Translate this page into:
Autoinoculation as a treatment modality for molluscum contagiosum: A preliminary uncontrolled trial
Correspondence Address:
Gauri Vats
Room No 35, PG Hostel, MDM Hospital Campus, Jodhpur, Rajasthan
India
| How to cite this article: Kachhawa D, Sonare D, Vats G. Autoinoculation as a treatment modality for molluscum contagiosum: A preliminary uncontrolled trial. Indian J Dermatol Venereol Leprol 2018;84:76-78 |
Sir,
Molluscum contagiosum (MC) is a self-limiting skin infection caused by poxvirus, commonly seen in children with a prevalence of 8–12%. Infection follows contact with infected persons or contaminated objects, and the diagnosis is clinical. Homologous autoimplantation is a simple technique which helps in inducing a cell-mediated immune responseto the antigens, aiding clearance of both local and distant lesions. Previous experience of good clearance of verruca vulgaris by autoimplantation prompted us to assess the utility of this technique in molluscum contagiosum.
A prospective study was conducted in the Department of Dermatology of MDM hospital, Dr SN medical college, Jodhpur for 6 months among 58 patients. The patients were subjected to complete work up including detailed history and examination of lesions. Except lactating mothers, pregnant/immunosuppressed patients, and those with a history of intake of immunomodulatory/immunosuppressive drugs we included all clinically diagnosed cases in our study. Institutional ethical clearance and proper written consent was obtained after counseling, and a treatment free washout period of 3 months was ensured. A single session of autoinoculation was performed. The patients were followed up at 7 days, and thereafter every 2 weeks for 3 months to look for clearance and another 3 months to check for relapse.
The response to therapy was graded as follows:
- Excellent, >75% of lesions disappeared
- Good, 51–75% lesions disappeared
- Average, 26–50% lesions disappeared
- Poor <25% lesions disappeared.
A well-developed lesion was chosen as a donor, under topical anesthesia, and using all aseptic precautions, it was approached using an insulin syringe and pierced from a site just adjacent to the lesion. It was then repeatedly punctured from within 5–7 times to expose the contents of the molluscum body to the dermis by crossing basement membrane, hence inoculating and exposing the viral antigen to the immunological surveillance system. After the procedure fusidic ointment was applied locally over the punctured site [Figure - 1].
 |
| Figure 1: Puncturing of lesion form within |
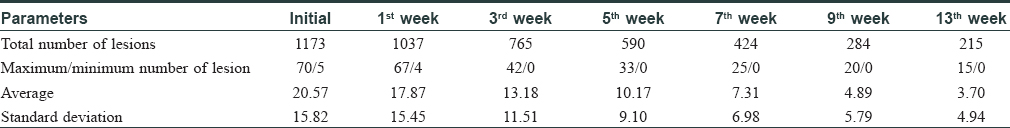
A total of 32 (55.2%) patients showed complete resolution of the lesions within 3 months. There was partial response (sappearnce of some lesions) in, 19 patients (32.8%) and seven (12.1%) patients had no improvement [Figure - 2]. Maximum response was seen after the 7th week of therapy. None of the patient showed relapse or development of a new lesion at a different site. Few patients developed hyperpigmentation at the site of autoimplantation which faded with time. The age-wise response of autoinoculation was analyzed at the end of 12 weeks [Figure - 3]. We also noted the total number of lesions, mean, standard deviation, and range of number of lesion at each follow-up visit. A steady decrease in both the total and mean number of lesions was observed [Table - 1] and [Figure - 4]. Local adverse events were mild erythema, edema, and postinflammatory hyperpigmentation.
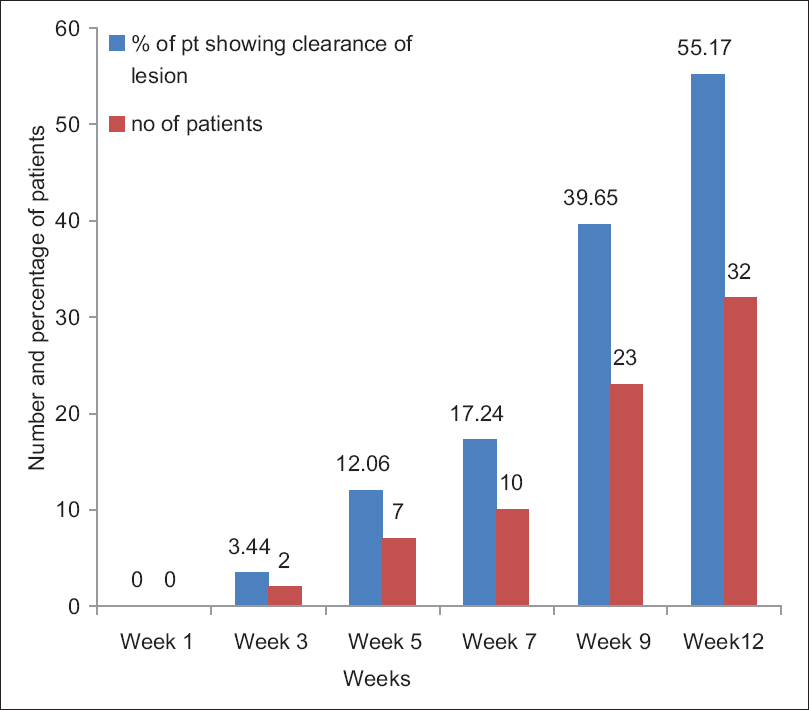 |
| Figure 2: Percentage of patients who showed clearance of lesions. week: End of week |
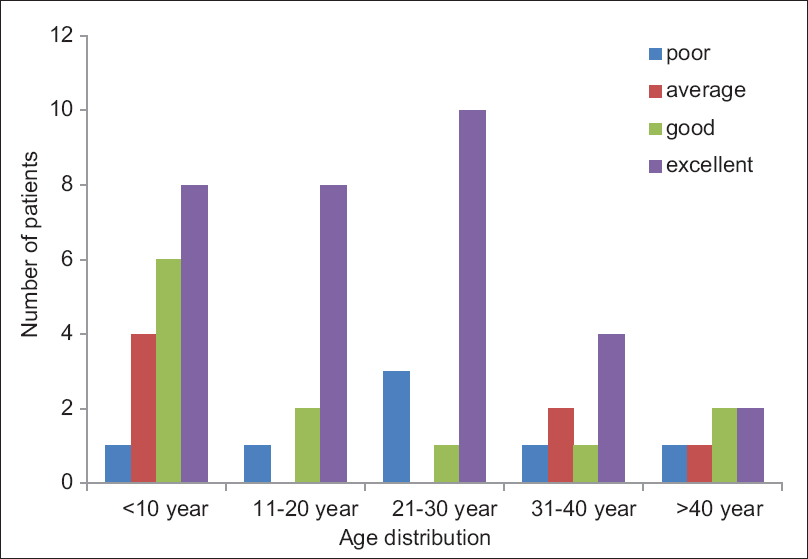 |
| Figure 3: Response to autoimplantation in various age groups at the end of 12th week |
 |
| Figure 4: The response at 1st and 3rd week of autoinnoculation |
The molluscum virus infection is localized to the epidermal layers where it induces a typical, complex hyperproliferative lesion with an abundance of virus particles but a conspicuous, absence of immune response. By not crossing the basement membrane the virus evades immune surveillance. The lesions are often self-limiting as most of them resolve without treatment, with the average length of infection lasting between 6 and 18 months.[1] Physical destruction has been recommended as the preferred method for treatment by many authors.[2] Lesion eradication may also be attempted chemically (trichloroacetic acid, tretinoin) or immunologically (imiquimod), inciting an inflammatory response which upregulates the immune system to clear the infection.[3] Topical cidofovir has been used in the immunosuppressed population but has not been systemically studied in the general population.[4],[5]
Hence, for effective control, there should be immune stimulation which can lead to long-term immunity against the virus. Molluscum virus is an orthopox virus which is closely related to varicella and vaccinia viruses, and a similar approach has been successful in generating immune response againsta vaccinia and varicella viruses by vaccination.
Various studies on autoimplantation in warts were shown to be associated with the production of Th1 cytokines (TNF-α, and IL-1) which downregulate the transcription of genes whereas INF-γ and IL-2 stimulate cytotoxic T cells and natural killer cells to eradicate the infected cells.[6]
Limitations of our study were a small sample size, lack of controls to assess spontaneous resolution, and lack of serotyping of persistent lesions or checking for serospecific antibodies. Spontaneous clearance of molluscum lesions during the trial could not be excluded, and thus a placebo controlled trial would be necessary to establish the exact therapeutic efficacy.
The modified technique of autoimplantation of molluscum is a safe, effective, and rapid procedure for its treatment. Our study indicates that autoinoculation therapy holds promise in the management of this infection. Being an easy day-care procedure, it is also a cost-effective option.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that name and initial will not be published and due efforts will be made to conceal patient identity, however, anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Seo SH, Chin HW, Jeong DW, Sung HW. An open, randomized, comparative clinical and histological study of imiquimod 5% cream versus 10% potassium hydroxide solution in the treatment of molluscum contagiosum. Ann Dermatol 2010;22:156-62.
[Google Scholar]
|
| 2. |
Theiler M, Kempf W, Kerl K, French LE, Hofbauer GF. Disseminated molluscum contagiosum in a HIV-positive child. Improvement after therapy with 5% imiquimod. J Dermatol Case Rep 2011;5:19-23.
[Google Scholar]
|
| 3. |
Myskowski PL. Molluscum contagiosum. New insights, new directions. Arch Dermatol 1997;133:1039-41.
[Google Scholar]
|
| 4. |
Ohkuma M. Molluscum contagiosum treated with iodine solution and salicylic acid plaster. Int J Dermatol 1990;29:443-5.
[Google Scholar]
|
| 5. |
Gottlieb SL, Myskowski PL. Molluscum contagiosum. Int J Dermatol 1994;33:453-61.
[Google Scholar]
|
| 6. |
Sterling JG, Kurt JB. Viral infection. In: Textbook of Dermatology. In: Champion RH, Burton JL, Ebling FJ, editors. 6th ed. Oxford: Blackwell Science Ltd.; 1998. p. 995-1095.
[Google Scholar]
|
Fulltext Views
8,079
PDF downloads
3,073





