Translate this page into:
Autologous noncultured melanocyte-keratinocyte transplantation in stable vitiligo: A randomized comparative study of recipient site preparation by two techniques
2 Department of Dermatology, Maulana Azad Medical College, Lok Nayak Hospital, New Delhi, India
Correspondence Address:
Vineet Relhan
Department of Dermatology, Maulana Azad Medical College, Bahadur Shah Zafar Marg, New Delhi - 110 002
India
| How to cite this article: Gupta S, Relhan V, Garg VK, Sahoo B. Autologous noncultured melanocyte-keratinocyte transplantation in stable vitiligo: A randomized comparative study of recipient site preparation by two techniques. Indian J Dermatol Venereol Leprol 2019;85:32-38 |
Abstract
Background: Accurate preparation of recipient area is a critical step in melanocyte-keratinocyte transplantation procedure for vitiligo. It is an important potential step for adaptation in the quest to achieve better results and ablative lasers potentially offer excellent precision over margin and depth control in achieving that.
Objective: To compare between the two techniques used for recipient site preparation: Er:YAG laser ablation and mechanical dermabrasion for melanocyte-keratinocyte transplantation procedure in terms of re-pigmentation achieved and adverse effects seen.
Methods: A randomized comparative trial was performed among 32 patients of stable vitiligo undergoing melanocyte-keratinocyte transplantation procedure. In Group A (n = 15), recipient site preparation was done with Er:YAG laser, and in Group B (n = 17), it was done with a motorized dermabrader. Patients of both groups were objectively assessed for re-pigmentation at 1, 3 and 6 months.
Results: A total of 253.696 cm2 of depigmented surface was operated upon and re-pigmentation of 125.359 cm2 (49.4%) was achieved. On comparison between two groups, no statistical difference was found with respect to total re-pigmentation achieved (Group A: 54.67% vs Group B: 48.841%, P = 0.663) and grades of re-pigmentation achieved (P = 0.796). Occurrence of adverse events was also statistically similar in both the groups.
Conclusion: This study did not reveal any statistically different outcome (in terms of re-pigmentation and adverse effects) between the two methods of recipient site preparation – motorized dermabrasion and Er:YAG ablation.
Limitations: This study is small and larger studies are needed to ascertain the benefit of Er:YAG for recipient site preparation. Future studies may also ascertain variables such as time taken to prepare the recipient area, nature of bleeding, postoperative healing, difficulties in specific area, cost of the procedure, patient comfort and ease of the surgeon, rather than comparing the re-pigmentation alone.
Introduction
Vitiligo is a disorder of pigmentation which affects 0.4–2% of the worldwide population.[1] Surgical therapies are recommended for patients with stable vitiligo who wish speedier re-pigmentation and/or are not responding sufficiently enough with medical therapies and phototherapy. Autologous noncultured melanocyte-keratinocyte transplantation is a cellular grafting technique, whereby a cellular suspension of epidermal basal layer-derived melanocytes and keratinocytes is obtained from normally pigmented donor skin. The cellular suspension is then applied to the diseased depigmented recipient sites after de-epithelization. Gauthier and Surleve-Bazeille first described this method in 1992.[2] Since then, various modifications have been suggested. In 1998, Olsson and Juhlin suggested addition of a melanocyte culture Dulbecco's modified Eagle medium (F12) to the suspension. They also introduced trypsinization at 37°C that reduced the duration of trypsinization from overnight to 50 min.[3] In 2001, van Geel et al. suggested another modification by complementing the cell suspension with hyaluronic acid, which allowed better adherence of cells to the grafted surfaces.[4] In 2003, Mulekar presented consistently effective use of the noncultured epidermal suspensions in a large number of patients using a simple incubator instead of an expensive CO2 incubator.[5]
In all grafting methods (tissue or cellular), preparation of the recipient lesion site is done by separating the epidermis from dermis to place new melanocytes at the dermo-epidermal junction. To achieve this, several modes of de-epithelization have been described, including induction of blisters by suction, liquid nitrogen application, psoralen & UVA (PUVA)-induced blisters, programmed diathermal surgical procedure, manual or motorized dermabrasion and laser-induced epidermal ablation.[6],[7],[8],[9],[10],[11] Irregular lesions particularly on delicate sites pose a critical problem for utilization of blisters (suction/liquid nitrogen) and mechanical abrasion. Laser-assisted dermabrasion offers precise removal of the epidermis. A large, uneven surface can be denuded into bloodless, smooth raw surface in a short time while accurately controlling the depth of tissue ablation. The two widely used ablative lasers in dermatology are carbon dioxide (CO2) and erbium-doped yttrium-aluminum-garnet (Er:YAG). The absorption coefficients of the Er:YAG and CO2 lasers are 12,800/cm and 800/cm, respectively, making the Er:YAG laser 12–18 times more efficiently absorbed by water-containing tissues than the CO2 laser.[12] Because the water-containing epidermis effectively absorbs the Er:YAG laser, this laser system is a more precise ablative tool, creating narrower zones of residual thermal necrosis.[11] Furthermore, there is a direct relationship between fluence delivered and tissue ablated: 2–5 μm of tissue is vaporized with each J/cm2 depending on the device, which allows the surgeon to precisely control the depth of ablation.[13]
Kaufmann et al. first used the Er:YAG laser to prepare recipient vitiligo sites and applied cultured melanocytes over them achieving good-to-excellent re-pigmentation in 55.55% sites treated.[9] Guerra et al. performed autologous cultured epidermal grafting over Er:YAG ablated achromic lesions in 21 patients of stable vitiligo. They achieved an average re-pigmentation of 75.9% over 6 months of follow-up.[10] Pianigiani et al. performed autologous cultured epidermal grafting over Er:YAG ablated vitiligo lesions in 93 patients. They also combined this procedure with postoperative narrowband ultraviolet B phototherapy and achieved re-pigmentation in 75% patients with focal and segmental vitiligo and in 30% patients with generalized vitiligo.[14] Fioramonti et al. performed autologous cultured melanocytes transplantation in a single patient over two lesions, de-epithelizing them with different methods – Er:YAG laser ablation and dermabrasion. They achieved poor pigmentation in the lesion treated with dermabrasion compared to that treated by Er:YAG.[12]
Despite having many different techniques to prepare the recipient site, there are very limited comparisons studies available in the literature that compare between different techniques and their effect on re-pigmentation outcomes. This study attempts to compare between the two techniques used for recipient site preparation in melanocyte-keratinocyte transplantation procedure – Er:YAG laser ablation and mechanical dermabrasion – in terms of re-pigmentation achieved and adverse effects seen.
Methods
This study was conducted among patients attending the Vitiligo Clinic at the Department of Dermatology, Maulana Azad Medical College and associated Lok Nayak Hospital, New Delhi between November 2012 and March 2014. The protocol of the study was presented to and duly approved by the Institutional Ethics Committee. Patients underwent history, general physical examination and a thorough dermatological survey. The minimum cut-off period of stability was taken as 1 year (i.e. no history of new lesions/increase in the size of existing lesions/koebnerization for the last one year). Exclusion criteria were keloidal tendency, extensive body surface area involvement, i.e. >50% body surface area, active infections and patients with bleeding diathesis. Patients >12 years of age, having clinically stable disease and otherwise fit for vitiligo surgeries were given the option of participating in the study. They were diligently informed about the procedure, the nature of the study and the risks/benefits involved. Those consenting and meeting the aforementioned criteria were randomized in the order of their presentation into two groups by using a computer-generated random number sequence for a two-arm study. Allocation concealment was done by using opaque (serially numbered) presealed envelopes, which were opened on the day of the surgery.
Preparation of cell suspension
A normally pigmented donor area of one-third to one-tenth of the recipient area size was selected preferably on the lateral aspect of the gluteal region. The area was then cleaned with 70% ethanol and povidone-iodine. It was then anesthetized with 1% lignocaine injected locally. The skin was stretched and a very superficial sample of approximately 200 μm thickness was obtained with the help of a skin grafting knife. Superficial wound on the donor area was dressed by framycetin sulfate dressing. The skin sample was transferred to a petri dish containing approximately 4 ml of 0.2% w/v Trypsin-ethylenediaminetetraacetic acid solution (HiMedia® Laboratories, Mumbai, India) so that the sample was completely immersed in the solution. Sample was placed with epidermis upwards and care was taken to avoid folds and to ensure that it remained properly soaked in the solution. The petri dish was incubated for 50 min at 37°C. After incubation, the graft was thoroughly washed thrice in 1 ml trypsin inhibitor (HiMedia® Laboratories, Mumbai, India) and 3 ml phosphate-buffered saline thrice. The graft was then transferred to a petri dish containing Dulbecco's modified Eagle/F-12 medium (HiMedia® Laboratories, Mumbai, India). The dermis was separated from the epidermis and was discarded. The epidermis in the petri dish was broken down into multiple small pieces with the help of fine iris scissors, and then transferred to a 15-ml conical bottom test tube along with the medium. Now, the test tube containing the epidermal pieces was vigorously shaken for 10 s and subjected to centrifugation at 2,000 rpm for 6 min. Thus, a cell pellet was achieved at the bottom of the tube. The remnant epidermal pieces along with the medium were discarded and the cell pellet was re-suspended in 0.5–1 ml of Dulbecco's modified Eagle medium/F-12 medium. This suspension was then transferred to a 1 ml syringe with the help of a pipette.
Recipient site preparation
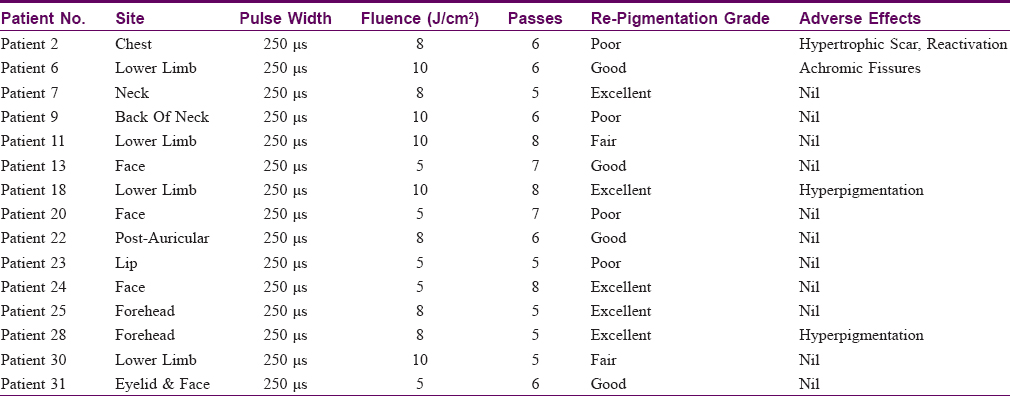
The recipient area was marked out with a marker, cleaned with povidone-iodine and 70% ethanol and anesthetized with 1% lignocaine [Figure - 1]: Consort Diagram]. In the first randomly selected group (Group A), recipient site was ablated till the dermo-epidermal junction (till pinpoint bleeding spots appear) by Er:YAG laser (MCL-30 Dermablate®, Asclepion Laser Technologies GmbH®, Jena, Germany) using appropriate energy and fluence settings. This device is a 2940-nm laser with fixed pulse duration of 250 μs. Moreover, there is a direct relationship between fluence delivered and tissue ablated: 4–5 μm of tissue is vaporized with each J/cm2 in this device. The parameters used for Er:YAG ablation can be found in [Table - 1].
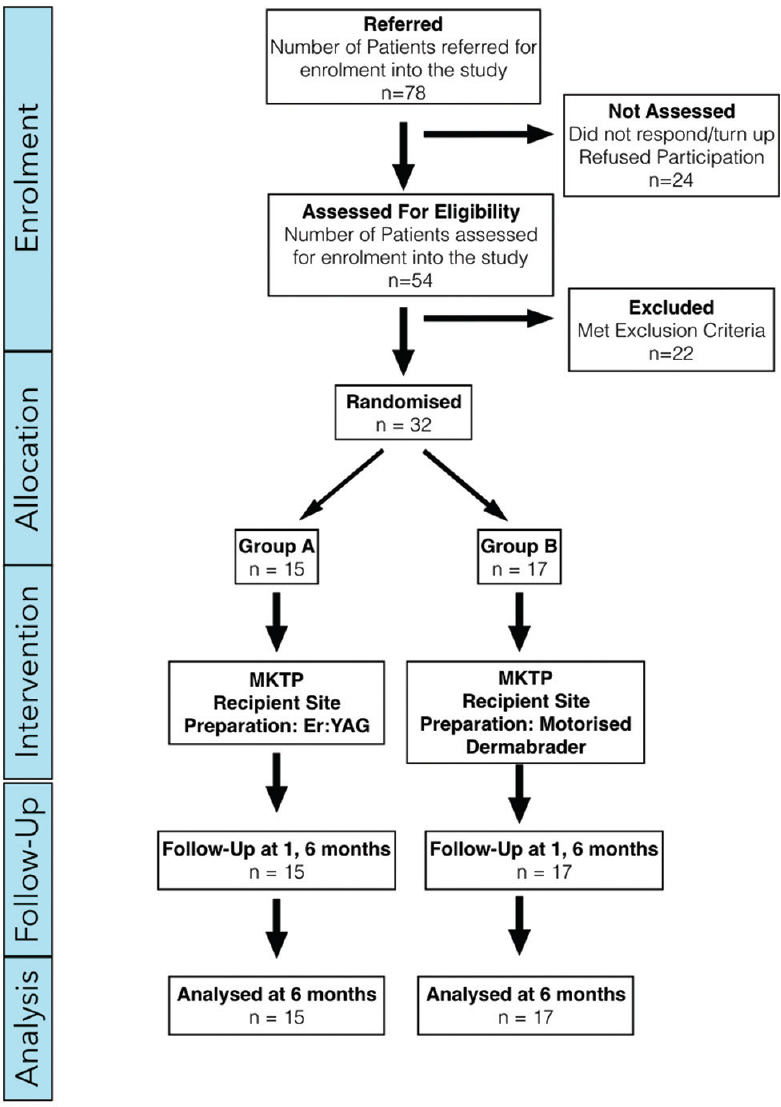 |
| Figure 1: Consort diagram depicting timeline of the study |
In the second randomly selected group (Group B), the recipient area was abraded down to the dermo-epidermal junction with a variable speed micro-motor dermabrader fitted with diamond fraises. The speed of the motor dermabrader varied from 15,000 rpm (for sites such as dorsum of feet) to 5,000 rpm (for sites such as lips). The denuded area in both the groups was then covered with gauze pieces soaked in normal saline until bleeding ceased.
Cell suspension was applied evenly on the denuded skin and covered with a collagen sheet. It was further covered with sterile gauze pieces and held in place with adhesive dressing.
Outcome evaluation and follow-up
Patients of both the groups were objectively assessed for re-pigmentation at 1 month, 3 months and 6 months. On every follow-up visit, digital photographs and measurements of the affected sites were taken. Photographs of before surgery and 6 months postsurgery were analyzed with the help of software ImageJ 1.47v (National Institutes of Health, USA) and depigmented area measured. An independent observer also assessed the patient.
Re-pigmentation was measured in terms of percentage of the original area of depigmentation and was graded as excellent (>80%), good (51–80%), fair (31–50%) and poor (<30%). Results were compared between the two groups. Patients of both the groups were also monitored for any adverse effects that might arise during the course of treatment and their occurrence was recorded for comparison between the two groups. Time of onset of pigmentation was also noted.
Statistical evaluation
The data were collected in a predesigned format and summarized as frequencies, percentages and proportions. Baseline characteristics of two groups were compared – nominal data with Chi-square tests and scale data with independent samples t-tests. Percentage area re-pigmented was compared with independent-samples t-test. Degree of re-pigmentation between groups was compared with Mann–Whitney Wilcoxon rank-sum test. Complication occurrence was compared with Chi-square test. Correlation tests were also done between re-pigmentation achieved and duration and stability of disease by Pearson's and Spearman's correlation analysis. P value <0.05 was considered significant. All descriptive and analytical statistics were done using Microsoft® Excel® 2013 and IBM® SPSS® Statistics Version 22.
Results
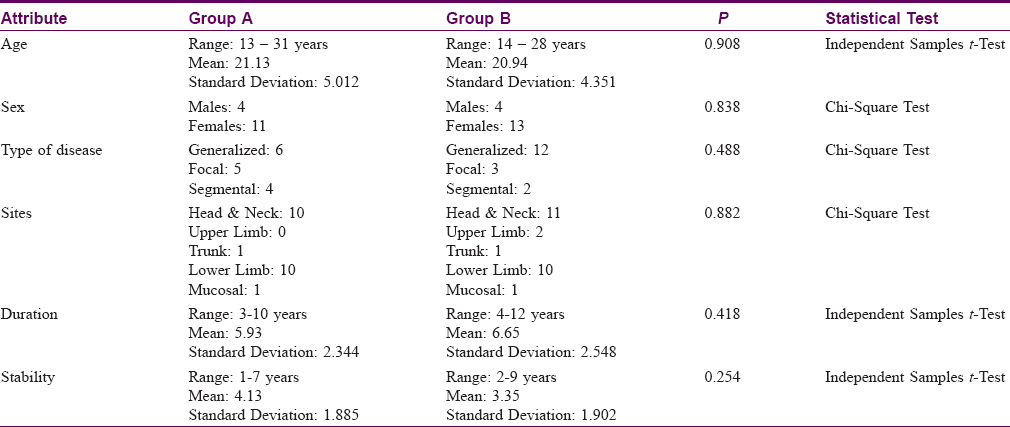
A total of 32 patients were enrolled into the study and operated. Age of patients ranged from 13 to 31 years, mean age being 21.03 years (standard deviation = 4.597). The disease duration varied from 3 to 12 years, mean being 6.31 years (standard deviation = 2.442). Baseline characteristics were compared within the two groups and found not to be significantly dissimilar [Table - 2]. Many patients in our study were having an ongoing re-pigmentation at 6 months postsurgery and even developed further re-pigmentation afterwards. However, results and comparison presented in this paper are of only until 6 months after the surgery.
In Group A (recipient site preparation by Er:YAG), a total of 95.956 cm2 skin surface was operated upon in 15 patients and 22 lesions. Re-pigmentation of 46.758 cm2 (54.7%) was achieved. Five (33.3%) patients achieved excellent re-pigmentation. Four (26.7%), two (13.3%) and four (26.7%) achieved good [Figure - 2], fair and poor re-pigmentation, respectively.
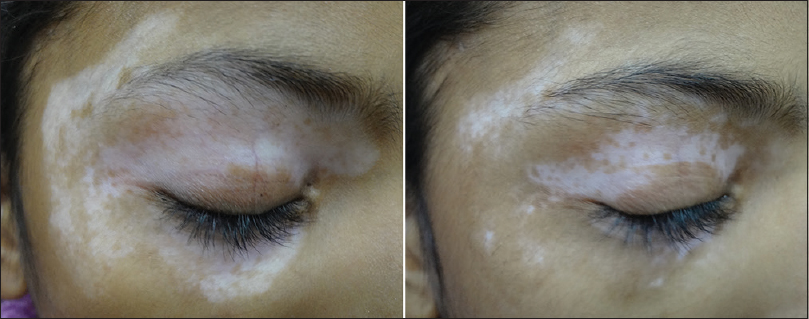 |
| Figure 2: Good re-pigmentation over periorbital region in Group A (erbium-doped yttrium-aluminum-garnet laser) after 6 months of surgery |
In Group B (recipient site preparation by motorized dermabrasion), a total of 157.74 cm2 skin surface was operated on 17 patients and 25 lesions. Re-pigmentation of 78.601 cm2 (48.8%) was achieved. Six (35.3%), four (23.5%) and seven (41.2%) patients achieved excellent, good and poor re-pigmentation, respectively [Figure - 3].
 |
| Figure 3: Excellent re-pigmentation over lower leg and foot in Group B (dermabrasion) after 6 months of surgery |
On comparison with respect to total re-pigmentation achieved (Group A: 54.7% vs Group B: 48.8%), the difference was not found to be statistically significant (P = 0.663, independent-samples t-test). With respect to grades of re-pigmentation achieved by different patients also, no statistically significant difference was found between the two groups (P = 0.796, Mann–Whitney U test).
Few adverse effects were noted in both the groups. Four patients in Er:YAG group and three patients in the dermabrasion group developed complications. Two patients each in both groups developed hyperpigmentation. One patient in Group A had achromatic fissures and one patient in Group B had scarring. A Single patient in the Er:YAG group, operated on the chest region developed scarring and re-activation of disease (appearance of new depigmented lesions around the operated lesion). Occurrence of complications was statistically similar in both the groups (P = 0.538, Chi-square test).
Re-pigmentation onset ranged from 15 to 60 days. Mean time of onset of re-pigmentation was 36.30 days (standard deviation = 16.734). Mean time of onset in Er:YAG group and dermabrasion group was 40.91 and 32.08 days, respectively. However, this difference was not statistically significant (P = 0.214, independent samples t-test).
In our study, segmental vitiligo showed most favorable response with 66.7% lesions achieving excellent re-pigmentation and 33.3% lesions achieving good re-pigmentation. This was followed by focal (25% excellent; 25% good; 25% fair and 25% poor) and generalized (27.8% excellent; 22.2% good and 50% poor). There was no significant difference in re-pigmentation among the groups of study for different types of vitiligo.
61.9% lesions at head and neck showed excellent to good re-pigmentation. Both the lesions operated on upper limb showed excellent re-pigmentation. 50% lesions operated on lower limb showed excellent to good re-pigmentation. Both the lesions operated on the mucosal surface (lip) showed poor re-pigmentation. One lesion operated upon the trunk showed good re-pigmentation, while the other showed poor re-pigmentation. No statistically significant difference for re-pigmentation on different sites was found among the groups of study.
Discussion
Autologous noncultured melanocyte-keratinocyte is a well-established surgical modality for stable vitiligo worldwide. This procedure holds the distinct ability of treating extensive areas in a single sitting from a relatively small donor graft. Over time, by innovation and contribution of various workers from around the world, the procedure has been simplified and cost significantly reduced. Now, this procedure is considered as an optimal surgical option by internationally published guidelines.[15] However, the nuances of vitiligo surgery are in a constant state of evolution with the quest to obtain technical simplicity and long-standing, uniform, recipient site dominated pigmentation with minimal side effects. Preparation of recipient site is a critical step in any vitiligo surgery, even more so in epidermal cell suspensions as recipient site conditions determine the fate of transplanted basal layer cells. It is important for the skin surface at the recipient site to be abraded uniformly till appropriate depth. Laser-assisted ablation offers precise removal of the epidermis and depth of tissue ablation can be well controlled. The 2940 nm Er:YAG laser has the ability of achieving precise and rapid de-epithelization without coagulating the recipient bed. This property also helps in regulating the depth of ablation by allowing detection of the pin-point bleeders as soon as they appear.
This randomized comparative study evaluates the use of Er:YAG laser in recipient site preparation vis-à-vis motorized dermabrader. No significant difference in terms of total re-pigmentation achieved, grades of re-pigmentation or adverse effects were noted between the two groups. One patient from Er:YAG group operated on chest developed hypertrophic scarring and reactivation of disease. Although the patient did not have any report of previous keloidal tendency and also fulfilled the stability criterion for inclusion, the adverse outcome suggests that there is a need to exercise special caution before operating a lesion on a region-like chest, which is prone to hypertrophic scarring. Mulekar has also reported “Reactivation” of disease after National Childhood Encephalopathy Study once in a single patient in a study.[8] Stability should be more rigorously examined before selecting patients for vitiligo surgery. In our study, the duration of stability correlated with moderate strength with the grade of re-pigmentation (Spearman's rank order coefficient (ρ) = +0.501 at P = 0.003) and re-pigmentation percentage achieved (Pearson's correlation coefficient (r) = +0.442 at P = 0.011) [Figure - 4]. This was seen irrespective of the mode of recipient site preparation. However, because stability in vitiligo does not still have a unanimous definition, it is safe to assume that more the duration of stability, higher the chances of a favorable outcome. This is in concordance with the findings of Rao et al. regarding stability in vitiligo.[16]
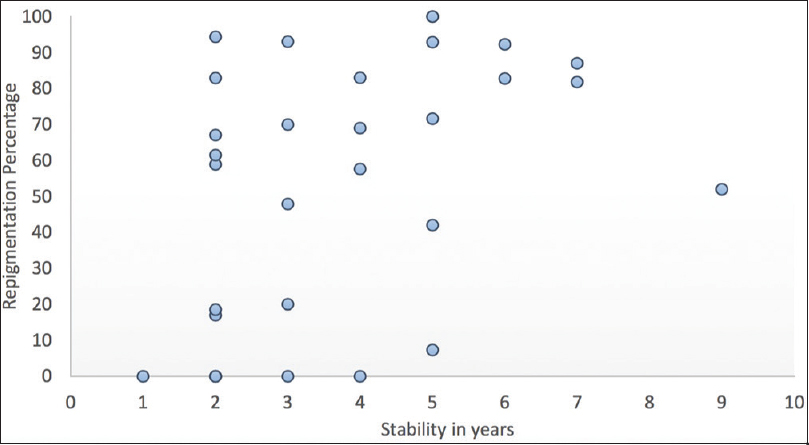 |
| Figure 4: Scatter diagram depicting correlation between re-pigmentation percentage achieved and stability of disease |
Certain sites are considered difficult for re-pigmentation, as either they are technically difficult to operate or are traditionally resistant to most treatment. These sites are elbows, knees, lips, nipples, genitalia, eyelids, palms, toes and fingers. Mulekar et al. demonstrated fair amount of success by noncultured melanocyte-keratinocyte transfer in a study evaluating its efficacy at difficult sites.[17] Our study consisted of two lesions from elbow, one from eyelid and two from lips. The two elbow lesions showed excellent re-pigmentation, eyelid lesion showed good re-pigmentation and the lips showed poor re-pigmentation.
This study is small, and larger studies are needed to ascertain the benefit of Er:YAG for recipient site preparation. Specifically, sites which have uneven surfaces or difficult areas should be compared where it might have an edge over motorized dermabrasion. Although the baseline characteristics of the two groups in our study did not differ significantly [Table - 2], it would have been a better study design if the patients and lesion sites were matched before enrolment into groups. Also, analysis of patient's operative and postoperative comfort, time taken to prepare recipient area, nature of bleeding, postoperative healing, difficulties in specific area, cost of the procedure and surgeon's ease would have been valuable additional variables to compare between the two groups. Comparative studies with other modes of dermabrasion, such as manual dermabrasion, and cryotherapy could also be conducted in order to determine suitability of different modes for different areas.
Conclusion
This study did not reveal any statistically different outcome (in terms of re-pigmentation and adverse effects) between the two methods of recipient site preparation – motorized dermabrasion and Er:YAG ablation. This study is small and larger studies are needed to ascertain the benefit of Er:YAG for recipient site preparation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Krüger C, Schallreuter KU. A review of the worldwide prevalence of vitiligo in children/adolescents and adults. Int J Dermatol 2012;51:1206-12.
[Google Scholar]
|
| 2. |
Gauthier Y, Surleve-Bazeille JE. Autologous grafting with noncultured melanocytes: A simplified method for treatment of depigmented lesions. J Am Acad Dermatol 1992;26:191-4.
[Google Scholar]
|
| 3. |
Olsson MJ, Juhlin L. Leucoderma treated by transplantation of a basal cell layer enriched suspension. Br J Dermatol 1998;138:644-8.
[Google Scholar]
|
| 4. |
van Geel N, Ongenae K, De Mil M, Naeyaert JM. Modified technique of autologous noncultured epidermal cell transplantation for repigmenting vitiligo: A pilot study. Dermatol Surg 2001;27:873-6.
[Google Scholar]
|
| 5. |
Mulekar SV. Melanocyte-keratinocyte cell transplantation for stable vitiligo. Int J Dermatol 2003;42:132-6.
[Google Scholar]
|
| 6. |
Koga M. Epidermal grafting using the tops of suction blisters in the treatment of vitiligo. Arch Dermatol 1988;124:1656-8.
[Google Scholar]
|
| 7. |
Lerner AB, Halaban R, Klaus SN, Moellmann GE. Transplantation of human melanocytes. J Invest Dermatol 1987;89:219-24.
[Google Scholar]
|
| 8. |
Guerra L, Primavera G, Raskovic D, Pellegrini G, Golisano O, Bondanza S, et al. Erbium: YAG laser and cultured epidermis in the surgical therapy of stable vitiligo. Arch Dermatol 2003;139:1303-10.
[Google Scholar]
|
| 9. |
Kaufmann R, Greiner D, Kippenberger S, Bernd A. Grafting of in vitro cultured melanocytes onto laser-ablated lesions in vitiligo. Acta Derm Venereol 1998;78:136-8.
[Google Scholar]
|
| 10. |
Capurro S, Fiallo P. Epidermal disepithelialization by programmed diathermosurgery. Dermatol Surg 1997;23:600-1.
[Google Scholar]
|
| 11. |
Walsh JT Jr., Deutsch TF. Er:YAG laser ablation of tissue: Measurement of ablation rates. Lasers Surg Med 1989;9:327-37.
[Google Scholar]
|
| 12. |
Fioramonti P, Onesti MG, Marchese C, Carella S, Ceccarelli S, Scuderi N, et al. Autologous cultured melanocytes in vitiligo treatment comparison of two techniques to prepare the recipient site: Erbium-doped yttrium aluminum garnet laser versus dermabrasion. Dermatol Surg 2012;38:809-12.
[Google Scholar]
|
| 13. |
Kaufmann R, Hibst R. Pulsed 2.94-microns erbium-YAG laser skin ablation – experimental results and first clinical application. Clin Exp Dermatol 1990;15:389-93.
[Google Scholar]
|
| 14. |
Pianigiani E, Risulo M, Andreassi A, Taddeucci P, Ierardi F, Andreassi L, et al. Autologous epidermal cultures and narrow-band ultraviolet B in the surgical treatment of vitiligo. Dermatol Surg 2005;31:155-9.
[Google Scholar]
|
| 15. |
Taieb A, Alomar A, Böhm M, Dell'anna ML, De Pase A, Eleftheriadou V, et al. Guidelines for the management of vitiligo: The European Dermatology Forum consensus. Br J Dermatol 2013;168:5-19.
[Google Scholar]
|
| 16. |
Rao A, Gupta S, Dinda AK, Sharma A, Sharma VK, Kumar G, et al. Study of clinical, biochemical and immunological factors determining stability of disease in patients with generalized vitiligo undergoing melanocyte transplantation. Br J Dermatol 2012;166:1230-6.
[Google Scholar]
|
| 17. |
Mulekar SV, Al Issa A, Al Eisa A. Treatment of vitiligo on difficult-to-treat sites using autologous noncultured cellular grafting. Dermatol Surg 2009;35:66-71.
[Google Scholar]
|
Fulltext Views
6,296
PDF downloads
3,757





