Translate this page into:
Basal cell carcinoma developing in verrucous epidermal nevus
2 Department of Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Amrinder J Kanwar
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh - 160 012
India
| How to cite this article: De D, Kanwar AJ, Radotra BD. Basal cell carcinoma developing in verrucous epidermal nevus. Indian J Dermatol Venereol Leprol 2007;73:127-128 |
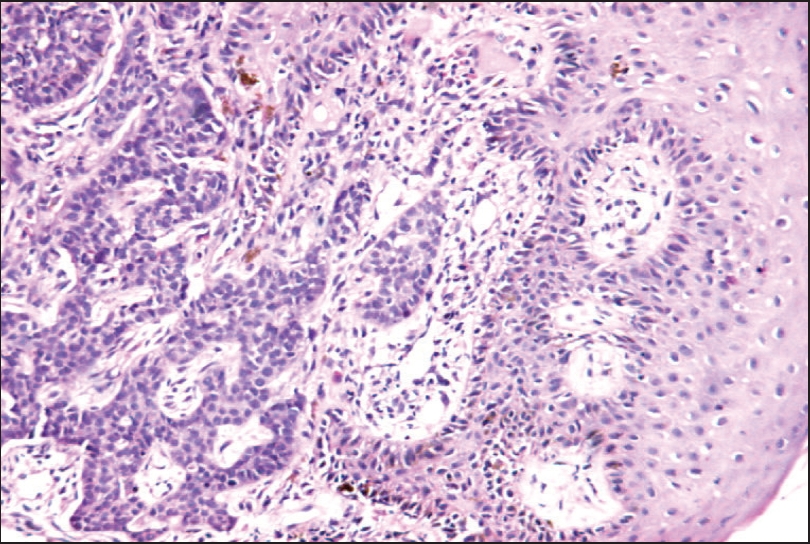 |
| Masses of basaloid cells in infi ltrative pattern (H an E, x200) |
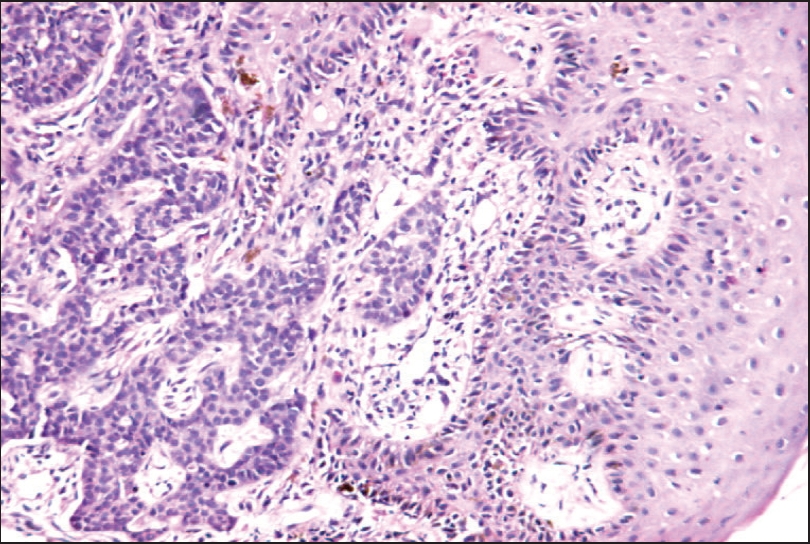 |
| Masses of basaloid cells in infi ltrative pattern (H an E, x200) |
 |
| Noduloulcerative basal cell carcinoma in verrucous epidermal nevus |
 |
| Noduloulcerative basal cell carcinoma in verrucous epidermal nevus |
Sir,
Epidermal nevi increase slowly in size during childhood and become stationary at puberty. [1] Both basal cell and squamous cell carcinomas have been reported to develop in an epidermal nevus; these are however extremely rare. [2],[3],[4],[5] Malignant transformation should be suspected when sudden localized development of nodules or ulcer appears.
A 58-year-old farmer presented to us with hyperpigmented (dark brown) soft verrucous plaque on the right temporoparietal region since birth. The present size was attained around puberty. The lesion had been asymptomatic till eight months back when a nodule appeared on the plaque; it developed central ulceration with pain, bleeding and crusting. Examination revealed multiple dark brown soft verrucous papules coalescing into a plaque disposed in a linear distribution over the right temporoparietal area extending up to the right pre-auricular area. There was single well-defined ulcer (6x6 cm) with a regular outline, elevated rolled edge and a firm base with crusting and bleeding in a few areas [Figure - 1]. It was not fixed and there was no local lymphadenopathy. A diagnosis of basal cell carcinoma arising in a verrucous epidermal nevus was made. Biopsy from the margin of the ulcer revealed basaloid tumor with cells arranged in an infiltrative pattern with retraction spaces [Figure - 2]. Mild pleomorphism, hyperchromatosis, inconspicuous nucleoli and scanty cytoplasm were also noted. Focal keratin pearls, desmoplastic reaction and myxoid change could also be seen. Sebaceous glands were scanty. These findings were suggestive of basal cell carcinoma (BCC).
The lesion was excised with a free margin of 5 mm and the defect was closed with a flap.
Epidermal nevi are hamartomatous lesions arising from the embryonic ectoderm; their incidence is estimated to be one in 1000 live births. [1] Malignant changes in a verrucous epidermal nevus is extremely uncommon.
It is interesting to note that the risk of developing BCC in a nevus sebaceous, another type of epidermal nevus is relatively higher (6.5-50%), [6] compared to the commoner verrucous epidermal nevus. This is in spite of the fact that both arise from pluripotent primary epithelial germ cells which have the capacity to differentiate to different epithelial structures.
To the best of our knowledge, this is the first report of its kind from India where a malignant change in a verrucous epidermal nevus has been described.
| 1. |
Solomon LM, Esterly MB. Epidermal and other congenital organoid nevi. Curr Probl Pediatr 1975;6:1-56.
[Google Scholar]
|
| 2. |
Cramer SF, Mandel MA, Hauler R, Lever WF, Jenson AB. Squamous cell carcinoma arising in a linear epidermal nevus. Arch Dermatol 1981;117:222-4.
[Google Scholar]
|
| 3. |
Horn MS, Sausker WF, Pierson DL. Basal cell epithelioma arising in a linear epidermal nevus. Arch Dermatol 1981;117:247.
[Google Scholar]
|
| 4. |
Goldebrg HS. Basal cell epitheliomas developing in a localized linear epidermal nevus. Cutis 1980;25:295-7,299.
[Google Scholar]
|
| 5. |
Ichikawa T, Saiki M, Kaneko M, Saida T. Squamous cell carcinoma arising in a verrucous epidermal nevus. Dermatology 1996;193:135-8.
[Google Scholar]
|
| 6. |
Chun K, Vazcuez M, Sanchez JL. Nevus sebaceous: Clinical outcome and considerations for prophylactic excision. Int J Dermatol 1995;34:538-41.
[Google Scholar]
|
Fulltext Views
3,433
PDF downloads
2,771





