Translate this page into:
Auto-amputation of penis due to carcinoma: Still a threat in the era of modern medicine: Report of two cases
Correspondence Address:
Ramanitharan Manikandan
Department of Urology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry - 605 006
India
| How to cite this article: Ghosh B, Manikandan R, Dorairajan LN, Kumar S. Auto-amputation of penis due to carcinoma: Still a threat in the era of modern medicine: Report of two cases. Indian J Dermatol Venereol Leprol 2013;79:224-226 |
Abstract
Incidence of penile carcinoma is decreasing worldwide. Nevertheless, the incidence of penile cancer is still significant in various tropical countries, and it often presents in advanced stage. We report two unique cases of penile auto-amputation due to advanced cancer and review relevant literature. Both the patients presented with ulcerative lesion replacing penile base following automatic sloughing of the whole penis and voiding dysfunction. In addition, the first patient had metastatic inguinal lymph nodes. Supra-pubic urinary diversion was the initial management in both the patients. The first patient was treated with combined chemo-radiation, but he succumbed to death following two cycles of chemotherapy. The second patient was successfully treated with total penectomy and perineal urethrostomy. He recovered well but was lost to follow-up.Introduction
Although the incidence of penile carcinoma is low in developed countries, it continues to be a significant health problem in various tropical countries. [1] Surprisingly, despite the penis being an easily accessible organ, patients with penile cancer often present late in the disease process. The reasons for delayed presentation could be due to various social and psychological factors. Since pain is not a significant symptom in the early stages and proportionally less as compared to the extent of the disease, probably this contributes to the delay in the patient seeking medical attention. Auto-amputation of the penis has been reported after hair strangulation of penis, paraphimosis due to hemangioma and as a manifestation of ulcerative colitis. [2] Although auto-amputation of the glans penis due to advanced penile cancer is known, sloughing off of the whole penis is rare. [1] Less than ten such cases have been reported in English literature so far. [1],[2],[3] Here, we present two cases of auto-amputation of penis due to penile carcinoma.
Case Reports
Case 1
A 40-year-old male farmer presented with a history of automatic shedding-off of his penis one and half months ago. He had initially developed a few small ulcers around the base of his penis, which gradually turned into pus-discharging wounds. These slowly coalesced to form a circumferential ulcer around the root of the penis, and ultimately the whole penis sloughed off leaving an ugly-looking ulcer. He had severe voiding symptoms along with dysuria. He did not have any known co-morbidities. He was initially treated with some traditional herbal medications. He reported to us due to increasing difficulty in passing urine. On examination, there was a foul-smelling, pus-discharging ulcer, replacing the base of his penis [Figure - 1]. The margins of the ulcer were rolled out, and the base was indurated with infected slough at the floor. The urethral orifice could not be made out separately. There were multiple, bilateral, fixed, non-tender inguinal lymph nodes (largest 2 cm). Laboratory values were within normal limits, except for anemia (Hb- 8 gm %) and elevated ESR (104 mm, 1st hr). Chest x-ray and abdominal ultrasound was normal. Incisional biopsy from the ulcer margin showed features of an infiltrating well-differentiated squamous cell carcinoma, and fine needle aspiration cytology (FNAC) from inguinal lymph nodes confirmed bilateral metastatic involvement. Initially, the patient underwent a supra pubic urinary diversion. He declined to accept the option of total penectomy with perineal urethrostomy. Hence, he was planned for combined modality treatment with radiotherapy and chemotherapy. With radiotherapy, his wound showed signs of regression, but he succumbed to extensive disease after 2 cycles of chemotherapy.
 |
| Figure 1: Complete absence of penis and ulcer replacing penile base |
Case 2
A 65-year-old chronic smoker presented with a history of his penis having sloughed off three months ago. He had a foul-smelling genital discharge and severe voiding symptoms. He initially developed a small ulcer over the root of his penis six month earlier, which gradually increased in size. Ultimately, the penis sloughed off from the base, leaving a raw wound. He did not have any systemic symptoms. Physical examination revealed a pus-discharging, ulcero-proliferative growth at the penile base encroaching on to the scrotal skin [Figure - 2]. The base of the ulcer was not fixed to the surrounding tissue. Bilateral testes and epididymis were normal. There were bilateral, multiple, mobile, non-tender inguinal lymph nodes (maximum diameter 1.5 cm). Laboratory values were normal. Ultrasonography of the abdomen was normal. A wedge biopsy from the tumor showed a well-differentiated squamous cell carcinoma [Figure - 3], and FNAC from the inguinal lymph nodes suggested reactive hyperplasia. A suprapubic urinary diversion was done initially. Total penectomy and perineal urethrostomy was done as definitive therapy. The patient successfully recovered from the surgery but was subsequently lost to follow-up.
 |
| Figure 2: Ulcero-proliferative growth encroaching scrotum with absence of penis |
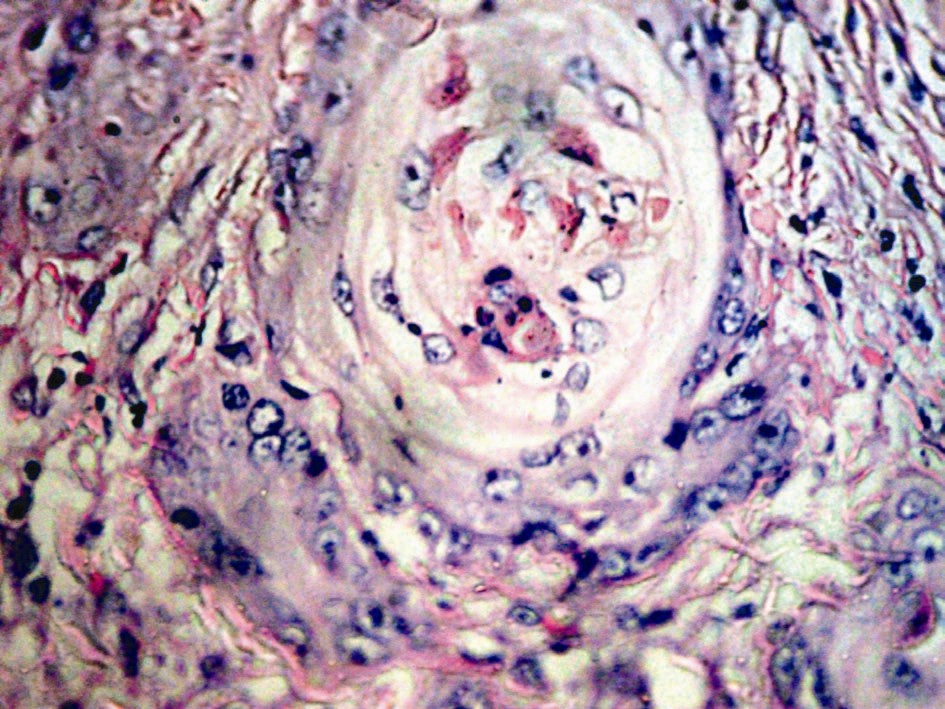 |
| Figure 3: Higher magnification view of well-differentiated squamous cell carcinoma (H and E stain, 40X) |
Discussion
The majority of penile cancers are squamous cell carcinomas. [1] It follows an indolent process, and widespread dissemination is infrequent until very late in the course of the disease as the Buck′s fascia acts as a barrier to direct tumor spread. Primary excision is the treatment modality of choice for penile carcinoma. Organ preserving surgeries can be considered in patients with small, superficial tumors, whereas total amputation is the standard of care for large and invasive lesions. Ilio-inguinal lymph node dissection is the standard treatment for metastasis to inguinal lymph nodes. [4] Radiotherapy and chemotherapy usually have an adjuvant role, except for some cases. Irrespective of the tumor stage, grade, and treatment modalities, the average 3, 5, and 10 year survival rates are 59%, 52%, and 32%, respectively. But, in untreated patients, the survival rates fall sharply to around 6%. [2],[3]
Penile gangrene and subsequent auto-amputation is known to develop in diabetics and end-stage renal disease patients. [5] The cause of penile auto-amputation in advanced penile cancer could be vasculogenic due to blockade of end arteries with tumor emboli or direct tumor invasion. Most common presentation of penile cancer is as an ulcerative or exophytic lesion over glans penis or prepuce. Only less than 2% of patients present with an initial lesion on the penile shaft. [4] So, even if the patient presents in an advanced stage of disease, auto-amputation of the whole penis is very rare. Both of our patients presented late in the course of disease because of lack of awareness and social reasons. Definite treatment protocol for such patients with auto-penectomy is unavailable since all the available literatures are isolated case reports or small series. Surgical excision of the primary tumor should be contemplated whenever feasible. Sometimes, rotational flaps may be of help to cover the wound following wide local excision. If the primary tumor is fixed to the underlying structures, then primary radiotherapy can be considered. Neo-adjuvant chemotherapy with Taxanes is recommended for patients with unresectable tumor or fixed, enlarged lymph nodes. [6] Considering the grave prognosis of such cases, only palliative treatment can be offered. [1]
Despite the diagnostic and therapeutic advancement in cancer management and the fact that penile cancer is potentially curable, it is truly regrettable that such delayed presentation and poor follow-up with dismal prognosis continue to exist. Only improvement in social awareness can lead to timely and apt treatment of penile cancer to prevent the occurrence of such unfortunate cases.
| 1. |
Agarwal P, Sharma D. Auto destruction of penis due to carcinoma. J Eur Acad Dermatol Venereol 2005;19:220-2.
[Google Scholar]
|
| 2. |
Chiu WK, Chuang FP, Wu ST, Cha TL, Lee SS. Auto-amputation of penis due to carcinoma. ANZ J Surg 2009;79:89-90.
[Google Scholar]
|
| 3. |
Pettaway CA, Lynch DF, Davis JW. Tumors of the penis. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh Urology. 9 th ed. Philadelphia: Saunders-Elsevier; 2007. p. 959-92.
[Google Scholar]
|
| 4. |
Pizzocaro G, Algaba F, Horenblas AS, Solsona E, Tana S, Van Der Poel H, et al. EAU penile cancer guidelines 2009. Eur Urol 2010;57:1002-12.
[Google Scholar]
|
| 5. |
Rajaian S, Gopalakrishnan G, Kekre NS. Auto-amputation of Penis Due to Advanced Penile Carcinoma. Urology 2010;75:253-4.
[Google Scholar]
|
| 6. |
Vijayan P. Gangrene of the penis in a diabetic male with multiple amputations and follow up. Indian J Urol 2009;25:123-5.
[Google Scholar]
|
Fulltext Views
3,541
PDF downloads
1,143





