Translate this page into:
Atopic dermatitis – Impact on sleep, work performance and its associated costs: A cross-sectional study
Corresponding author: Dr. Adawiyah Jamil, Dermatology Unit, Department of Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia. adawiyahjamil@ukm.edu.my
-
Received: ,
Accepted: ,
How to cite this article: Lim JA, Jamil A, Arumugam M, Kueh YC. Atopic dermatitis – Impact on sleep, work performance and its associated costs: A cross-sectional study. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_892_2024
Dear Editor,
The impact of atopic dermatitis (AD) on sleep disturbance, work performance, and its economic burden has not been adequately described. We conducted this study to uncover the relationships between sleep quality, work performance, predictive factors, and the cost of work performance loss across AD severity.
All patients with AD who visited our centre from March to August 2023 were screened in this cross-sectional study. Participants included were employed and English-proficient adults. Exclusion criteria were non-AD sleep disorder, memory disorder, and medications that affect sleep like antidepressive agents and antipsychotics. Validated Pittsburgh Sleep Quality Index (PSQI) and World Health Organisation Health and Work Performance Questionnaire (WHO-HPQ) were used.1,2 AD severity was assessed using the Eczema Area and Severity Index (EASI). A score of 7 or less indicates mild AD, while a score greater than 21 indicates severe AD.
Out of a total of 402 patients, 78 that fulfilled the study criteria were recruited. The mean age was 31.7 ± 9.2 years with 73.1% being females . Early onset and higher caffeine intake were significantly associated with increasing AD severity. Sleep quality was poor even in mild AD (Global PSQI score 6.65 ± 3.85, 12.32 ± 5.96, 16.63 ± 3.44 for mild, moderate, and severe AD, respectively) [Table 1]. All seven components of sleep (quality, latency, duration, efficiency, disturbance score, daytime dysfunction), absenteeism, and presenteeism were significantly affected across AD severity (p < 0.001) [Figure 1]. Apart from the itch, skin pain and feeling too hot or too cold were among the main causes of sleep disturbance.
| AD severity Mean ± SD or n (%) | P-valuea | |||
|---|---|---|---|---|
| Mild n = 26 | Moderate n = 28 | Severe n = 24 | ||
| Global PSQI sleep score | 6.65 ± 3.85 | 12.32 ± 5.96 | 16.63 ± 3.44 | < 0.001 |
| Caffeine intake, mg/week | 43.8 ± 70.0 | 70.3 ± 61.3 | 116.7 ± 71.7 | 0.001 |
| Age AD diagnosed | 16.4 ± 12.0 | 14.4 ± 14.7 | 7.8 ± 9.8 | 0.045 |
| Absenteeism | ||||
| Absolute absenteeism, hours/month | 1.92 ± 9.81 | 11.57 ± 19.35 | 42.86 ± 49.44 | < 0.001 |
| Relative absenteeism | 0.01 ± 0.05 | 0.06 ± 0.11 | 0.25 ± 0.31 | < 0.001 |
| Presenteeism | ||||
| Absolute Presenteeism, % | 87.31 ± 11.16 | 70.00 ±13.61 | 48.75 ± 22.52 | < 0.001 |
| Relative Presenteeism | 1.00 ± 0.09 | 0.86 ± 0.19 | 0.62 ± 0.27 | < 0.001 |
| Overall work impairment, % | 13.19 ± 13.03 | 34.18 ± 15.84 | 60.75 ± 25.07 | < 0.001 |
| Annual cost of work impairment | ||||
| Cost of absenteeism, $ | 123 ± 626 | 2563 ± 6819 | 6712 ± 11731 | < 0.001 |
| Cost of presenteeism, $ | 3344 ± 3242 | 7644 ± 6379 | 11824 ± 9157 | < 0.001 |
| Cost of overall work impairment, $ | 3405 ± 3317 | 9355 ± 9708 | 14303 ± 12529 | < 0.001 |
| Sleep impact on work and cost | ||||
| PSQI score as independent variable | Regression coefficient, b | 95% CI | t-stat | P-valueb |
| Absenteeism | 2.50 | 1.35 ‒ 3.64 | 4.34 | < 0.001 |
| Presenteeism | 2.48 | 3.08 ‒ 1.87 | 8.14 | < 0.001 |
| Overall work impairment | 0.03 | 0.02 ‒ 0.04 | 8.64 | < 0.001 |
| Estimated annual cost of absenteeism, $ | 495.24 | 218.71 ‒ 771.77 | 3.57 | < 0.001 |
| Cost of presenteeism, $/year | 606.19 | 369.79 ‒ 842.59 | 5.11 | < 0.001 |
| Cost of overall work performance, $/year | 810.79 | 482.69 – 1138.90 | 4.92 | < 0.001 |
| Factors associated with poor work performance | ||||
| Univariate logistic regression | ||||
| Independent variables | OR (95% CI) | P-value | ||
| Occupation | 1.334 (1.031 ‒ 1.724) | 0.028 | ||
| Caffeine | 1.019 (1.010 ‒ 1.028) | < 0.001 | ||
| Alcohol | 7.986 (1.186 ‒ 53.772) | 0.033 | ||
| EASI score | 1.166 (1.094 ‒ 1.244) | <0.001 | ||
| Itch score | 1.975 (1.422 ‒ 2.745) | < 0.001 | ||
| Antihistamine used frequency | 4.339 (1.786 ‒ 10.542) | 0.001 | ||
| PSQI global score | 1.473 (1.232 ‒ 1.760) | < 0.001 | ||
| Sleep quality | 4.223 (2.170 ‒ 8.218) | < 0.001 | ||
| Sleep latency | 4.656 (2.215 ‒ 9.784) | < 0.001 | ||
| Sleep duration | 3.201 (1.671 ‒ 6.130) | < 0.001 | ||
| Sleep efficiency | 3.234 (1.953 ‒ 5.356) | < 0.001 | ||
| Sleep disturbance | 11.785 (3.610 ‒ 38.480) | < 0.001 | ||
| Medication to sleep | 4.688 (1.936 ‒ 11.353) | < 0.001 | ||
| Daytime dysfunction | 2.445 (1.426 ‒ 4.192) | 0.001 | ||
|
Multivariable logistic regression (Final model for predictors of poor work performance) |
||||
| Independent variables | AOR (95% CI) | P-value | ||
| EASI score | 1.144 (1.057 ‒ 1.238) | < 0.001 | ||
| Caffeine | 1.018 (1.005 ‒ 1.031) | 0.006 | ||
| Sleep quality | 2.716 (1.061 ‒ 6.950) | 0.037 | ||
Receiver Operator Characteristic (ROC) = 94.6%, Hosmer-Lemeshow test p = 0.685, 84.6% of cases classified correctly
a One-way ANOVA test; b Linear regression analysis
AD: atopic dermatitis; AOR: adjusted odd’s ratio; BMI: body mass index; CI: confidence interval; EASI: eczema area and severity index; OR: crude odd’s ratio;
PSQI: Pittsburgh sleep quality index; SD: standard deviation; $: US Dollar
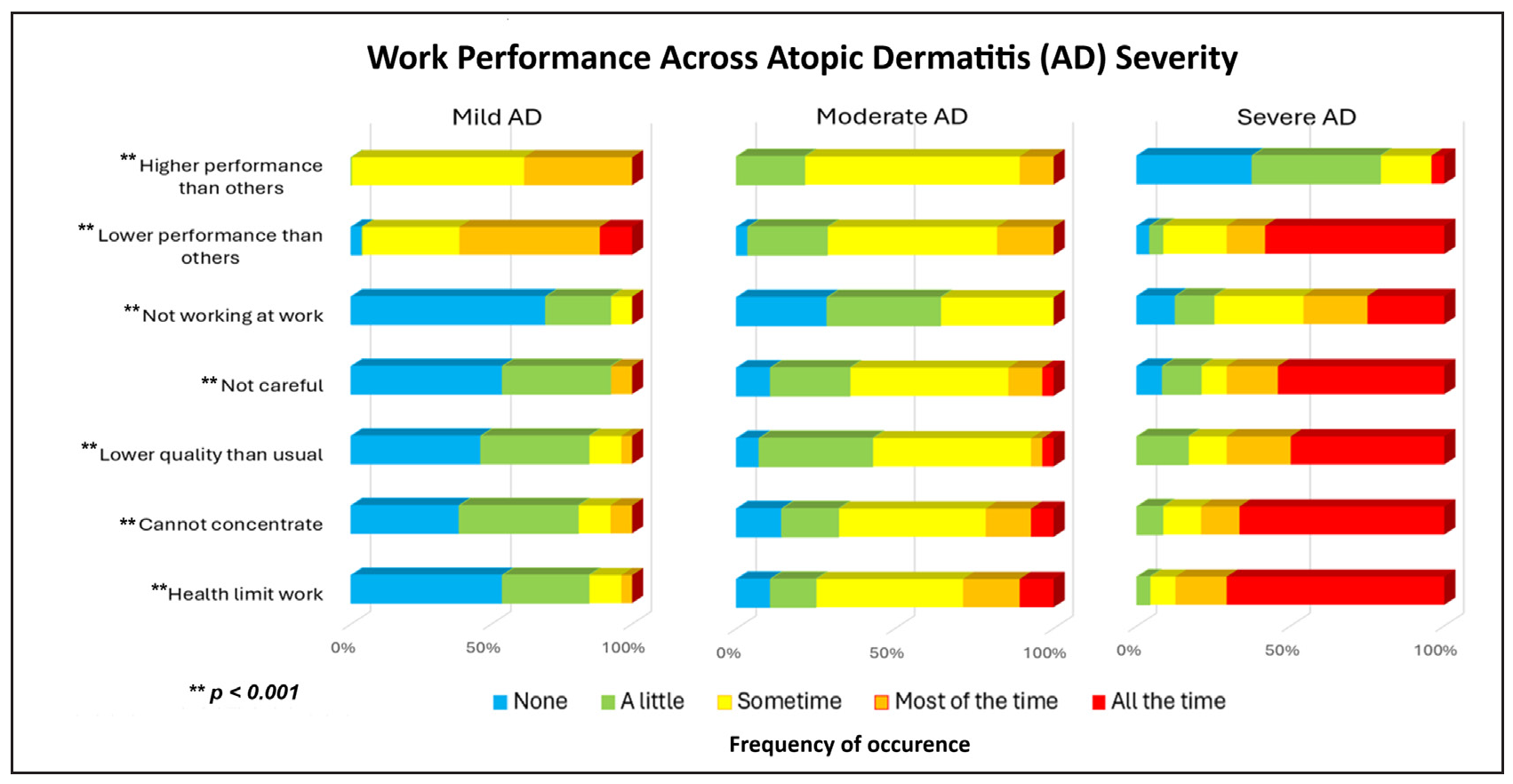
- Components of work performance across atopic dermatitis severity.
Absenteeism and presenteeism were calculated using the WHO-HPQ protocol.3 Absenteeism is the total hours off work, while presenteeism refers to performance at work. Absolute presenteeism measures performance from 0 (no performance) to 100 (full performance) and relative presenteeism is a ratio from 0 to 1. The estimated costs, outlined in the formula in Box 1, were adjusted for purchasing power parity and presented in 2024 U.S. dollars ($).2,4,5
The estimated cost of absenteeism per year was $123 ± 626, $2563 ± 6819, $6712 ± 11,731 for mild, moderate, and severe AD respectively (p < 0.001). The estimated cost of presenteeism per year were $3344 ± 3242, $7644 ± 6379, $11,824 ± 9157 for mild, moderate, and severe AD respectively (p < 0.001). The estimated annual cost of work impairment was $3405 ± 3317 for mild AD, $9355 ± 9708 for moderate AD, and $14,303 ± 12,529 for severe AD (p < 0.001). This corresponded to 11%, 37%, and 59% of the mean annual salary for mild, moderate, and severe AD respectively. This is comparable to developed countries, where the annual indirect cost of AD is approximately $11,807.90 (equivalent to 24.2% of the US annual salary) and ranges from $11,089.39 to $21,694.17 across Europe in the 2024 US dollars.5,6 Additionally, the economic burden of AD is comparable to that of psoriasis.5
Linear regression analyses on the effects of sleep on work and its indirect cost are shown in Table 1. Absenteeism, presenteeism, overall work impairment, and its associated cost were significantly affected by the severity of sleep disturbance across AD severity [Figure 2a-c]. One unit increase in sleep impairment (PSQI) score increased absenteeism by 2.50 times while worsening presenteeism by 2.48 times. Moreover, one unit increase in PSQI score corresponded to an estimated increase in absenteeism cost by $495.24, presenteeism cost by $606.19, and overall work impairment cost by $810.79 respectively (p < 0.001).
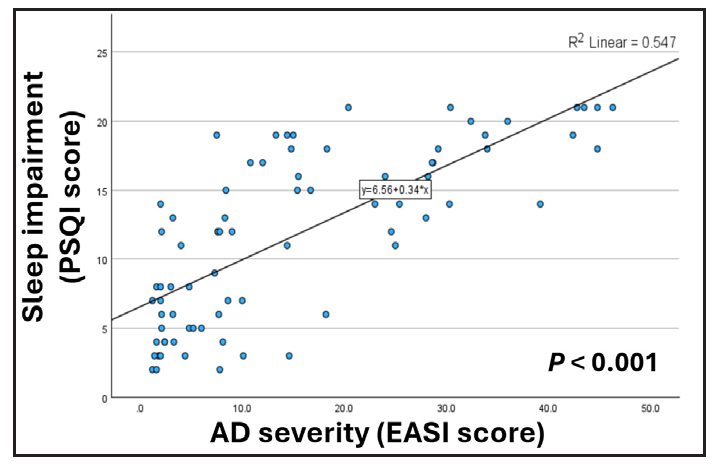
- The effects of atopic dermatitis (AD) severity based on eczema area and severity index (EASI) score, on sleep.
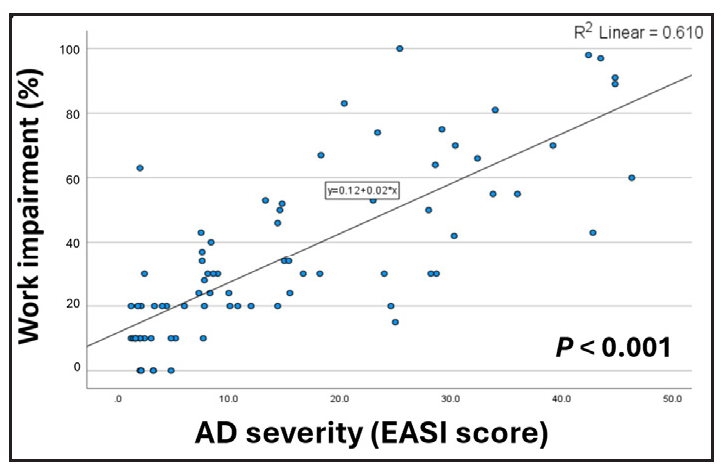
- The effects of atopic dermatitis (AD) severity based on eczema area and severity index (EASI) score, on work impairment.
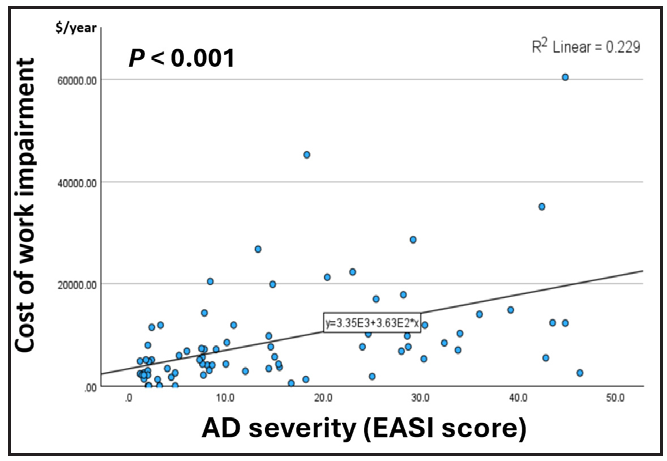
- The effects of atopic dermatitis (AD) severity based on eczema area and severity index (EASI) score, on cost.
Univariate logistic regression analysis identified several factors significantly associated with poor work performance in AD patients. Multivariable logistic regression showed significance for EASI score (aOR: 1.14, 95% CI 1.057–1.238), caffeine intake (aOR: 1.02, 95% CI 1.005–1.031), and sleep quality (aOR: 2.72, 95% CI 1.061–6.950). This final model is an excellent predictor for poor work performance which has a Receiver Operating Characteristic curve of 0.946, Hosmer-Lemeshow test of p = 0.685, and accurately classifies 84.6% of cases.
In this study, caffeine intake is associated with AD severity, poorer sleep score, and poorer work performance. While caffeine is often used to boost cognitive performance during sleep deprivation, it has been shown to reduce sleep quality, especially if consumed within 8.8 hours of bedtime.7 A cause-and-effect relationship cannot be confirmed as this was a cross-sectional study. However, the finding is noteworthy, and AD patients are advised to be cautious and avoid caffeine nine hours before bedtime.
In our study, AD affects presenteeism more than absenteeism, aligning with the previous research.5,6 This reflects the nature of AD which carries both physical and psychological aspects. Patients may not be ill enough for sick leave, but yet not well enough for optimum performance. Uncontrolled AD from a young age may lead to poor academic performance and limited educational opportunities. Consequently, individuals may find themselves confined to outdoor occupations during adulthood, which, in turn, could trigger AD flares.
In conclusion, poor sleep quality is prevalent across all AD severity. Presenteeism has a greater impact on work performance than absenteeism. Independent predictors of poor work performance include greater AD severity, poorer sleep quality, and elevated caffeine intake. This underscores the urgent need for patients, employers, and treating doctors in forming a comprehensive management strategy to address the physical symptoms of AD and its detrimental effects on sleep and work.
Ethical approval
The research/study was approved by the Institutional Review Board at the Research Ethic Committee, The National University of Malaysia, number JEP-2023-135, dated 16/3/2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This research was funded by the Universiti Kebangsaan Malaysia Medical Faculty Fundamental Grant FF-2023-097, Persatuan Dermatologi Malaysia Research Grant Award and Hoe Pharmaceuticals. The funding bodies have no role in the study design, data collection, analysis, interpretation, or in writing the manuscript.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
AI-assisted technology has been utilised to enhance the grammatical accuracy of this manuscript, ensuring clarity without any manipulation of results or analysis.
References
- Effects of disease severity on sleep and quality of life in Taiwanese patients with atopic dermatitis. JAAD Int. 2022;8:92-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Impact of depression on work productivity and its improvement after outpatient treatment with antidepressants. Value Health. 2011;14:475-82.
- [CrossRef] [PubMed] [Google Scholar]
- The world health organization health and work performance questionnaire (HPQ) J Occup Environ Med. 2003;45:156-74.
- [CrossRef] [PubMed] [Google Scholar]
- Campbell & cochrane economics methods group, EPPI-centre. CCEMG – EPPI-centre cost converter. Available from: https://eppi.ioe.ac.uk/costconversion/
- Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: An analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77:274-9.e3.
- [CrossRef] [PubMed] [Google Scholar]
- The economic and psychosocial comorbidity burden among adults with moderate-to-severe atopic dermatitis in Europe: Analysis of a cross-sectional survey. Dermatol Ther (Heidelb). 2021;11:117-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The effect of caffeine on subsequent sleep: A systematic review and meta-analysis. Sleep Med Rev. 2023;69:101764.
- [CrossRef] [PubMed] [Google Scholar]





