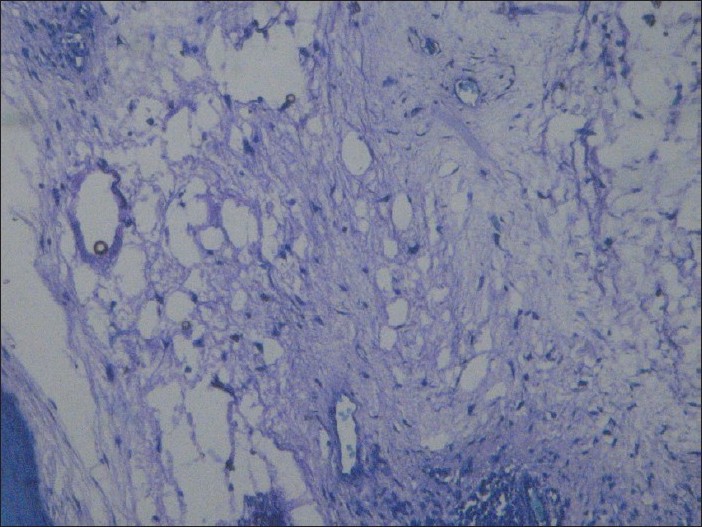 |
| Figure 3: Diffuse dermal mucin stained violet with toluidine blue stain (Toluidine blue, ×200) |
What is your Diagnosis?
Answer: Cutaneous focal mucinosis (CFM)
Histological examination of excised specimen revealed mild hyperkeratosis, thinned epidermis, and diffuse mucin deposition in the dermis with bluish myxoid and stringy, and granular appearance of stroma with increased number of mast cells and without folliculo-tropism or increased vascularity [Figure - 2]. Mild superficial perivascular lymphocytic infiltrate without pigment incontinence was also seen. Toludine blue stain confirmed the presence of diffuse dermal mucin [Figure - 3].
Discussion
Cutaneous mucinosis is a heterogenous disorder characterized by abnormal deposition of mucin within the dermis. It could be primary (e.g., CFM) or secondary (e.g., associated with a neoplasm). [1]
Mucin is an amorphous and gelatinous substance concerned with hydration of ground substance. Although exact source of mucin is not known, fibroblasts are claimed to produce acid mucopolysaccharides that stain with toluidine blue stain. Abnormal deposition of mucin either discrete or diffuse throughout the dermis causes cutaneous mucinosis. [2]
Mucinoses can be primary, i.e., due to metabolic cause or secondary, i.e., due to catabolic cause. [2],[3] Various causes for secondary mucinosis include thyroid dysfunction, connective tissue disease, granuloma annulare, graft-vs-host disease, follicular mucinosis, Dego′s disease, venous insufficiency to post ultraviolet or photochemotherapy treatment, and more recently HIV infection. None of these was present in our patient. [2],[4],[5]
CFM was first described as separate entity by Johnson and Helwig in 1966 who also defined histologic criteria for diagnosis of the same. [3] CFM typically presents usually as an asymptomatic solitary papule or nodule mostly on the face, trunk, or extremities in middle-aged adults affecting both sexes. [1],[3] Multiple lesions are seen with self-healing juvenile and adult form of cutaneous mucinosis and rarely lesions are also described in infants, i.e., cutaneous mucinosis of infancy (CFI). [1],[6]
Exact cause of CFM is obscure but it is thought to be more of reactive than neoplastic lesion, and fibroblasts are claimed to be the major source of hyaluronic acid produced in expense of connective tissue, while tissue hypoxia has been postulated as possible stimulus for mucin secretion by fibroblast in venous insufficiency and hypoxia-induced hyaluronic acid secretion by articular chondrocytes has been documented. [1],[3],[4]
Histopathology is essential for diagnosis of CFM that shows diffuse ill-defined dermal mucinous lesion with normal or hyperplastic hyperkeratotic epidermis and sparing of subcutaneous tissue. Additionally, thinned collagen fibers within mucinous stroma with absent elastic or reticulum fibers without increased vascularity are seen. [1],[3] Follicular induction of epidermis as in dermatofibroma is also seen occasionally in CFM. [1],[7] Mucin in CFM can be stained with Alcian blue at pH 2.5 or with toludine blue stain. [1]
CFM should be differentiated from many conditions such as papular and nodular mucinosis, digital mucus cyst, CFI, self-healing cutaneous mucinosis, nodular cutaneous lupus mucinosis and cutaneous myxoma, ganglion, and alopecia mucinosa. [2],[3],[8],[9]
Excision is the treatment of choice [2]
Differentiation from cutaneous myxoma is important which is a progressively growing neoplasm that is composed of mucinous stroma, network of fine reticulum fibers with spindle-shaped fibroblasts entrapped within lesion and increased vascularity with microhemorrhages and occasional inflammation. Multiple cutaneous lesions with a prominent vascular component are recognized feature of Carney′s complex consisting of dominantly inherited complex of myxomas (cutaneous, cardiac, and mammary) with spotty pigmentation and endocrine overactivity. [1],[3]
| 1. |
Wilk M, Schmoeckel C. Cutaneous focal mucinosis - A histopathological and immunohistochemical analysis of 11 cases. J Cutan Pathol 1994;21:446-52.
[Google Scholar]
|
| 2. |
Kumar B, Dogra S. Metabolic disorders. In: Valia RG, Valia AR, editors. IADVL Textbook of Dermatology. 3 rd ed. Mumbai, India: Bhalani Publishing House; 2008. p. 1298-337.
[Google Scholar]
|
| 3. |
Bernier MA, Vila JB, Bordel-Gomez MT, Gracia GM, Garcia-Tejerina JA, Romero AM. Multiple transluscent papules on chest-Quiz case. Arch Dermatol 2004;140:1531-6.
[Google Scholar]
|
| 4. |
Pugashetti R, Zedek DC, Seiverling EV, Rajendarn P, Berger T. Dermal mucinosis as a sign of venous insufficiency. J Cutan Pathol 2010;37:292-6.
[Google Scholar]
|
| 5. |
Rongioletti F, Ghigliotti G, Demarchi R, Rebora A. Cutaneous mucinosis and HIV infection. Br J Dermatol 1998;139:1077-80.
[Google Scholar]
|
| 6. |
Velho GC, Oliveira M, Alves R, Silvestreb F, Massaa A, Baptist AP. Childhood cutaneous mucinosis. J Eur Acad Dermatol Venereol 1998;10:161-6.
[Google Scholar]
|
| 7. |
Tatsas AD, O'Leary MF, Wright JE, Robbins JB. Cutaneous focal mucinosis causing follicular induction of the epidermis. Am J Dermatopathol 2009;31:462-4.
[Google Scholar]
|
| 8. |
Kano Y, Sagawa Y, Yagita A, Nagashima M. Nodular cutaneous lupus mucinosis: Report of a case and review of previously reported cases. Cutis 1996;57:441-4.
[Google Scholar]
|
| 9. |
Usha V, Yogirajan K, Papali C, Remadevi AV. Self-healing juvenile cutaneous mucinosis. Indian J Dermatol Venereol Leprol 1996;62:392-3.
[Google Scholar]
|
Fulltext Views
4,734
PDF downloads
3,424





