Translate this page into:
Atypical manifestations of disseminated cutaneous botryomycosis mimicking dermatitis herpetiformis in an immunocompetent adult woman
2 Department of Dermatology, Kubba Skin Clinic, Saket, New Delhi, India
3 Department of Dermatology, Max Smart Hospital, Saket, New Delhi, India
Correspondence Address:
Shikha Khare
A-19, Single Storey, Malka Ganj, Behind Malka Ganj Post Office, New Delhi - 110 007
India
| How to cite this article: Misri R, Khare S, Batrani M, Kar H K. Atypical manifestations of disseminated cutaneous botryomycosis mimicking dermatitis herpetiformis in an immunocompetent adult woman. Indian J Dermatol Venereol Leprol 2019;85:511-513 |
Sir,
Botryomycosis is a chronic granulomatous reaction to bacterial infections. The lesions are characterized by multiple abscesses, sinus formation, fistulas and skin ulceration, mostly caused by Staphylococcus aureus. Appropriate antibiotics, surgical drainage and excision are common methods that are employed to treat botryomycosis.
A 40-year-old female presented to the Dermatology Outpatient Department of a tertiary care hospital, with a history of severely pruritic skin lesions over the upper and lower extremities and abdomen since 3 months. Lesions initially started over the left ankle as intensely pruritic red papules. Later, lesions appeared on the right leg and abdomen within a few days. There was history of serous discharge in a few lesions following scratching. No constitutional symptoms were present. There was no history of prior insect bite, trauma, gastrointestinal disturbances, diabetes or any chronic illness.
On physical examination, multiple erythematous excoriated papules, and few crusted lesions were seen in a bilaterally symmetrical distribution on the extensor aspect of forearms, lower legs, abdomen, buttocks and upper back. [Figure - 1]. There were no lesions in the web spaces or over the genitalia and no family history of similar lesions. The diagnosis of scabies was ruled out and a provisional diagnosis of dermatitis herpetiformis was considered. Findings from routine blood investigations such as a hemogram, blood sugar profile, liver function and kidney function tests were all found to be within normal limits. Serological tests for HIV, HbsAg and hepatitis C virus antibodies were found negative. Histopathological examination from an excoriated papule on the ankle revealed a grain in the center of suppurative neutrophilic inflammation, in the mid-reticular dermis, with a mild surrounding lympho-histiocytic infiltrate. The granule was composed of clumped non-filamentous cocci with a peripheral eosinophilic rim (hematoxylin and eosin, ×400). Periodic acid–Schiff staining was negative [Figure - 2]a and [Figure - 2]b.
 |
| Figure 1: Multiple erythematous, excoriated papules and plaques, some of which are topped with a crust |
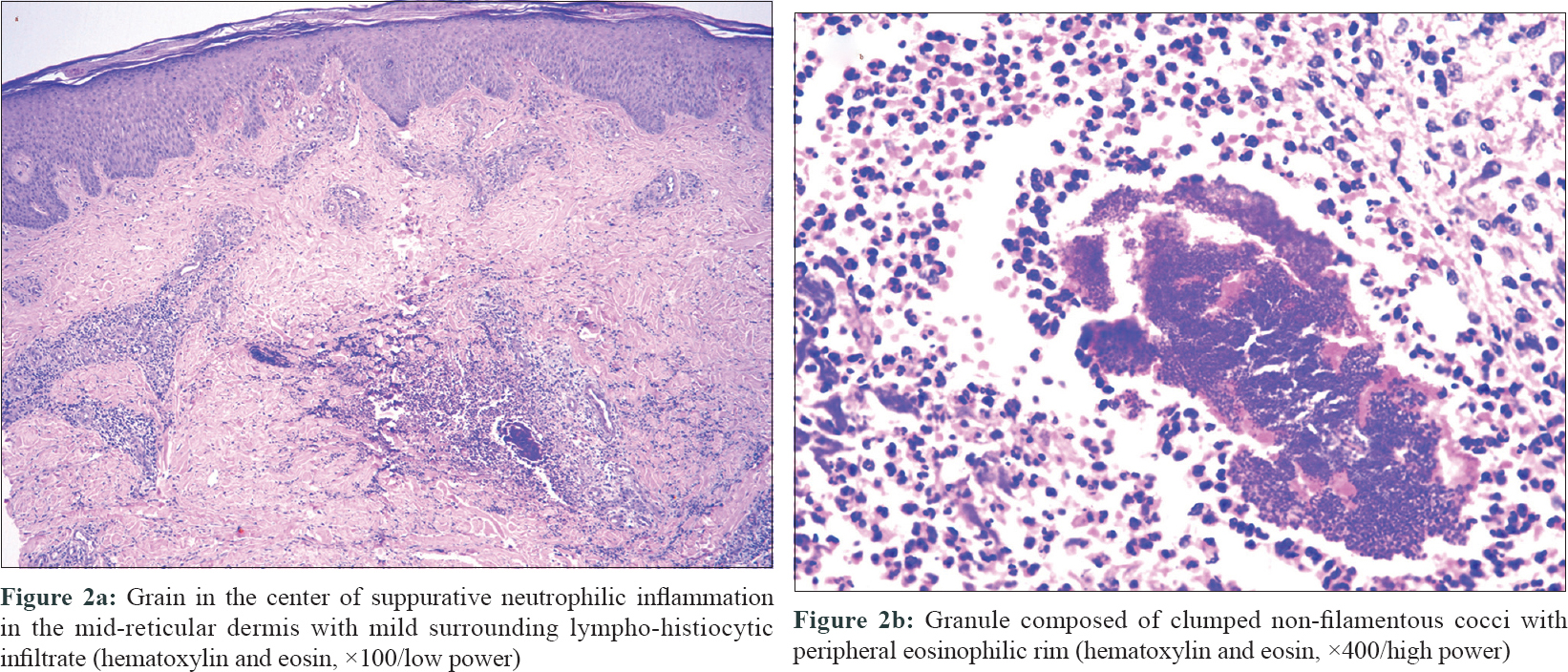 |
| Figure 2 |
Direct immunofluorescence was negative for IgG and IgA. Microbiological examination of the punch biopsy specimen showed no growth on culture. A diagnosis of cutaneous botryomycosis was made. The patient was continued on oral erythromycin and antihistamines for three more weeks along with topical fusidic acid and bland emollients, following which all the skin lesions healed with post-inflammatory hyperpigmentation [Figure - 3].
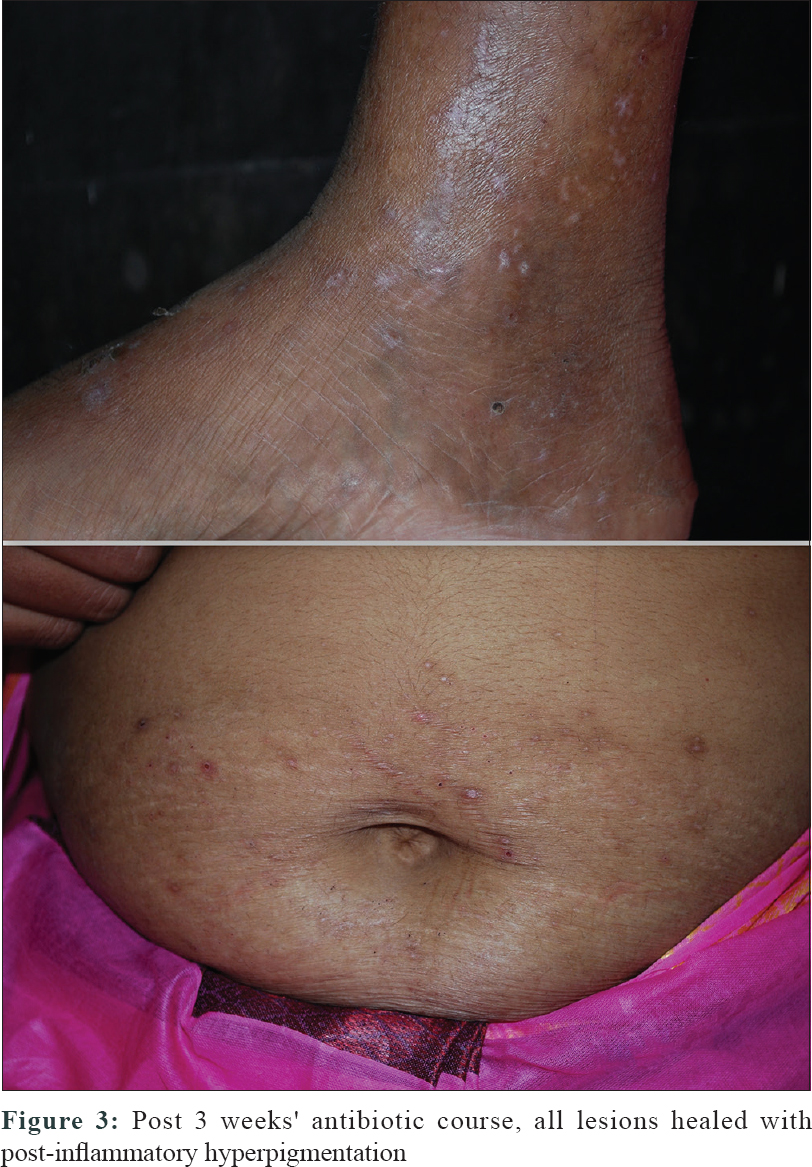 |
| Figure 3: Post 3 weeks' antibiotic course, all lesions healed with post-inflammatory hyperpigmentation |
Botryomycosis is caused by Staphylococcal aureus, but several other organisms such as Pseudomonas aeruginosa, Escherichia coli, Proteus, Propionibacterium acnes, alpha-hemolytic streptococci, peptostreptococci, Actinobacillus lignieresii and Moraxella nonliquefaciens species have been isolated singly or in combination.[1],[2],[3],[4] The proposed pathogenesis states that it could be the symbiosis of low virulence of inoculated microorganism with impaired host immunity. Predisposing factors are trauma, alcoholism, diabetes, renal disease, liver disorders, malnutrition, cystic fibrosis and immunosuppression such as in HIV.[3]
There are two forms of the disease, cutaneous and visceral. Visceral involvement occurs commonly in the lungs, although involvement of the brain, kidney, spleen and liver have been described.[5] Usually, the lesions are predominantly cutaneous and subcutaneous nodules which ulcerate, suppurate and form plaques, ulcers and sinuses, which heal slowly, and leave atrophic scars. In immunocompetent patients, lesions are found primarily on the extremities, especially in agricultural workers who do not wear footwear, and are thus subjected to repeated trauma.[6]
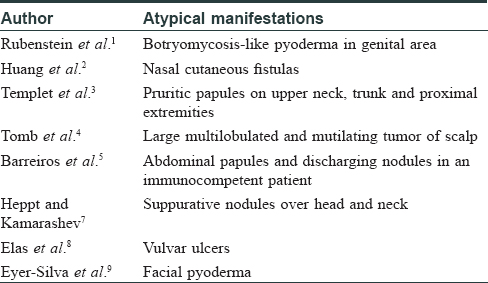
In our case, the presentation of disseminated, pruritic, excoriated papular lesions on the trunk and extremities in an immunocompetent patient is both unusual and atypical. No microbiological growth on culture was found maybe due to the fact that patient had taken oral erythromycin 500 mg QID for 7 days before the investigation. The authors found that these kind of lesions mimicking dermatitis herpetiformis have been reported only once, in prior literature.[5] In that particular case, the patient was immunocompetent and had lesions confined to the abdomen. The organism isolated was Staphylococcus aureus and the patient responded to 4 weeks of oral clindamycin therapy. Another similar case has been reported in a HIV positive patient, where the organism isolated was Staphylococcus aureus and the patient responded to 2 weeks of oral cephalexin. Other atypical manifestations of cutaneous botryomycosis have been tabulated in [Table - 1].
There is a paucity of literature on botryomycosis presenting as disseminated, itchy excoriated papules involving the trunk and extremities, which misled us in the beginning. Proper history and biopsy are warranted in patients presenting with such lesions for early diagnosis and effective treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.[9]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Rubenstein E, Krulig E, Cardenas V, Kerdel FA. Botryomycosis-like pyoderma in the genital region of a human immunodeficiency virus (HIV)-positive man successfully treated with dapsone. Int J Dermatol 2010;49:842-3.
[Google Scholar]
|
| 2. |
Huang CF, Liaw FY, Dai NT, Ou KW, Wang CC, Wang WM. Botryomycosis presenting as nasal cutaneous fistulas caused by Prevotella melaninogenica. Clin Exp Dermatol 2012;37:501-4.
[Google Scholar]
|
| 3. |
Templet JT, Straub R, Ko C. Botryomycosis presenting as pruritic papules in a human immunodeficiency virus-positive patient. Cutis 2007;80:45-7.
[Google Scholar]
|
| 4. |
Tomb RR, Stephan F, Haddad A, Choucair J. Cutaneous granular bacteriosis, a rarely diagnosed infection of the head and the neck. Clin Exp Dermatol 2009;34:887-9.
[Google Scholar]
|
| 5. |
Barreiros HM, Cunha H, Bártolo E. Photoletter to the editor: Botryomycosis in an immunocompetent woman. J Dermatol Case Rep 2013;7:29-30.
[Google Scholar]
|
| 6. |
Karthikeyan K, Thappa DM, Jeevankumar B. Cutaneous botryomycosis in an agricultural worker. Clin Exp Dermatol 2001;26:456-7.
[Google Scholar]
|
| 7. |
Heppt MV, Kamarashev J. Cervicofacial botryomycosis: Is atopic dermatitis a predisposing factor? Dermatopathology (Basel) 2014;1:81-5.
[Google Scholar]
|
| 8. |
Elas D, Swick B, Stone MS, Miller M, Stockdale C. Botryomycosis of the vulva: A case report. J Low Genit Tract Dis 2014;18:e80-3.
[Google Scholar]
|
| 9. |
Eyer-Silva WA, Silva GA, Ferry FR, Pinto JF. Facial botryomycosis-like pyoderma in an HIV-infected patient: Remission after initiation of darunavir and raltegravir. Rev Soc Bras Med Trop 2017;50:277-9.
[Google Scholar]
|
Fulltext Views
3,921
PDF downloads
1,635





